The Indian government announced a nationwide lockdown as a preventive measure to control the prevailing COVID-19 pandemic. This survey was developed and conducted to assess the impact of lockdown on Indian optometry practice.
MethodsA survey questionnaire was designed and circulated across the optometrists practicing in India through multiple social media platforms. All the data were extracted and only valid response were analyzed and reported.
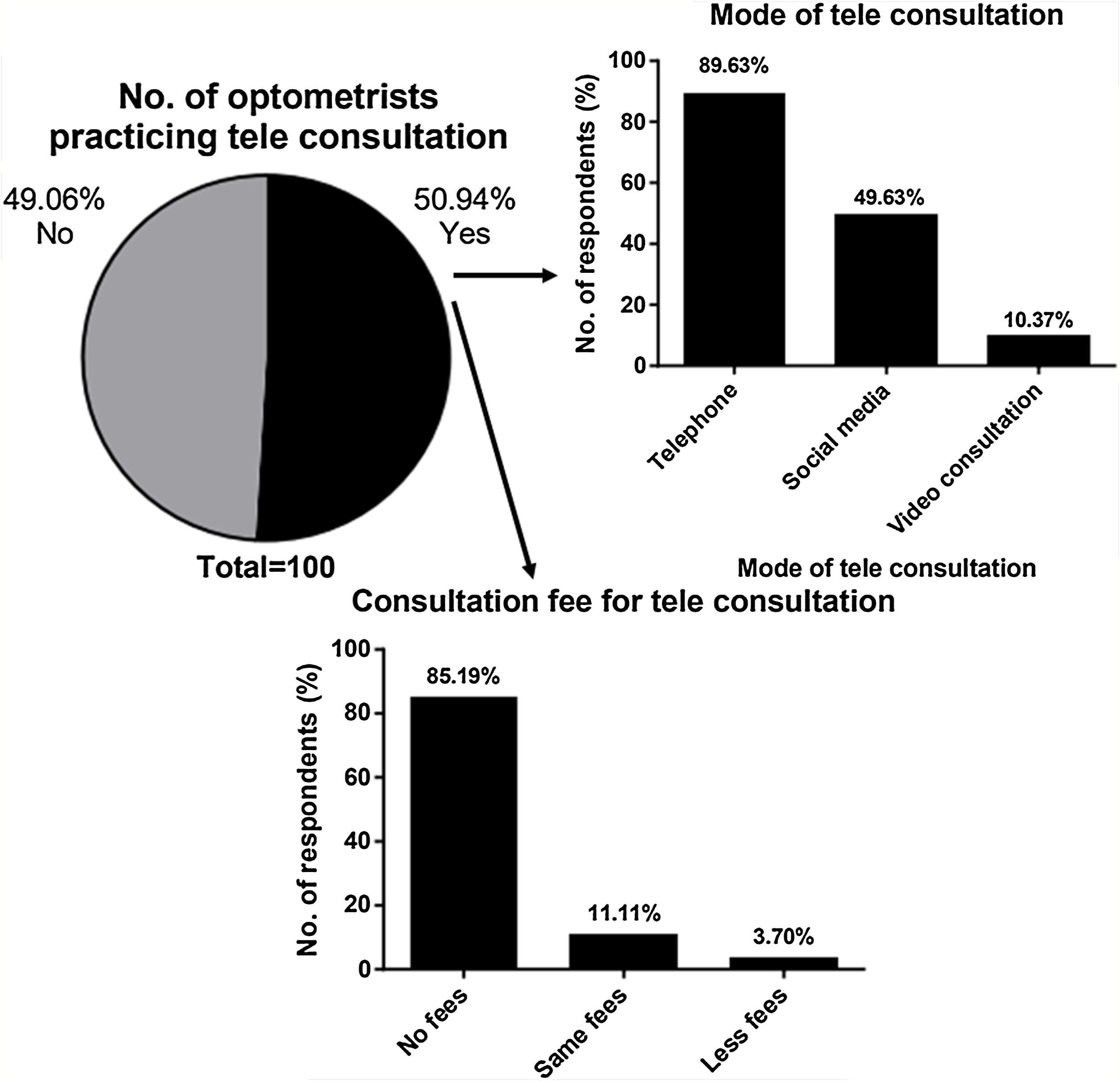
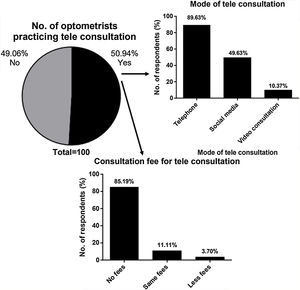
ResultsA total of 691 optometrists participated in the survey. Most of the participants (22.25%) were in private practice followed by academics (14.89%). Among the valid responses collected, it was found that 43.37% of the respondents were consulting patients during the lockdown. Of these, 27.17% of optometrists were examining infectious cases and 48.68% were examining all the patients who came for consultation. Approximately 50.94% of the participated optometrist had begun telephonic/e‑mail/video consultations. In addition, 64.48% reported that optometrists were at an equal risk of clinching COVID‑19 on comparison with other domains during patient examination. Nearly 30.44% respondents felt that optometrists would face challenges in approaching the patient post COVID-19 considering the close working distance.
ConclusionA proportion of optometrist have switched to some form of teleconsultation in order to aid patients during this prevailing pandemic. Regulatory bodies should issue appropriate guidelines regarding the safe optometry practice for the betterment of both patient and practitioners during face-to-face consultation.
Toward the end of 2019, a cluster of people presented with signs related to pneumonia in the Wuhan a city in China, which was later identified to be novel coronavirus disease 2019 (COVID-19).1,2 After initial diagnosis of this novel disease, there was an alarming increase in the rate of COVID-19 cases in China, and by early 2020 WHO (World Health Organization) declared this COVID‑19 outburst as a pandemic. The first case of COVID-19 in India was noted in Kerala on 30th January 2020.
COVID‑19 manifests flulike ailment with fatigue, sore throat, fever, cough, dyspnoea, occasional diarrhea and vomiting.3 Literature suggests that old age and the presence of comorbidities could result in poor prognosis of the condition. In older age group and immune-compromised individuals, the condition is found to deteriorate to acute respiratory distress syndrome and multi‑organ failure, leading to death.3–5
WHO had notified that the transmission could primarily occur through contacts, droplets, and fomites.4,5 Considering this, many countries including India have announced a complete lockdown as a preventive measure to constrain the spread.2,3 Indian government imposed a nation-wide lockdown of all non-essential services for 21 days from 25th March 2020, and on 14th April 2020, the lockdown got extended further for 19 days till 3rd May 2020. General guidelines proposed by the national and international organizations might not be directly applicable to India and to eye-care professionals in particular. In addition, few guidelines released by health ministries of different states, lead to confusion and panic among eye-care practitioners.6–8
As a result of the pandemic, many hospitals and clinics pulled themselves off from offering service. The closure of outpatient departments has decreased the accessibility to health care.3,6
Optometrists are primary eye-care professionals who delivers patient care and dispense optical devices such as spectacles, contact lens, and low-vision devices. Many optometrists across India have closed their practice for non-essential services during the lockdown. Owing to the prevailing pandemic, optometrists have been challenged with issues pertaining to patient care, manufacturing and dispensing optical devices, maintaining business stability, and control of infection.9 This survey aimed at assessing the impact of COVID-19 lockdown on optometry education and care of sick, highlighting the modes of teaching and patient consultation.
MethodsA cross-sectional online survey questionnaire was administered in accordance with the Declaration of Helsinki.10 The aim of this survey was to evaluate the optometrist practice pattern and patient care during the COVID-19 lockdown. As this study aimed to collect only the perception and the service by the optometrists, ethics approval was not obtained. The information collected did not include personal information and was anonymized, which was similar to surveys carried out by Nilesh et al.11 and Nair et al.3
The survey questionnaire (Google form) was structured and finalized after a group discussion with four optometrists. The structured questionnaire was circulated among optometrists practicing in India through social medias, namely WhatsApp, Telegram, and Facebook. The survey responses were collected from April 24, 2020, to April 29, 2020. A reminder was sent every 2 days via social media platforms. In the online survey, respondents could not alter responses after submitting the questionnaire.
The survey consisted of a 15-item questionnaire (Appendix Table 1) focusing on different optometry practices, mode of education, and patient care in India during the COVID-19 lockdown. A team of five optometrist piloted the questionnaire initially to check the clarity and to assess the time required to complete the survey.12 Minor corrections to the questionnaire were made based on their feedback. The estimated time to completion of this questionnaire was approximately 2–3 min. At the beginning of the survey, a written statement indicated that the participation is voluntary and their response to the survey implies their consent for participation. The statement also mentioned that the questionnaire was to be completed only by the optometrist practicing in India.
As the optometry profession in India is not regulated,13 to filter out the responses from practitioners who had completed short-term courses, one item in the questionnaire requested the responder to fill their highest educational qualification in optometry. Further to filter responses from undergraduate and diploma students, an option “Diploma/Bachelors student” was added. One item in the questionnaire requested the responder to provide information about their previous participation in the survey to avoid multiple response from the same responder.14
Sample sizeThe sample size calculated15 was 593, considering approximately 49,000 Indian optometrists13 and 4% margin of error with 95% confidence interval.
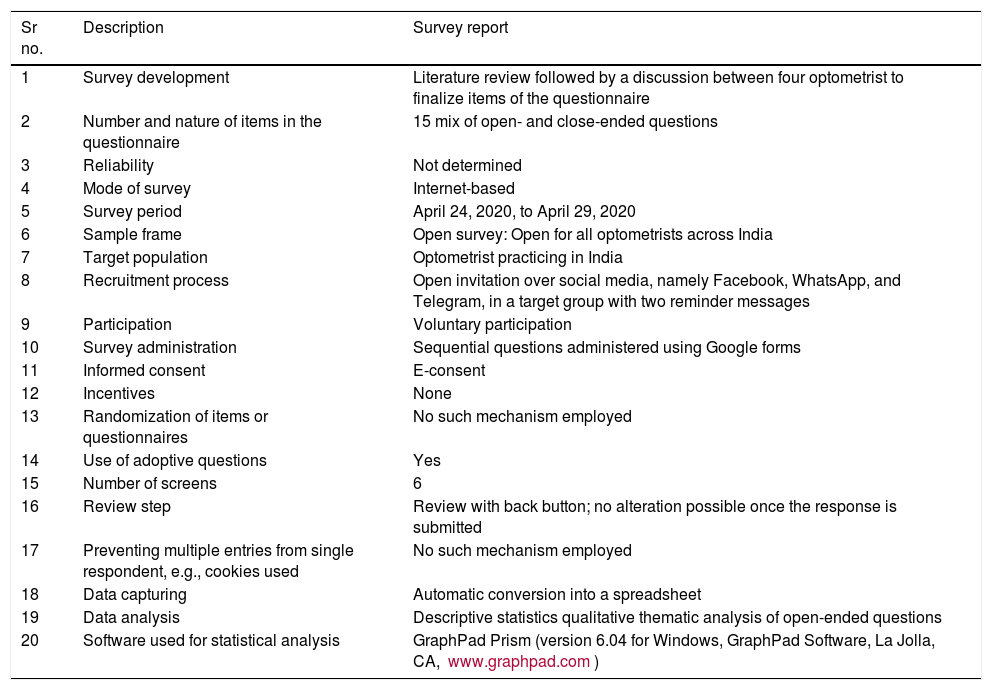
Data analysisThe analysis was conducted and graphs were generated using GraphPad Prism (version 6.04 for Windows; GraphPad Software, La Jolla, CA). The proportion of each response was calculated. The Checklist for Reporting Results of Internet E-Surveys (CHERRIES) guidelines were used to prepare the survey16 (Table 1).
Summary of the methodology followed in the survey.
| Sr no. | Description | Survey report |
|---|---|---|
| 1 | Survey development | Literature review followed by a discussion between four optometrist to finalize items of the questionnaire |
| 2 | Number and nature of items in the questionnaire | 15 mix of open- and close-ended questions |
| 3 | Reliability | Not determined |
| 4 | Mode of survey | Internet-based |
| 5 | Survey period | April 24, 2020, to April 29, 2020 |
| 6 | Sample frame | Open survey: Open for all optometrists across India |
| 7 | Target population | Optometrist practicing in India |
| 8 | Recruitment process | Open invitation over social media, namely Facebook, WhatsApp, and Telegram, in a target group with two reminder messages |
| 9 | Participation | Voluntary participation |
| 10 | Survey administration | Sequential questions administered using Google forms |
| 11 | Informed consent | E-consent |
| 12 | Incentives | None |
| 13 | Randomization of items or questionnaires | No such mechanism employed |
| 14 | Use of adoptive questions | Yes |
| 15 | Number of screens | 6 |
| 16 | Review step | Review with back button; no alteration possible once the response is submitted |
| 17 | Preventing multiple entries from single respondent, e.g., cookies used | No such mechanism employed |
| 18 | Data capturing | Automatic conversion into a spreadsheet |
| 19 | Data analysis | Descriptive statistics qualitative thematic analysis of open-ended questions |
| 20 | Software used for statistical analysis | GraphPad Prism (version 6.04 for Windows, GraphPad Software, La Jolla, CA, www.graphpad.com) |
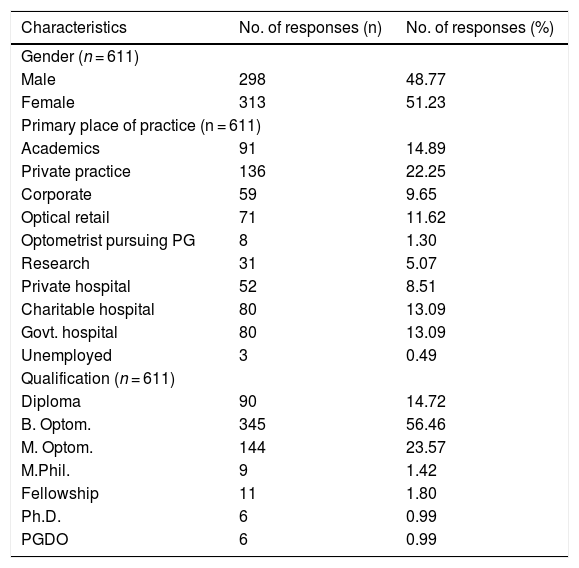
Survey response was received from 691 optometrists. Of which, data from only 611 were valid and were included for the analysis. Data were excluded from 11 undergraduate/diploma students, 1 optometrist practicing outside India, 14 technicians with short-term courses, 33 respondents who had reported to have responded the survey before, and 21 respondents with logical contradictions (e.g., those who answered that they were not practicing any kind of teleconsultation had also responded that they are charging for teleconsultation). Among the included respondents, 51.23% were female and 48.77% were male. The characteristics of the respondents are mentioned in Table 2.
Summary of the demographics of the optometrists involved in the survey.
| Characteristics | No. of responses (n) | No. of responses (%) |
|---|---|---|
| Gender (n = 611) | ||
| Male | 298 | 48.77 |
| Female | 313 | 51.23 |
| Primary place of practice (n = 611) | ||
| Academics | 91 | 14.89 |
| Private practice | 136 | 22.25 |
| Corporate | 59 | 9.65 |
| Optical retail | 71 | 11.62 |
| Optometrist pursuing PG | 8 | 1.30 |
| Research | 31 | 5.07 |
| Private hospital | 52 | 8.51 |
| Charitable hospital | 80 | 13.09 |
| Govt. hospital | 80 | 13.09 |
| Unemployed | 3 | 0.49 |
| Qualification (n = 611) | ||
| Diploma | 90 | 14.72 |
| B. Optom. | 345 | 56.46 |
| M. Optom. | 144 | 23.57 |
| M.Phil. | 9 | 1.42 |
| Fellowship | 11 | 1.80 |
| Ph.D. | 6 | 0.99 |
| PGDO | 6 | 0.99 |
PG, postgraduate.
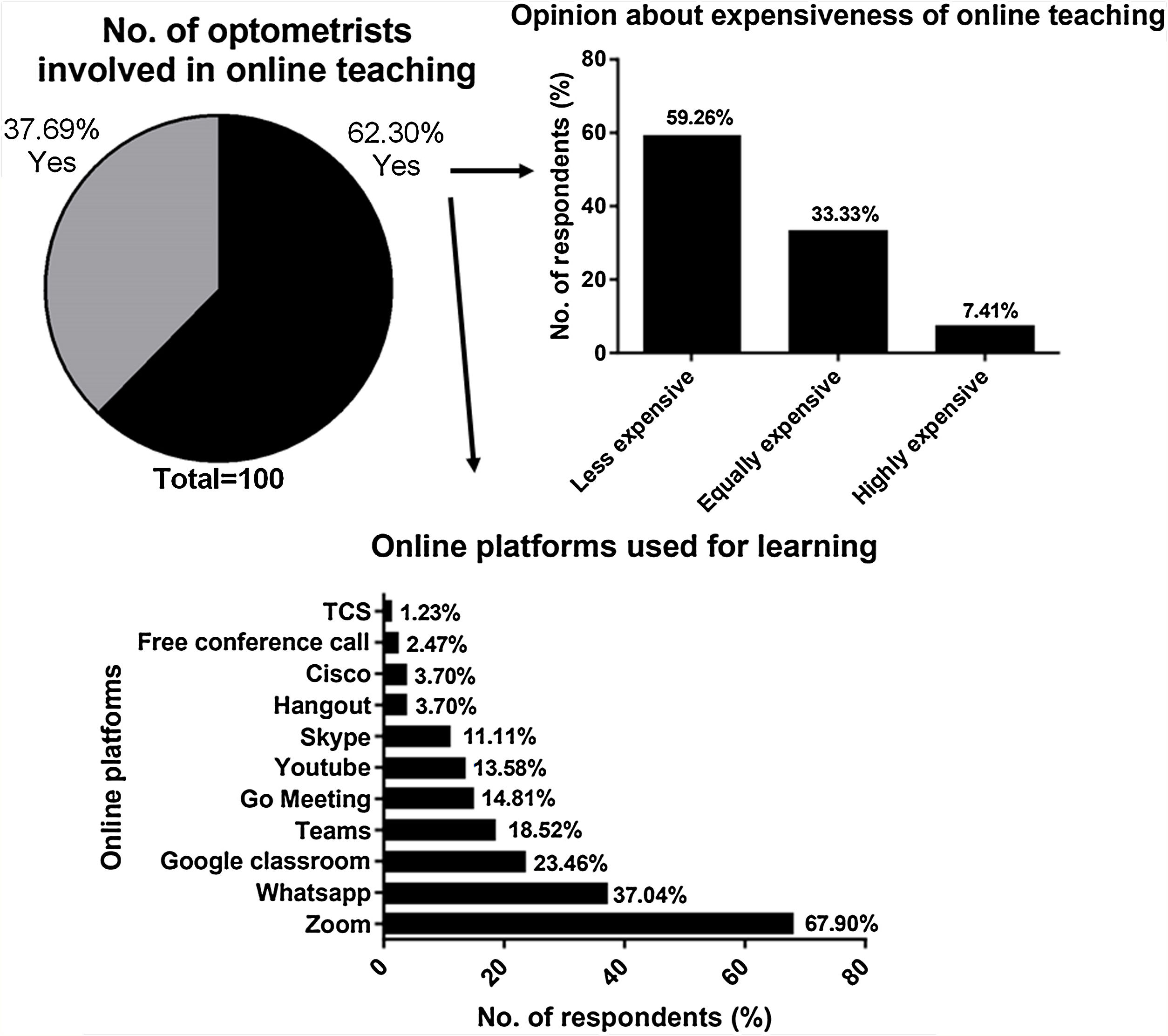
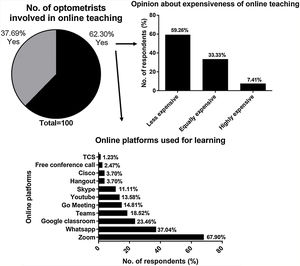
Of the respondents who nominated to be primarily involved in academics, research, and higher education, 62.30% were involved in online teaching. Modes used for online teaching are shown in Fig. 1.
Respondents involved in taking online classes were asked about the expenses involved in taking online classes compared to normal offline teaching. However, 59.26% said that online teaching was less expensive, 7.41% felt it to be more expensive, and 33.33% reported to be equally expensive.
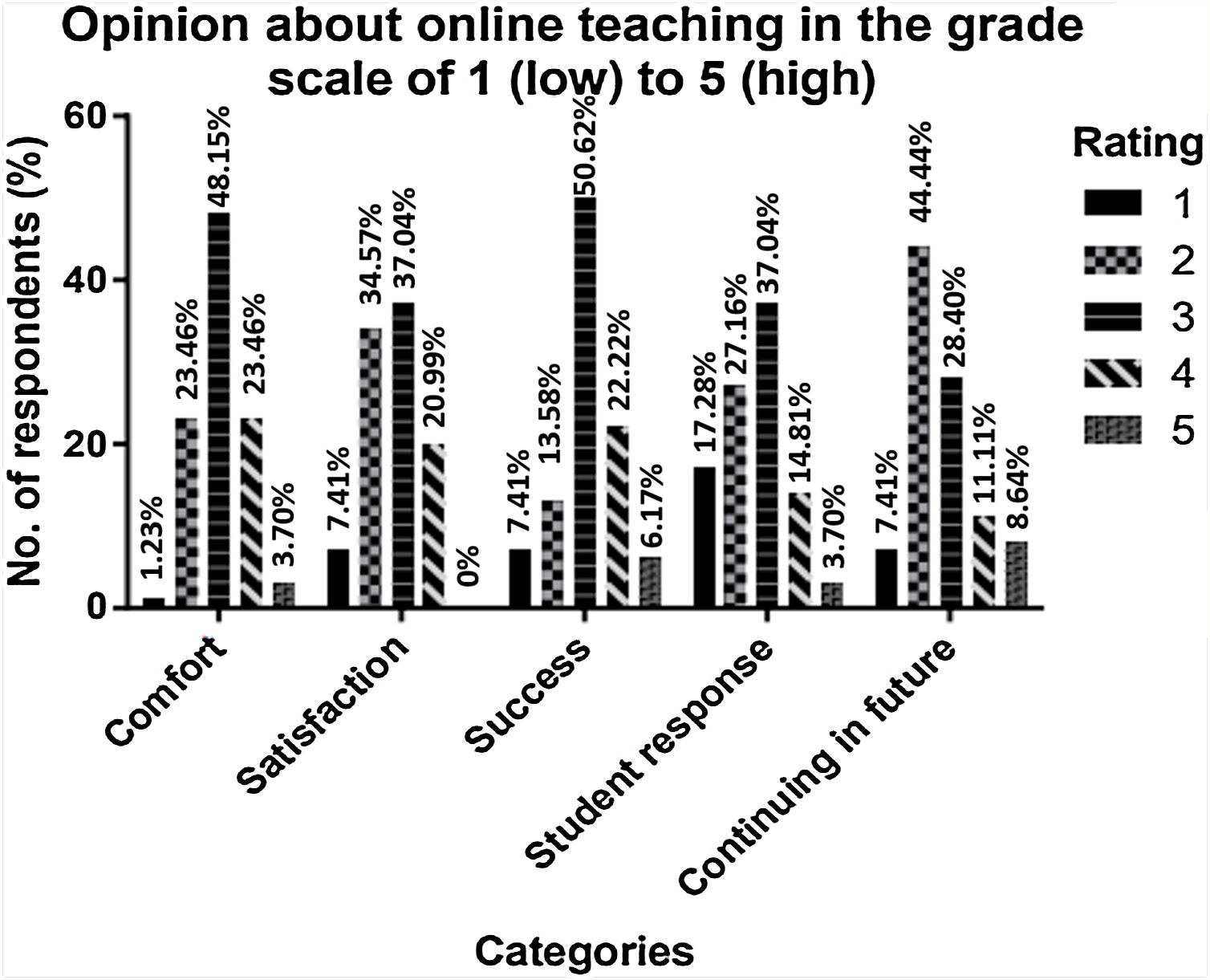
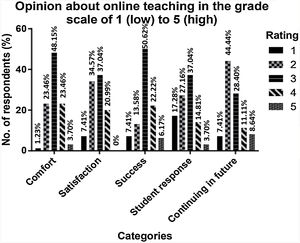
The results of five-point Likert scale accessing comfort, satisfaction, successfulness, the response of students, and their preference in continuing online classes are shown in Fig. 2.
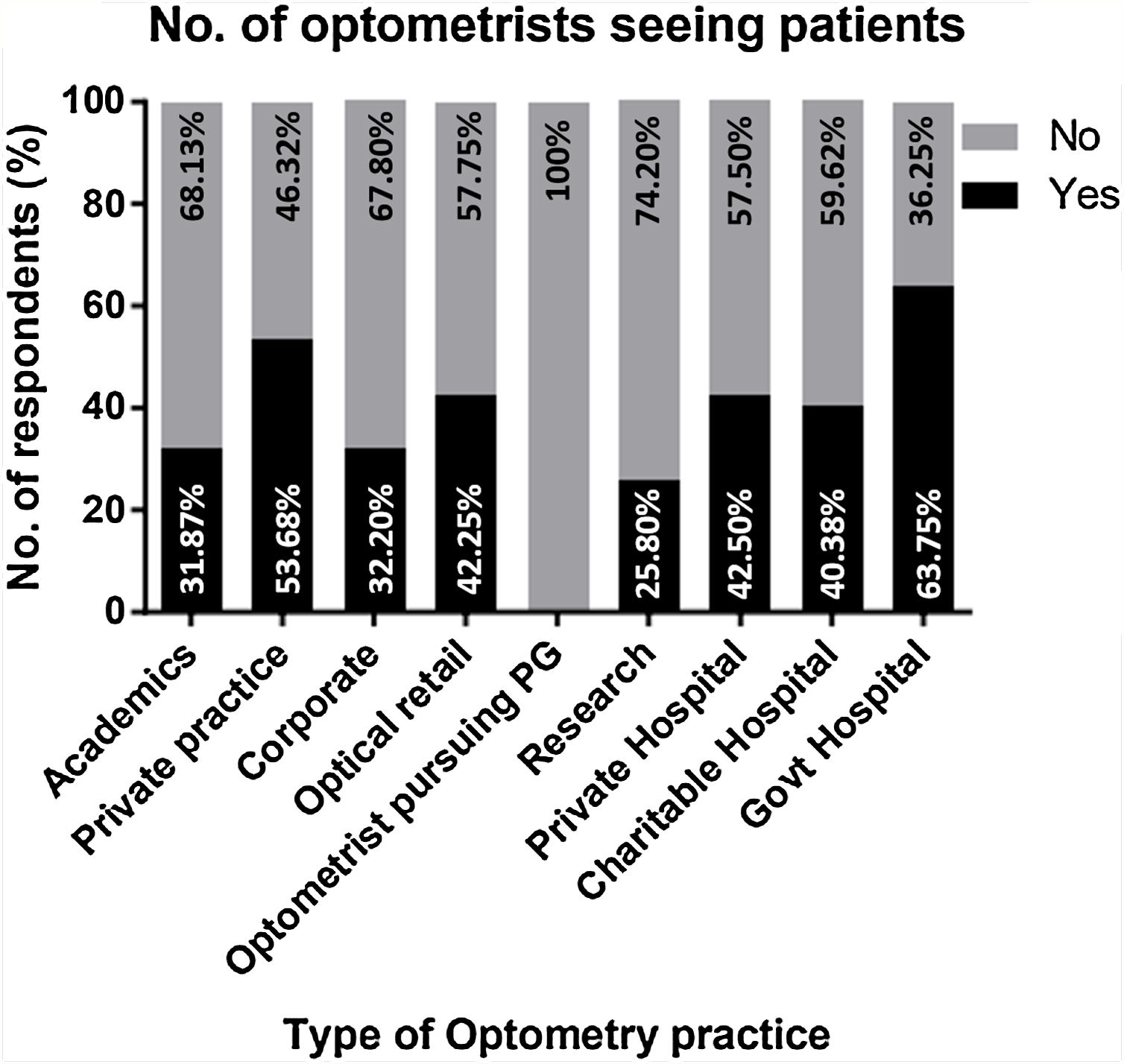
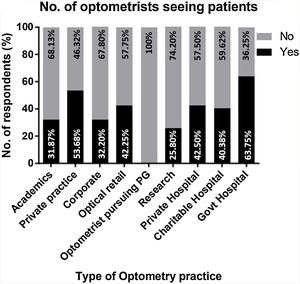
Clinical practiceOf the total optometrists responded, 43.37% were involved in consulting patients during the lockdown either in hospitals or through teleconsultation. Fig. 3 shows the number of optometrists engaged in consultation from their primary mode/place of practice.
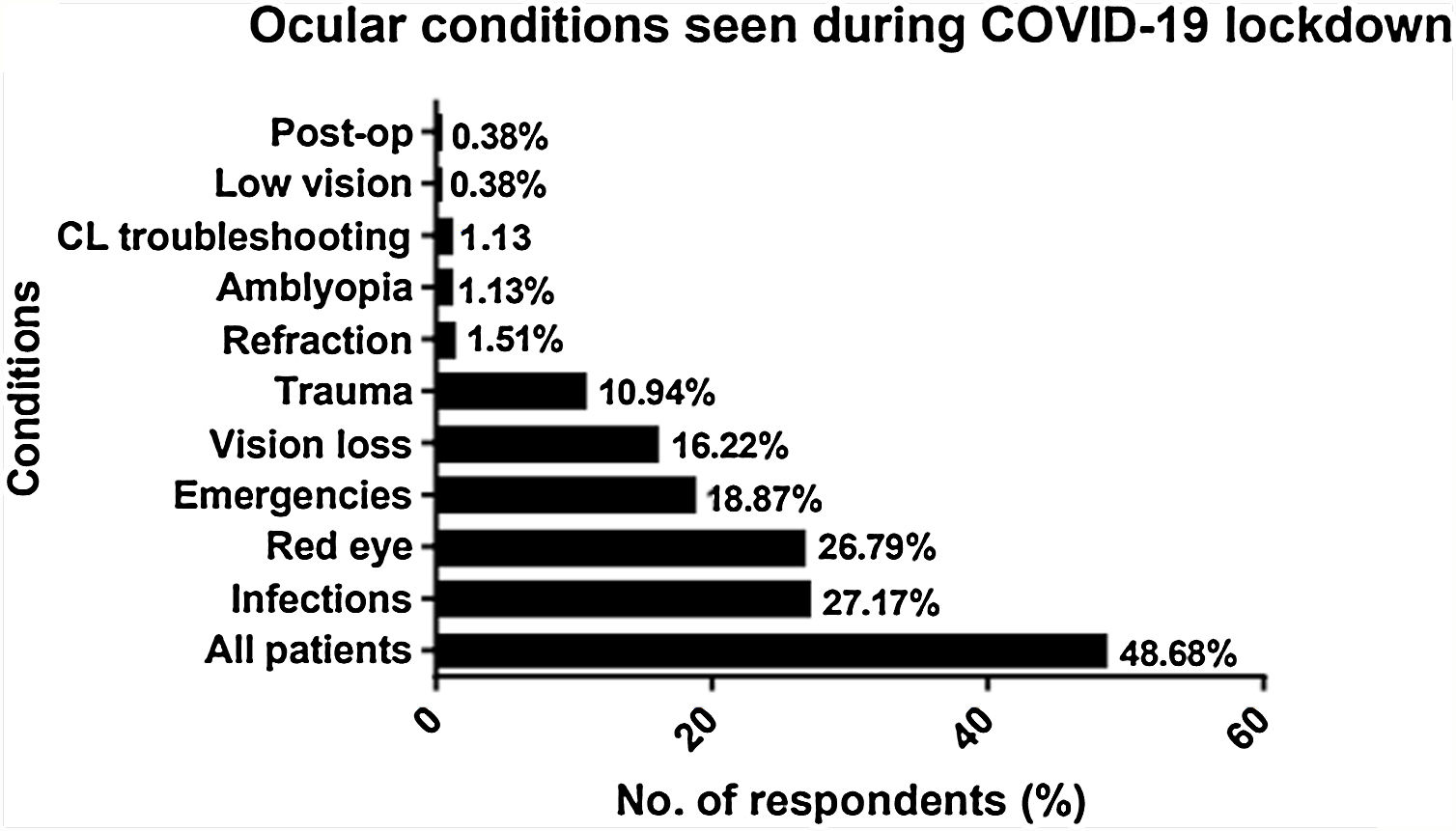
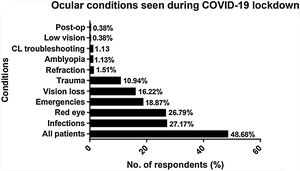
Optometrists who were currently involved in consulting patients were asked to mention the type of patient or the conditions they were consulting. Infections were the most commonly consulted by 27.17%, followed by red eye seen by 26.79%, and emergency cases by 18.87% optometrists. Furthermore, 48.68% optometrists reported that they were consulting all patients coming to them (Fig. 4).
The respondents were questioned for their exploration and initiation on other avenues for attending patients such as teleconsultation. For such initiatives, 50.94% responded positively (Fig. 5). In contrast, 18.87% of the clinicians said that they were favorably considering the prospective idea of starting such initiative, whereas 30.19% of the clinicians reported to have no plans in starting any such consultations. Among those who were involved in teleconsultation, 85.19% did not charge any professional fees from patients; 11.11% reported that were charging the consultation as they normally charge for an physical consultation; and 3.7% collected less professional charges than that for an in‑person consultation. Interestingly, none of the respondents reported charging higher consultation fee than usual.
Lockdown: challenges and current scenarioIt was found that 75.94% optometrists were involved in attending online seminars and webinars. All the optometrists who participated in the study were questioned for their perceptions of the risk of contracting COVID-19 while examining patients. About 22.59% felt that risk of contracting COVID‑19 is high for optometrists; 12.93% and 64.48% felt to have lower and equal risk, respectively.
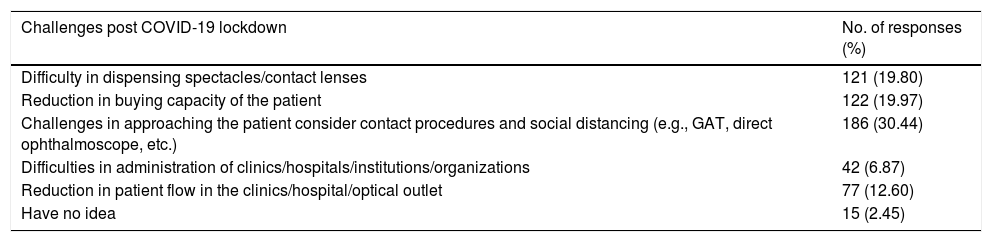
The last part of the survey focused on accessing optometrists’ opinion on challenges they will be facing during their practice post-COVID-19 lockdowns (Table 3).
Table showing the potential challenges for optometrist during COVID-19 lockdown.
| Challenges post COVID-19 lockdown | No. of responses (%) |
|---|---|
| Difficulty in dispensing spectacles/contact lenses | 121 (19.80) |
| Reduction in buying capacity of the patient | 122 (19.97) |
| Challenges in approaching the patient consider contact procedures and social distancing (e.g., GAT, direct ophthalmoscope, etc.) | 186 (30.44) |
| Difficulties in administration of clinics/hospitals/institutions/organizations | 42 (6.87) |
| Reduction in patient flow in the clinics/hospital/optical outlet | 77 (12.60) |
| Have no idea | 15 (2.45) |
GAT, Goldmann applanation tonometer.
Our survey revealed that a greater part of the optometry practice was hampered during the pandemic. During pandemic, although optometrists may be available, the unavailability of other support personnel may cause operational and logistical challenges for continuing a health-care facility. It was noted that 43.37% of the optometrists were involved in consulting the patients.
Optometrists were selective in consulting patient. Infectious conditions, redness, and emergencies were the most commonly consulted cases. Interestingly, 48.68% of respondents involved in consulting stated that they were consulting all patients those who came seeking consultation.
As there are no given guidelines to optometric practice in India during the lockdown,6 the usage of personal protective equipment and precautionary methods followed during examining the patient is questionable. Considering closer working distance while examining patients, optometrists found themselves to be at equal or high risk of getting infected by COVID-19, which in accordance with the results of the survey shown by Nair et al.3
Optometry is the first face of interaction concerning eye care; and eye clinic is an environment with high‑risk for both the examiner and the patient, and the eye-care practitioner need to understand the risk factors associated with it.
Ocular infection cases were the most common condition that was being examined by 72 (27.17%) optometrists. The ocular implications of the severe acute respiratory syndrome coronavirus 2 (SARS‑CoV‑2) are clearly established and the literature reports ocular surfaces are more prone for SARS‑CoV‑2 invasion.17–19
It is also reported in the literatures that, patients with no conjunctivitis tested positive for SARD-CoV-2 nucleic acid in conjunctival sac swabs.20 Virus can enter respiratory track through nasolacrimal ducts via tears droplets.20 Though the reported studies suggested ocular transmission a low risk,21,22 it is also known that one‑third of the COVID‑19 positive patients had ocular implications such as chemosis, epiphora, and conjunctival hyperemia, and it is possible to transmit via eyes.23 To reduce infection post lockdown, prevention at the level of primary eye care is vital.
Prevention at primary eye care settingIn this survey, 30.44% respondents mentioned that there are challenges on approaching a patient considering contact procedures and social distancing. Health-care setting provides an favorable environment for virus to spread from person to person or from lifeless objects in shared areas such as waiting hall and examination rooms.9 Measures to forestall the infection include social distancing, use of protective equipment, and hygiene/infection control procedures.7
Typical COVID-19 virus can survive for up to 72 h.24 Sanitizing work place and other areas where patients might touch (e.g., door handle) is an effective way to forestall the spread of infectious agents.9 Frequent hand washing with alcohol-based sanitizers after patient contact effectively reduces the spread of any infectious material.25
A simple mnemonic “MASKS” strategy, developed by Hogg and Houston,26 can be used as a necessary precaution for outpatient setting: “M—masks for patients with cough and fever and providers examining those patients; A—alcohol gel for sanitation (for patients as well as office staff); S—seating of potentially infectious individuals apart from others (recommended distance at least 1 m); and K—kleening (disinfecting) hard surfaces; S—signs to guide patients and staff (e.g., to promote handwashing)”. The estimated implementation cost such methods in a typical clinical setting that attends 30 patients/day is $2 per day.
TeleconsultationIt was interesting to know that almost 50.94% of respondents were involved in providing patient care through teleconsultation. Teleconsultation can be used as an effective means for providing patient care by avoiding in-clinic direct contact. Teleconsultation can be performed through different means that include telephone consultations, monitoring with mobile phone-based applications, and remote consultations with specialists by electronic data transfer.9,27 However, advanced technology is not the only mode of improving teleconsultation; revamp in history taking through the use of validated questionnaires or adapting patient-reported outcome measures may enhance patient care.27 There are a few other vision-related applications that show promising outcomes, for example, for the assessment of contrast sensitivity,28 manifest and latent deviations,29 and visual field screening.30–32 At the same time, the majority remain unvalidated for clinical use.33 The potential for estimating visual acuity and refractive error utilizing handheld electronic gadgets is growing in the area of research.31 A study on web-based refraction in adult population (aged 18–40 years) showed good agreement with customary subjective refraction.27,34,35 For several years, teleconsultation in eye care has demonstrated to be a useful, valid, and cost-effective method in managing the eye diseases.9,36–38 In the setting of social distancing, sending clinical data electronically to an eye care specialist for online consultation could reduce the need for patients to visit another public gathering place (e.g., hospitals and clinics) and in turn may forestall patients’ exposure to contagious individuals.9 In addition to validated and well-researched tools, usability, medico-legal implications, and practitioner opinions are likely to influence the usage of teleconsultation.
Business interruption and recoveryAmong the respondents, 22.25% were having their own independent practice, which was similar to practice during normal days.11 Among the private practitioners, 46.32% were under total lockdown, which could create economic damage on a small business due to absence of staff, interrupted utilities, or consumer fear. A study has shown that two-thirds of businesses will file bankruptcy within a year, if they do not resume the business within two weeks after a disaster.39
The aftereffect of business by acute natural disasters includes problems such as customer accessibility, absence of employee, and shipping delays, which tender to business losses and impede recovery. On chance if particular regions are set apart as zones of higher danger, difficulties to recuperation become magnified.40 Providers of services and goods whose markets are restricted to a local level (e.g., optometrists) are more helpless against delays in long-term recuperation after a disaster.9,41
Providers of services or goods must be prepared for disruption in the typical progression of trade. Businesses that prepare for emergencies beforehand in general endure and resume typical activities in a superior way than those that don't.9,41 The study by Hom et al.9 summarized 10 business planning methods, namely the preparation of getting organized, risk assessment, employee health, employee policies, supply and service interruptions, pandemic and management plan, prepare to fill vacancies, plans for business continuity, inform/education of employees, and informing other stakeholders.
Academic practiceAmong the optometrists with academic and research background, 62.30% were found to be involved in taking the class online using various modes. The results suggest that a higher number of educators have quickly adopted online classes, suggesting the need for development of devoted online modules explicit to characterized territories of competency alongside definite arranging of blended learning exercises.42 Though literature suggests that there is a significant increase in scoring lower grades among students compared to face-to-face classes, motivating and continuous interaction with the students during online classes may improve grades.43–45
The lockdown, which was a first in India, brought many ambiguities in both personal and professional fronts for most health-care practitioners. The rapidly‑evolving scenario made it challenging to have a detailed survey on practice, usage of personal protective equipment, and adherence to guidelines. Thus, the duration for the survey completion was kept short.
ConclusionCOVID-19 pandemic will have an impact on optometry practice henceforth. Changes in the clinical management policy such as planning timely appointments, dynamic screening, accelerated consults for sick patients, patient health-care declarations, and other waiting room guidelines may turn out to be a part of the routine clinical practice in the future. Other reasonable changes include, employee and environmental protection measures to forestall disease transmission.46 In future some new proof will develop, changing the prevention and treatment modalities for COVID‑19. From the perspective of eye-care practitioners, it is challenging to put on restrictions in the workplace. But for the eye-care practitioners to return to serving society optimally and securely, the regulatory bodies should provide some clear guidelines in order to resume patient care without trading off wellbeing of both the practitioners and their patients.
Author contributionSKK – Involved in study conception and design, data acquisition, drafting, critical revising and final approval of the manuscript.
PN - Involved in study design, data acquisition, data analysis, drafting and critically revising the manuscript.
VSR - Involved in study design, data acquisition, data analysis, drafting and critically revising the manuscript.
AN - Involved in study design, data acquisition and drafting the manuscript.
Source(s) of supportNil.
Presentation at a meetingNil.
Conflicting interestThe authors have no conflicts of interest to declare.
We would like to thank Mr. Kumaran, General Secretary, Optometric Association of Tamil Nanbargal (OATN) and Karthikeyan K, Chairman, Tamil Nadu Government Optometry professionals Association and Vice President, National Ophthalmic Association for helping us in circulating the questionnaire with the optometrist in national and state associations.