To evaluate the association between visual symptoms and use of digital devices considering the presence of visual dysfunctions.
MethodsAn optometric examination was conducted in a clinical sample of 346 patients to diagnose any type of visual anomaly. Visual symptoms were collected using the validated SQVD questionnaire. A threshold of 6 hours per day was used to quantify the effects of digital device usage and patients were divided into two groups: under and above of 35 years old. A multivariate logistic regression was employed to investigate the association between digital device use and symptoms, with visual dysfunctions considered as a confounding variable. Crude and the adjusted odds ratio (OR) were calculated for each variable.
Results57.02 % of the subjects reported visual symptoms, and 65.02% exhibited some form of visual dysfunction. For patients under 35 years old, an association was found between having visual symptoms and digital device use (OR = 2.10, p = 0.01). However, after adjusting for visual dysfunctions, this association disappeared (OR = 1.44, p = 0.27) and the association was instead between symptoms and refractive dysfunction (OR = 6.52, p < 0.001), accommodative (OR = 10.47, p < 0.001), binocular (OR = 6.68, p < 0.001) and accommodative plus binocular dysfunctions (OR = 46.84, p < 0.001). Among patients over 35 years old, no association was found between symptoms and the use of digital devices (OR = 1.27, p = 0.49) but there was an association between symptoms and refractive dysfunction (OR = 3.54, p = 0.001).
ConclusionsVisual symptoms are not dependent on the duration of digital device use but rather on the presence of any type of visual dysfunction: refractive, accommodative and/or binocular one, which should be diagnosed.
In recent years, there has been a growing trend in the extended use of near vision, either for studying, particularly among young individuals, or for employment in occupations that align with modern demands of society. Technology is increasingly being used to facilitate the development of both educational and professional activities. Most of this technology refers to digital devices such as computers, smartphones or tablets.1 These devices are very common in today's society, being easily accessible from an early age and suitable for individuals of all age groups. In this sense, several studies have shown that an abusive use of all these devices could cause the appearance of symptoms.1-8 Accordingly, it is reasonable to hypothesize that any existing visual dysfunction (such as refractive, accommodative or binocular dysfunction) in a patient might influence or exacerbate the manifestation of this symptomatology.
Uncorrected refractive errors have been related to numerous symptoms during near tasks and their prevalence is significant when considering the presence of symptoms.9 Likewise, to maintain a clear and single image during near work activities, both the accommodative and convergence systems must function properly. If either of these systems fails, resulting in accommodative and/or vergence dysfunctions (also known as general binocular dysfunctions), subjects may complain of symptoms.10 Several studies have shown that general binocular dysfunctions are commonly found in clinical practice, and although there is considerable disparity in their reported prevalence based on scientific evidence,11 there are different symptoms associated with these anomalies.10-13 A systematic review by García-Muñoz et al.14 demonstrates the disparity of symptoms associated with these anomalies, as well as differences in the way of asking about symptoms and the measurement of their severity. There seems to be no clear definition of the problem, which makes it difficult to provide precise data on the association between visual symptoms and the duration of digital device use, as well as to identify potential factors that may influence the appearance of these symptoms, such as visual dysfunctions. In this sense, the scientific literature15 has also shown the disparity of symptoms which experts consider that may be related with any type of visual anomalies. For that reason, it has been developed a questionnaire to evaluate symptoms related to any type of visual anomalies. This is the tool named Symptom Questionnaire Visual Dysfunctions (SQVD)16,17 which has been shown to be an accurate, valid and reliable questionnaire to detect visual symptoms related to any type of refractive, accommodative and binocular dysfunctions.
Several studies have analysed the association between visual symptoms and hours of use of digital devices,3,5-7,18 although there is little agreement between the symptoms that appear after hours of use. Several authors have shown for young people, that one hour of tablet or smartphone use increases eye strain and blur.2,19 Other studies have shown that adolescents have increased ocular discomfort and visual symptoms when using smartphones for more than two hours per day.20 And other studies5,7,18,21-23 consider the use of 6 h per day is related to these symptoms.
In any case, none of these studies analysed whether a particular visual dysfunction could contribute to these symptoms. Thus, it cannot be definitively concluded that the symptoms are solely caused by the specific use of these devices, as is commonly assumed. In fact, according to the concept of computer vision syndrome, patients are considered to have this syndrome regardless of whether they have a refractive, accommodative, or binocular anomaly that could be the underlying cause of several symptoms.24-28
Therefore, the aim of this study is to examine the association between visual symptoms reported by patients of a clinical sample and the hours of daily duration of digital device use, when considering the presence of any type of visual anomaly, including refractive, accommodative or binocular one.
MethodsIn order to achieve the aim of the study, a prospective study of a clinical sample of subjects from an optometric clinic (primary care clinic) was performed. Regarding the inclusion criteria, subjects with any type of ocular pathology, refractive surgery, dry eye or who were taking medication that could alter visual function, were excluded from the study. The clinical sample included 346 patients between 13 and 65 years old with a mean value of 32.95 ± 14.56 years. Of the 346 patients, 121 were men (35%) and 225 women (65%).
Informed consent was obtained from all subjects after giving them an explanation of the nature of the study. For underaged participants (those under 18 years of age), were their parents or legal guardians who accepted the study's participation principles and signed the informed consent, and the participants also gave their consent to participate. This research followed the tenets of the Declaration of Helsinki and was approved by the University of Alicante's Ethics Committee.
All patients included underwent a complete visual examination to determine the existence of any visual anomaly Thus, refractive examination was developed for all of them. Accommodative tests were only done for those subjects until 35 years old to avoid possible effects of pre-presbyopia.7,8,29 Binocular vision tests were done for all subjects independently of their age, so that in the case of the presbyopic subjects, the binocular test needed to be done at near distance were performed with their appropriate addition in place.
The examination included the following:
- •
Symptomatology. The SQVD16,17 was completed by all patients of the sample. The questionnaire has 14 items and each item has a Likert scale with three response options to indicate the frequency of the symptom: No, Occasionally or often and Almost always. The answer for each item is assigned a score between 0 and 2 points, and the total SQVD score is then obtained by adding the 14 individual item scores. The scores can then range from 0 to 28. Patient scores ≥ 6 indicate the presence of visual symptoms related to some type of visual dysfunction, be it refractive, accommodative or binocular. Results of this questionnaire were not taken into account to diagnose any visual condition (refractive, accommodative or binocular one).
- •
Refractive examination. It was achieved by means of retinoscopy and subjective examination. The subjective examination was performed by means of monocular fogging method with cross-cylinder followed by binocular balancing to a standard endpoint of maximum plus for best visual acuity. Once obtained the maximum plus value for best visual acuity, this result of the subjective examination was then used as the baseline for all accommodative and binocular vision tests.
- •
Accommodative tests.30 Monocular accommodative amplitude (push-up method31), monocular and binocular accommodative facility using ± 2.00 D flipper lenses at 40 cm, monocular estimate method (MEM) dynamic retinoscopy, and positive and negative relative accommodations at 40 cm were done.
- •
Binocular vision tests.30 The following test were performed. Unilateral and alternate cover test measurements for distant and near vision (using a prism bar, the deviation value was midway between the low and high neutral findings using an alternate cover test). Measurement of gradient and calculated AC/A ratio. Near point of convergence using an accommodative target of 20/30 visual acuity moving the target away from the subject at a speed of approximately 1 to 2 cm per second32 until the break and recovery findings were recorded. Positive and negative fusional vergences determined at far and near vision with Risley prism (with a smooth gradual increase in prism power). Both fusional vergences were measured, although their order was performed according to the subject's type of heterophoria (for exophoria the positive fusional vergence was measured first and the negative fusional vergence was performed first for esophoria). Vergence facility using 3∆ base in/ 12Δ base out prism combination at 40 cm. Worth test and stereopsis measurement using graded circles of Randot SO-002 test.
After conduction all these tests, results were analysed to determine the presence of refractive, accommodative and/or binocular anomalies within each age group. To avoid bias in diagnosing dysfunctions, this process was performed by two authors who were different from the individual who conducted the visual examination. Furthermore, the authors who carried the analysis were masked to the SQVD scores, ensuring a masked approach.
To diagnose refractive dysfunctions,30 each patient was checked for any change in their habitual refraction with respect to the subjective examination obtained in this study. The clinical criteria applied to establish this difference were having at least one of the following conditions:
1. A less negative subjective examination result than the habitual refraction; in other words, that the patient was overcorrected for myopia (equal to or greater than 0.50 D).
2. Changes in the sphere or cylinder equal to or greater than 0.50 D, with which visual acuity was increased by at least one line with the new refraction.
Accordingly, patients were diagnosed with refractive dysfunction (RD) when the subject used a different habitual refraction to that indicated by the subjective examination (as explained above) or when the subject did not use a prescription but needed it. Thus, those patients whose subject's habitual refraction was satisfactory were considered without refractive dysfunction.
Accommodative dysfunctions (AD) and nonstrabismic binocular dysfunctions (BD) were diagnosed according to the criteria described in the scientific literature.10,12,13,30 As the scientific literature has only shown the diagnostic validity for several anomalies12,13 it was decided to make a diagnosis based on the number of clinical signs associated with each dysfunction, classifying the signs that could be associated with each dysfunction as fundamental and complementary. For this purpose, we used the clinical signs as fundamental and complementary signs according to the scientific literature,10,12,13 following the criteria of García-Muñoz et al.30 Thus, for the diagnosis of an accommodative or binocular dysfunction, in addition to the fundamental clinical sign associated with each dysfunction, subjects needed to show two or more complementary signs. Accommodative dysfunctions were only diagnosed for subjects until 35 years old, as the accommodative tests in higher ages may be influenced by the proximity of presbyopia.29 However, binocular anomalies did were tested in the group of patients over 35 years old.
Subjects who presented both an accommodative and a binocular dysfunction (AD + BD) were included in this group if they presented the fundamental clinical sign of each dysfunction as well as at least one complementary sign for each of them.
Furthermore, when the same subject presented a refractive dysfunction and an accommodative and/or binocular dysfunctions, these subjects were included within the group corresponding to their accommodative and/or binocular dysfunction, even though they also presented with a refractive dysfunction.
Strabismus and amblyopia were diagnosed following the Multi-ethnic Pediatric Eye Disease Study Group (MEPEDS study) criteria.33-35 Strabismus was considered when a heterotropia at distance and/or near fixation was present, with or without spectacle correction and was classified as esotropia, exotropia or hypertropia. Unilateral amblyopia was defined as a ≥ 2-line interocular difference in best corrected visual acuity (BCVA) with ≤20/32 in the worse eye and presence of a unilateral amblyopia risk factor. Bilateral amblyopia was defined as bilaterally deficient BCVA (<20/50 in 30–47 months or <20/40 in ≥48 months) in the presence of bilateral isoametropia or with evidence of visual axis obstruction of both eyes.
Those subjects who did not have any visual dysfunction were classified as a group without dysfunction. Therefore, in this group were both patients who did not have any refractive dysfunction and those who did not have any type of accommodative/binocular anomaly.
Data analysisPatients were asked to report the number of daily hours using all digital devices (including the time spent using the computer, tablet, smartphone and all other digital devices) so that number of hours was referred to the total use of devices. The time of use of these devices was categorized according to the number of hours used. According to the scientific literature a threshold of 6 h per day was used to quantify the effects of using digital devices.5,7,18,21-23,28,36,37 Thus, dichotomous variables were created dividing the sample between those patients with equal or less than 6 h of using and those with more than 6 h.
In addition to that, the sample was divided into two groups of patients according to the age, patients under and over 35 years old.
The association between the number of hours of digital device use and the presence or absence of visual symptoms according to the SQVD was analysed using a multivariate logistic regression. In this analysis, the presence of any visual dysfunction (RD, AD, BD, AD + BD, strabismus, and amblyopia) was considered a confounding variable for the association between symptoms and the number of hours using these devices. Therefore, the likelihood of having visual symptoms according to the hours of digital device use was analysed after eliminating the possible effect that these visual dysfunctions could have on this association. This assessment was evaluated by means of a multivariate logistic regression, showing the crude odds ratio (OR) and the adjusted OR for each variable analysed.
The statistical analysis was performed using the SPSS 26.0 statistical tool for Windows.
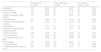
ResultsOf the 346 subjects examined, 198 patients (57.2 % of the total) had symptoms according to the SQVD. There was no association between having symptoms and sex (p = 0.205 for patients under 35 years, p = 0.444 for patients over 35 years). Table 1 shows the symptoms encountered in the sample, according to the 14 items showed in the SQVD.
Symptoms according to the 14 SQVD items, encountered in the patients of the sample.
According to the visual anomalies encountered, 226 subjects (65.32% of the total) had any type of visual anomaly. Table 2 shows the distribution of patients for each group of dysfunctions, for the overall sample and the two subgroups made in the sample, subjects between 13 and 35 years old and the group of patients between 36 and 65 years old.
Number of patients within each dysfunction category, for the overall sample and the two subject subgroups, aged 13 to 35 years, and 36 to 65 years old. (AI: accommodative insufficiency, AE: accommodative excess, CI: convergence insufficiency, CE: convergence excess, DI: divergence insufficiency, BE: basic esophoria; BX: basic exophoria; CI95%: confidence interval at 95%).
Results of the crude OR to assess the association between having symptoms and the different variables analysed (that is, the hours of digital device use and the different groups of visual dysfunctions) are shown in Table 3. Table 4 shows the results of the multivariate logistic regression, showing the adjusted OR for all variables analysed: the hours of using digital devices and the presence of each group of dysfunctions.
Crude odds ratio (OR) of the association between visual symptoms and the variables of using digital devices and having visual dysfunctions, for the group under 35 years old and the group over 35 years old. (*: indicates statistically significative; AD: accommodative dysfunction; BD: binocular dysfunction).
Multivariate logistic regression with the adjusted odds ratio (OR) of the association between visual symptoms and visual dysfunctions, for the group under 35 years old. (*: indicates statistically significative).
Results for patients under 35 years (Table 3) revealed a statistically significant association (OR 2.10, p = 0.01) between having visual symptoms and the use of digital devices for more than 6 h. And the same was happen for all visual dysfunctions, for which there was an association between having visual symptoms and the presence of any type of visual dysfunction, except for the group of strabismus and amblyopia. However, when adjusting by the confounding variables (Table 4), the multivariate logistic regression showed that the variable of the hours of using digital devices was no longer associated with symptoms whilst all items related to each type of visual dysfunctions obtained statistically significant OR, showing association.
For the group of patients over 35 years (Table 3), the crude OR showed that there was not a statistical association between symptoms and the use of digital devices (OR 1.27, p = 0.49), so that the multivariate logistic regression did not have to be done. The crude OR was not obtained for accommodative dysfunctions (as there was no anomaly) nor for binocular dysfunctions (as there were only 2 patients).
DiscussionThe results of this research in a clinical population show that the likelihood of presenting visual symptoms does not depend on the hours of digital device use but rather on the presence of any type of visual dysfunctions, including refractive, accommodative and/or binocular one.
It was found that 57.2 % of the analysed sample in this study reported some type of visual symptoms according to the SQVD. These results are lower than other studies, but their differences may be attributed to variations in the patient populations examined. For instance, Altalhi et al.,36 who analysed university students, reported that the 97.3% of participants had symptoms related to digital devices. Porcar et al.,7 focusing on adult workers who used video display units (VDU) for their occupation, reported a frequency of 72% of patients with symptoms. Other example of higher values of symptoms is seen in the study by Kharel et al.38 in which the authors found a prevalence of symptoms of 71.6% in a sample of university students. Although our results are not exactly equal, they are closer to those found in a randomised sample,10 where 44.6% of subjects had symptoms and in which the information was collected in a clinical sample as we did. The fact of having a randomised sample may be the reason for these differences, as when patients are collected in a randomised way, there is less likelihood to have a particular event, in this case, symptoms.
Considering visual dysfunctions, 65.02% of the subjects in this sample presented visual anomalies, a value which agrees with the score of 58.3% reported in other studies that used the same diagnostic criteria.30 These values are higher than others found in the scientific literature,11 which is logical since our sample was a clinical population where individuals with visual dysfunctions are more likely to be present. In any case, specifying by dysfunctions, the prevalence results for accommodative and binocular anomalies agree with those found by other studies, as those values found in the study by Garcia- Muñoz et al.,30 conducted on a random sample of university students, as well as those observed in the study by Porcar et al.,8 which evaluated subjects who were digital devices users. This suggests that our sample, despite not being random, is indeed representative in terms of visual dysfunctions compared to what is reported in the scientific literature.
Regarding the relationship of the symptomatology to the hours of use of digital devices, our results show that in crude analysis, there was no association between the use of digital devices and symptoms for patients over 35 years old. This result agrees with that of Sánchez-Brau et al.39 in which the authors found no association between symptoms and the use of more than 6 h with digital devices in workers over 45 years old. However, we did find an association between symptoms and the presence of refractive dysfunction, highlighting the importance of wearing the appropriate refractive correction for these individuals.
For patients under 35 years old, there were an association between the number of hours of using these devices and the presence of symptoms, but this association disappeared when considering the confounding factor of having a visual dysfunction. And this piece of evidence means that the hours of digital device use are not the causal factor for these symptoms, but rather these symptoms appear because the patients have visual dysfunctions. This is the most significant and important finding of our study, challenging the common assumption that the use of smartphones, tables or computers directly causes visual symptoms. And that is not the case. Our results show a novel perspective that has not been previously explored.
In this sense, in the scientific literature, several studies3,5-8,18,21-28,36-38,40 have analysed the association between symptoms and the use of these digital devices. Some of them3,5,7,8,18,21-27,38,40 have found an association between visual symptoms and their use, particularly they have observed that symptoms improve when using these devices since 2 h,8,38,40 4 h,26 5 h3,24,25,27 and 6 h.5,7,18,21-23 And there are other authors who have not observed this association,6,28,36,37 for which, once again, a threshold of greater than 6 h per day of device usage was the most commonly employed duration for this analysis.28,36,37
According to the studies which have shown this association between symptoms and the number of hours of using these devices,3,5,7,8,18,21-27,38,40 two of them,23,25 did not consider the presence of any visual anomalies, nor did they perform a visual examination or asking for the habitual prescription, thus failing to account this aspect when analysing their results. The other studies3,5,7,8,18,21,22,24,26,27,38,40 did consider the refractive status of patients, with only four of them performing a visual examination7,8,38,40 while the others only asked about the use of an optical correction when using these devices.3,5,18,21,22,24,26,27 However, none of these studies considered the possibility that a visual anomaly could be a confounding factor that could be related to visual symptomatology. As a result, they cannot assure that symptoms were due to the use of these devices. For that reason, all of these studies are not comparable to our results. In contrast, by conducting a complete visual examination, we have been able to diagnose any type of visual anomaly, clearly showing how the confounding factor of having any type of visual dysfunctions can influence the results.
Furthermore, among those studies that found an association between having symptoms and the number of hours of using these devices,3,5,7,8,18,21-27,38,40 only three studies21,26,40 performed an association analysis using logistic regression to assess the association between the number of hours of device use and the presence of symptoms. However, none of them considered the adjusted odds ratio (OR) for the presence of visual dysfunction to examine whether these anomalies (refractive, accommodative or binocular) could be a confounding factor between the number of hours of using the devices and the visual symptoms.
According to the studies which have not shown this association between symptoms and the use of these devices,6,28,36,37 three of them6,36,37 did not perform any refractive examen and did not take into account the refractive status of the patients. Only one study28 considered the refractive error of patients (but not other accommodative and binocular anomalies) but they did not take into account this variable as a confounding factor in a multivariate logistic regression, which could bias their results. In any case, since none of these studies6,23,28,36 performed an association analysis adjusting for the presence of a visual anomaly, their results were biased in this sense.
As mentioned above, our study has not encountered an association between symptoms and the use of these devices, but with different visual dysfunctions: refractive, accommodative, binocular and accommodative plus binocular ones. Results show that a person with these visual anomalies is more likely to have visual symptoms compared to a person who does not have them. These findings are in agreement with those obtained by other authors10 who obtained that subjects with some kind of visual dysfunction are more likely to experience symptoms than those without any visual anomaly.
In any case, our results are not comparable with those studies in which the authors found an association between symptoms and the number of hours of using these digital devices,3,5,7,8,18,21-27,38,40 and the explanation is due to the different samples analysed. Our sample is a clinical one and the other studies usually examine samples with particular characteristics, as office workers,3,5,8,18,23,24 computer users6,7,23,40 or students.8,22,23,25-27,36,38 And certainly, both approaches may be complimentary to obtain a picture of the situation. Office workers may be appropriate samples to reflect the situation in offices, but clinical samples are essential for considering the situation in the clinical practice, as they are representative of patients who suffer symptoms and attend an optometric clinic where these visual conditions are commonly seen. In fact, it must be taken into account that workers or computer users who experience symptoms, are likely to visit an optometric clinic to solve their visual problems. Therefore, this approach must be analysed to know what happens to patients who visit an optometric clinic with these problems.
In this sense, considering the findings of this study that have shown an association with the presence of any type of visual dysfunction, this factor must be contemplated as a confounding factor. So, in future studies focused on particular samples, such as workers who use computers, or studies on computer visual syndrome (CVS), it should be taken into account the fact that the presence of a visual dysfunctions (refractive, accommodative and/or binocular one) may be a confounding factor. It must be considered that those questionnaires which are used to determine the presence of CVS have many items which are the same questions about visual symptoms related to these visual anomalies. It is highly likely that many patients diagnosed with CVS, actually have undiagnosed and untreated visual dysfunctions. This argument agrees with the results of the systematic review of Jaiswal et al.1 in which the authors state that when using these digital devices, accommodation and vergence systems are altered so that the impact on patients with accommodative and binocular vision anomalies needs to be determined in these studies.
In conclusion, based on the clinical sample analysed in this study, the likelihood of presenting visual symptoms does not depend on the hours of digital devices use but rather on the presence of a refractive, accommodative and/or a binocular anomaly. Patients with visual dysfunctions are more prone to present visual symptoms when using digital devices compared to those without such visual anomalies. This implies that when clinicians examine those patients who use these various digital devices, they should consider that visual symptoms are not due to the use of tablets, smartphones or computers, but rather to the presence of a refractive, accommodative or a binocular anomaly which may be diagnosed and treated by clinicians.
FundingThis research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Date of submission of reviewed manuscript10, November 2023.
Conflicts of interestThe authors report no conflict of interests and have no proprietary interest in any of the materials mentioned in this article.