Interpupillary distance (IPD) is important in developmental anatomy, genetics, design of optical instrumentation, ocular diagnostics, and optical prescribing. IPD frequently is measured on different days, and by either automatic pupillometers (physiological measurement) or manual ruler (anatomical measurement). Therefore, there is importance in the agreement and inter-session repeatability of manual and automatic IPD measurements.
MethodsMonocular distance from the bridge of the nose and binocular distance and near binocular IPD were randomly measured, using a millimeter ruler and the Essilor Pupillon pupillometer. Gender effects were assessed using Wilcoxon and Mann-Whitney tests, respectively. Agreement was assessed using Spearman correlation and Bland-Altman (B&A) plots. Thirty additional participants were tested within 1–2 weeks to determine the inter-session repeatability.
ResultsThe agreement study included 199 participants (mean age: 24.1 ± 5.0 range: 19−53, 58 male, 141 female) and the repeatability sub- study included 30 (mean age: 27.9 ± 4.5, range: 23–39, 6 male, 24 female). Males and females significantly differed in age (<2 year mean difference (md)) and IPD (monocular md: < 1 mm, binocular md: < 2 mm). Manual vs. automatic measurements were significantly different for all conditions (md: <1 mm for all) except for distance left eye male PD. There was no significant difference between the session for both methods.
ConclusionsBinocular and monocular manual and automatic measurements were significantly different statistically, but not clinically. Distance binocular IPD was approximately 3 mm wider than near IPD. Male binocular IPD was approximately 2 mm wider than the female IPD. Both methods had good inter-session repeatability.
Interpupillary distance (IPD) is the distance between the centers of the pupils.1,2
The IPD is relevant for developmental anatomists and geneticists,3 and has significance in many aspects of visual function. IPD is a clinical measure in surgery after facial trauma.4 Normative values of IPD are useful in the diagnosis of certain syndromes. For example, ocular hypotelorism in which the IPD is small, is associated with mongolism4 and hypertelorism, in which the IPD is large,5 is associated with acrocephalosyndactly (Apert’s syndrome),6,7 craniofacial dystosis (Crouzon’s disease),8 median cleft face syndrome (frontonasal dysplasia),7 Klinefelter Syndrome,9 as well as fetal hydantoin syndrome.10 Hypertelorism can have a secondary effect of exotropia, as well.11
In stereoscopic visual perception, the IPD determines the magnitude of the horizontal separation between the images seen by each eye, which are later combined by the brain into a stereoscopic three dimensional percept.2
In the technological world, the mean IPD is critical in the design of night viewing goggles,12 stereoscopic display devices and the production of stereoscopic content.2,4 Mismatches between the oculars of viewing devices and the viewer’s IPD result in loss of stereoscopic visual information13 and visual fatigue.14 Surgical stereoscopic imaging devices that are designed with a fixed IPD of 65 mm, for example, may not match all surgeons, and may pose risks when visual information is lost.15
IPD also affects the perceived visual angle of objects in virtual reality. Subjects with smaller IPDs perceive a larger visual angle of objects in virtual reality than those with larger IPDs.16 In stereoscopic viewing systems, viewers with larger IPDs prefer uncrossed disparities which can affect their visual comfort.17
In ocular examination, the accuracy of the IPD measurement can affect results of clinical tests.18 Clinicians adjust the phoropter or trial frame according to the patient’s IPD and the required working distance.19 Deviations between the oculars and the patient’s IPD can therefore result in prismatic effects, aberrations, and incorrect clinical measurements.18
IPD is also related to the accommodative vergence to accommodation (AC/A) ratio and is used to determine the ratio in the calculated AC/A method of clinical testing.20 The AC/A ratio has been shown to be reduced when the IPD is reduced.21 In addition, IPD provides information to the clinician regarding the patient’s vergence demand. Individuals with larger IPD have a greater convergence demand for near viewing, requiring larger fusional reserves.22
In optical dispensing, the correct IPD minimizes prismatic effects which could result from an incorrect placement of the optical centers of the lenses within the spectacles, and can cause non-tolerance.23–25 Applying the incorrect IPD has implication for the use of ready-made, over the counter readers by patients with IPDs that deviate from population norms. Approximately 62% of 1080 patients reported asthenopia while wearing over the counter readers that were mismatched to their IPD.26 Furthermore, prismatic effects caused by misalignment between the optical centers of spectacles and the pupils were found to induce a mean change of 1Δ of heterophoria.27 This change can be sufficient to cause asthenopia in patients with preexisting large heterophorias.28 Prismatic effects have also been shown to reduce stereoscopic depth perception.29
Accurate IPD measurements are especially critical in the proper fitting of progressive addition lenses (PALs). In bifocals prescribed to adults, for example, the inset should be larger for larger IPDs.30 In bifocals prescribed to pediatric patients, misalignment between the optical centers of the spectacle lenses and the IPD can impair several visual functions.31 Visual acuity can be reduced, especially in high prescriptions. In addition, vertical and horizontal heterophorias can be induced, which may cause symptoms. Finally, in extreme cases, decentration of the lens and pupil centers can cause diplopia.31
Incorrect placement of the optical centers of PALs with respect to the IPD results in poor alignment of the vertical corridors of vision for intermediate and near use, resulting in a limited field of view for the patient.32 Incorrect specification of the IPD was reported to be a major causative factor in 25% of 32 adults who did not tolerate their PALs.33
In the clinical setting, IPD can be measured either manually or automatically (digitally). Manual measurements use a millimeter (mm) ruler to note the distance between common points in the two eyes.34 This measurement is often referred to as the anatomical IPD.1,23 Automatic measurements calculate the distance between the two principal corneal reflexes and are often referred to as the physiological IPD.1,23
Textbooks recommend automatic measurements for larger refractive errors in order to minimize prismatic effects.18
In busy practices, IPD may be measured by on different occasions by different personnel, some more experienced than others.23 IPD measurements of inexperienced personnel were shown to be inaccurate and with poor repeatability.35 Manual measurements of the IPD are affected by parallax, differences between the observer’s and patient’s IPD,36 incorrect ruler positioning,37 and indistinct limbal margins due to patient characteristics (arcus senilis or pterygium, for example).1,23 In this sense, automatic pupillometers are expected to provide better repeatability, as the result is much less dependent on the examiner. Three prior studies reported clinically insignificant differences between the results of two IPD-measurement methods.1,23,38 However, in two studies1,23 the order of testing was not randomized, and the same unmasked examiner performed both methods of IPD measurement. One study23 did not use a mm ruler to measure the anatomical IPD, as is typically done in clinical practice.18 Herein, we examined the agreement of manual mm ruler measurements and automatic pupillometer measurements of IPD, each performed by a different examiner, who was masked to the results obtained by the other. Even when measured by the same experienced examiner, IPD is often measured on different days. Previous studies did not examine inter-session repeatability (i.e., IPD measurements performed on different days). In the present study, we examined the inter-session repeatability of manual and automatic IPD measurements.
IPD may be measured binocularly and monocularly. Monocular PD measurements are recommended in cases of progressive lenses,18,39 prescribing prisms,40 pediatric examinations,41 facial asymmetry,42 craniofacial surgery,43 and higher index ophthalmic lenses.42 Previous studies only compared binocular IPD measurements. Therefore, in the present study, we also included monocular PD measurements.
Because IPD varies with age, ethnicity and gender 2,24,34 the present study included a cohort of participants from Israel not previously reported and compared the differences between the genders in this cohort. To the best of our knowledge, this is also the first study to specifically validate the Essilor Pupillon pupillometer.
MethodsAgreement studySubjectsHealthy students and staff were recruited by email for vision screening at the Optometry Department at Hadassah Academic College, Jerusalem, Israel (HAC). Participants filled out a general and family history questionnaire. All participants underwent tests of binocular distance and near Snellen visual acuity. However, there was no visual acuity criterion for participation. All subjects had normal eye movements as assessed by an extraocular motility test, at least 70″ stereopsis (Paul Harris Randot stereotest, Bernell, USA), and did not have strabismus as verified with a distance and near cover test.
The study was approved by the HAC ethics committee and a statement of informed consent was obtained prior to participation.
ProceduresThe IPD measurements of all subjects, for all conditions were performed without spectacle correction, similarly to the clinical setting.
Manual measurementsFour types of manual IPD measurements were performed: binocular near, binocular distance, and monocular right eye and monocular left eye distance (from the bridge of the nose) using the Viktorin method as described by others 5,24,44
Each measurement was performed two consecutive times and averaged.5,24,34
The manual PD for near and distance was determined using a two-step procedure. The first step measured the binocular near IPD. The subject was asked to fixate on the examiner’s left eye. During fixation, the examiner determined the distance between the temporal limbus of the subject's left eye (Ltemporal) and the nasal limbus of the subject's right eye (Rnasal), using a millimeter ruler. The near IPD was then calculated as:
Near IPD = Subject fixating on examiner's left eye : Ltemporal → Subject fixating on examiner's left eye :Rnasal
In the second step, the binocular distance IPD was determined. Unlike the first step, the subject was asked to change fixation from the examiner's left eye, to the examiner’s right eye. Then, similarly to the near IPD measurement, the examiner determined the location of the subject's right nasal limbus and calculated:
Distance IPD = Subject fixating on examiner's left eye : Ltemporal → Subject fixating on examiner's right eye :Rnasal
Manual monocular measurements were performed with the examiner level with the subject and facing the subject. A specially marked PD ruler (Appendix 1) was placed on the bridge of the nose in the center of the subject's face, approximately in the back vertex plane of the spectacle lens. In order to measure the monocular right eye pupillary distance, the examiner closed his left eye and asked the subject to fixate on his open right eye. The examiner then noted the location of the center of the subject's right eye pupil from the corresponding mark on the PD ruler scale that was located directly below the subject's right eye. In order to measure the monocular left eye pupillary distance, the examiner opened his left eye and closed his right eye. He then asked the subject to fixate on his left eye while reading the location of the center of the subject's left eye pupil from the corresponding mark on the PD ruler scale.
Automatic IPD measurementsFour types of automatic PD measurements were performed: binocular near, binocular distance, monocular right eye distance, and monocular left eye distance. The automatic PD measurements were performed using the Essilor pupillometer (Pupillon, Essilor, France). The Pupillon displays a reading that is the mean of four measurements. As such, only one recording with the Pupillon was measured for each condition.
The manual and automatic measurements were conducted and recorded in alternating order. For example, if a subject was first measured using the manual method, they were subsequently measured using the automatic method. The next subject was then first measured using the automatic method, and subsequently measured using the manual method, etc.
The manual method was performed by one examiner and the automatic method was performed by another examiner, both experienced optometrists, each of whom were each masked to each other’s result.
Inter session repeatabilityThirty additional participants were recruited via emails to participate in a separate experiment examining the inter-session repeatability. Similarly to the vision screening participants, these participants filled out a general and family history questionnaire. Inclusion and exclusion criteria for these subjects was the same as described above.
These subjects participated in two study visits, 1–2 weeks apart. In both study visits, their manual and automatic PD measurements were recorded as detailed above.
In this sub-study, all PD measurements were performed three times. The order of the measurement methods was alternated as described previously. The manual and automatic measurements were performed by two different experienced optometrists, each masked to the results obtained by the other. The same optometrists performed the same measurement method on both study visits.
Data analysisOutcome parameters were tested for normality using the Shapiro-Wilk test, which indicated that most measures were normally distributed. Therefore, nonparametric statistics were applied for subsequent analyses. The paired-samples Wilcoxon test was applied to compare between the results of the two IPD measurement methods and an Independent Mann Whitney test was applied to compare between the gender groups.
The interchangeability of the manual and automatic measurements of data obtained in the vision-screening assessment was evaluated using Spearman's rank correlation and Bland and Altman plots.45 Bland-Altman plots indicate the mean difference (Md) and 95% confidence intervals (CI) calculated as Md ± 1.96* standard deviation (SD), which specify the interval within which 95% of the differences between the measurement of the two sessions was expected to fall.45 These are known as the 95% limits of agreement.
Non-normally distributed data were analyzed using the Bland & Altman non-parametric approach.46 According to this approach, measurements are compared using a clinically acceptable interval range. Therefore, based on previous results,44 an interval range of ±1 mm for monocular measurements and ±2 mm for binocular measurements was considered the clinical range of resolution.
The inter-test repeatability for each method was assessed using the mean values of the three measurements of each session. A paired-samples Wilcoxon test was applied to compare the first session's measurements to the second session's measurements, separately for each type of measurement.
As stated above, the manual IPD was measured two consecutive times, and the mean measurement was calculated. The automatic pupillometer displays the results of four consecutive measurements, without providing the values for each individual measurement. As such, it was not possible to compare the intra-test repeatability or intra-class correlation coefficient of the two techniques.
For all statistical tests, P values lower than 0.05 were considered statistically significant.
ResultsA total of 199 subjects (mean age: 24.1 ± 5.0 range: 19−53, 58 male, 141 female) participated in the agreement study (manual millimeter ruler and an automated Essilor pupillometer). The mean age, distance monocular and binocular visual acuity, stereoacuity, and measured IPD values using the manual and automated methods for all the subjects and for males and females separately, are tabulated in Table 1. There was a statistically significant difference between the ages and the IPD of the male and female participants. `
Mean and standard deviations of outcome measures of study participants.
| Mean ± SD (N) | Mean ± SD (N) | Mean ± SD (N) | Mann-Whitney test | ||
|---|---|---|---|---|---|
| All subjects | Male (M) | Female (F) | U value | P value (M vs F) | |
| Age (year) | 24.12 ± 5.04 (199) | 25.05 ± 5.95 (58) | 23.74 ± 4.58 (141) | 2575.5 | < 0.001 |
| RE Distance VA (decimal) | 0.87 ± 0.28 (199) | 0.89 ± 0.28 (58) | 0.86 ± 0.28 (141) | 3796.5 | 0.40 |
| LE Distance VA (decimal) | 0.87 ± 0.28 (199) | 0.86 ± 0.28 (58) | 0.87 ± 0.28 (141) | 3983 | 0.76 |
| Binocular Distance VA (decimal) | 1.05 ± 0.26 (199) | 1.03 ± 0.28 (58) | 1.06 ± 0.25 (141) | 3989 | 0.77 |
| Binocular Near VA (decimal) | 1.37 ± 0.32 (173) | 1.35 ± 0.34 (54) | 1.38 ± 0.31 (119) | 3102.5 | 0.57 |
| Stereoacuity (arc of sec) | 42.09 ± 18.71 (196) | 41.21 ± 18.62 (58) | 42.46 ± 18.80 (138) | 3830.5 | 0.63 |
| RE Distance manual PD (mm) | 30.37 ± 1.74 (199) | 31.04 ± 1.97 (58) | 30.10 ± 1.57 (141) | 2890.5 | < 0.001 |
| LE Distance manual PD (mm) | 29.88 ± 1.53 (199) | 30.41 ± 1.56 (58) | 29.66 ± 1.46 (141) | 3037 | < 0.001 |
| Binocular Distance manual PD (mm) | 60.57 ± 3.21 (199) | 61.90 ± 3.35 (58) | 60.03 ± 3.00 (141) | 2765.5 | < 0.001 |
| Binocular Near manual PD (mm) | 57.12 ± 3.09 (199) | 58.61 ± 3.26 (58) | 56.50 ± 2.81 (141) | 2560.5 | < 0.001 |
| RE Distance Pupillometer (mm) | 29.65 ± 1.89 (199) | 30.34 ± 2.08 (58) | 29.37 ± 1.73 (141) | 2988.5 | < 0.001 |
| LE Distance Pupillometer (mm) | 29.66 ± 1.99 (199) | 30.70 ± 1.97 (58) | 29.24 ± 1.84 (141) | 2381 | < 0.001 |
| Binocular Distance Pupillometer (mm) | 59.32 ± 3.44 (199) | 61.04 ± 3.71 (58) | 58.61 ± 3.06 (141) | 2482 | < 0.001 |
| Binocular Near Pupillometer (mm) | 56.31 ± 3.32 (199) | 57.96 ± 3.61 (58) | 55.63 ± 2.94 (141) | 2481 | < 0.001 |
The IPD was measured as part of an overall vision screening. Some subjects did not participate in all stations. Therefore, the number of participants for each outcome measure appears in parenthesis.
Table 2 describes the statistical comparisons of the differences between the two methods of IPD measurements for all participants, as well as separately for males vs. females. The manual measurements were significantly different from the automated Essilor Pupillon pupillometer for all conditions except for the distance left eye measurements in the male sub-cohort.
Wilcoxon test of comparisons between manual millimeter ruler vs. automated Essilor Pupillon pupillometer measurements.
| Subjects | Wilcoxon test | ||
|---|---|---|---|
| Z value | P value | ||
| RE Distance | All subjects | −7.52 | < 0.001 |
| Male | −4.15 | < 0.001 | |
| Female | −6.27 | < 0.001 | |
| LE Distance | All subjects | −2.44 | < 0.02 |
| Male | 1.75 | 0.08 | |
| Female | −3.81 | < 0.001 | |
| Binocular Distance | All subjects | −10.02 | < 0.001 |
| Male | −3.99 | < 0.001 | |
| Female | −9.16 | < 0.001 | |
| Binocular Near | All subjects | −9.09 | < 0.001 |
| Male | −4.35 | < 0.001 | |
| Female | −8.01 | < 0.001 | |
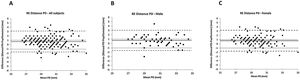
The rank correlation coefficient, mean difference (value ± SD), the 95% CI, and the clinical range of resolution between the manual millimeter ruler and the automated pupillometer distance monocular right eye measurements are shown in Table 3andFig. 1.
Correlation, agreement, and mean difference between manual and automatic measurements of monocular right eye PD.
| RE Distance | Correlation | Bland and Altman Agreement | |||
|---|---|---|---|---|---|
| rs | p | Mean difference (mean ± SD) | Mean difference + 1.96 SD | Mean difference - 1.96 SD | |
| All subjects | 0.77 | < 0.001 | 0.72 ± 1.22 | 3.12 | −1.68 |
| Male | 0.84 | < 0.001 | 0.69 ± 1.18 | 3.01 | −1.61 |
| Female | 0.73 | < 0.001 | 0.73 ± 1.24 | 3.18 | −1.71 |
Comparison of manual and automatic monocular right eye PD measurements. Bland and Altman plots representing the difference between manual and automatic monocular right eye pupillary distance measurements for all subjects (a) males (b) and females (c). The black line represents the mean difference, whereas the dashed lines show the 95% limits of agreement, and dotted lines show ±1 mm which are the upper and lower clinical range of resolution. Each data point represents one participant. All values presented are in millimeters.
For the monocular manual and automatic right eye PD measures, the mean differences of 63%, 62%, and 63% of all participants, male participants, and female participants were within clinical range of resolution (±1 mm), respectively.
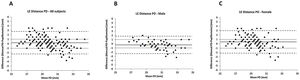
The correlation coefficient, mean difference (value ± SD), the 95% CI, and the clinical range of resolution between the manual millimeter ruler and the automated pupillometer distance monocular left eye measurements are shown in Table 4andFig. 2.
Correlation, agreement, and mean difference between manual and automatic measurements of monocular left eye PD.
| LE Distance | Correlation | Bland and Altman Agreement | |||
|---|---|---|---|---|---|
| rs | p | Mean difference (mean ± SD) | Mean difference + 1.96 SD | Mean difference - 1.96 SD | |
| All subjects | 0.78 | < 0.001 | 0.21 ± 1.28 | 2.72 | −2.29 |
| Male | 0.85 | < 0.001 | −0.28 ± 1.06 | 1.80 | −2.37 |
| Female | 0.73 | < 0.001 | 0.42 ± 1.30 | 2.98 | −2.14 |
Comparison of manual and automatic monocular left eye PD measurements. Bland and Altman plots representing the difference between manual and automatic monocular left eye pupillary distance measurements for all subjects (a) males (b) and females (c). The black line represents the mean difference, whereas the dashed lines show the 95% limits of agreement, and dotted lines show ±1 mm which are the upper and lower clinical range of resolution. Each data point represents one participant. All values presented are in millimeters.
For the monocular manual and automatic left eye PD measures, the mean differences of 74%, 76%, and 73% of all participants, male participants, and female participants were within clinical range of resolution (±1 mm), respectively.
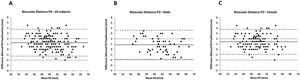
The correlation coefficient, mean difference (value ± SD), the 95% CI, and the clinical range of resolution between the manual millimeter ruler and the automated pupillometer distance binocular IPD measurements are shown in Table 5andFig. 3.
Correlation, agreement, and mean difference between manual and automatic measurements of distance binocular IPD.
| Binocular Distance | Correlation | Bland and Altman Agreement | |||
|---|---|---|---|---|---|
| rs | p | Mean difference (mean ± SD) | Mean difference + 1.96 SD | Mean difference - 1.96 SD | |
| All subjects | 0.93 | < 0.001 | 1.25 ± 1.27 | 3.76 | −1.25 |
| Male | 0.92 | < 0.001 | 0.85 ± 1.39 | 3.59 | −1.88 |
| Female | 0.93 | < 0.001 | 1.41 ± 1.19 | 3.76 | −0.98 |
Comparison of manual and automatic binocular distance IPD measurements. Bland and Altman plots representing the difference between manual and automatic distance binocular inter-pupillary distance measurements for all subjects (a) males (b) and females (c). The black line represents the mean difference, whereas the dashed lines show the 95% limits of agreement, and dotted lines show ±2 mm which are the upper and lower clinical range of resolution. Each data point represents one participant. All values presented are in millimeters.
For measures of binocular IPD, the mean differences of 77%, 81%, and 75% of all participants, male participants, and female participants were within the clinical range of resolution (±2 mm), respectively.
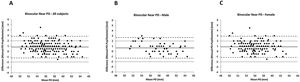
The correlation coefficient, mean difference (value ± SD), the 95% CI, and the clinical range of resolution between the manual millimeter ruler and the automated pupillometer near binocular IPD measurements are shown in Table 6andFig. 4.
Correlation, agreement, and mean difference between manual and automatic measurements of near binocular IPD.
| Binocular Near | Correlation | Bland and Altman Agreement | |||
|---|---|---|---|---|---|
| rs | p | Mean difference (mean ± SD) | Mean difference + 1.96 SD | Mean difference - 1.96 SD | |
| All subjects | 0.95 | < 0.001 | 0.80 ± 1.00 | 2.82 | −1.20 |
| Male | 0.96 | < 0.001 | 0.65 ± 0.99 | 2.63 | −1.33 |
| Female | 0.93 | < 0.001 | 0.87 ± 1.01 | 2.89 | −1.14 |
Comparison of manual and automatic binocular near IPD measurements. Bland and Altman plots representing the difference between manual and automatic near binocular inter-pupillary distance measurements for all subjects (a) males (b) and females (c). The black line represents the mean difference, whereas the dashed lines show the 95% limits of agreement, and dotted lines show ±2 mm which are the upper and lower clinical range of resolution. Each data point represents one participant. All values presented are in millimeters.
The mean differences of 92%, 91%, and 92% of all participants, male participants, and female participants were within the clinical range of resolution (±2 mm), respectively.
Inter session repeatabilityA total of 30 subjects (mean age: 27.9 ± 4.54, range: 23–39, 6 male, 24 female) participated in the inter-test repeatability sub-study. The mean age, distance monocular visual acuity, stereoacuity, and all measured IPD values using the manual and automated methods for all the subjects and, separately, for males vs. females are tabulated in Table 7. There was a statistically significant difference between male and female binocular near IPD measurements.
Mean and standard deviations of outcome measures of study participants (N = 30).
| Mean ± SD | Mean ± SD | Mean ± SD | Mann-Whitney test | ||
|---|---|---|---|---|---|
| All subjects | Male (M) | Female (F) | U value | P value (W vs M) | |
| Age (year) | 27.9 ± 4.54 | 29.83 ± 7.96 | 27.41 ± 3.32 | 69.50 | 0.89 |
| RE Distance VA (decimal) | 1.05 ± 0.08 | 1.03 ± 0.10 | 1.05 ± 0.09 | 63.00 | 0.54 |
| LE Distance VA (decimal) | 1.06 ± 0.09 | 1.03 ± 0.10 | 1.06 ± 0.09 | 60.00 | 0.43 |
| Stereoacuity (arc of sec) | 32 ± 9.96 | 26.66 ± 10.32 | 33.33 ± 9.63 | 48.00 | 0.14 |
| RE Distance manual PD (mm) | 30.16 ± 1.30 | 30.81 ± 1.89 | 30 ± 1.10 | 57.00 | 0.43 |
| LE Distance manual PD (mm) | 30.45 ± 1.62 | 31.72 ± 2.56 | 30.13 ± 1.17 | 45.00 | 0.16 |
| Binocular Distance manual PD (mm) | 60.69 ± 2.91 | 62.55 ± 4.29 | 60.15 ± 2.18 | 45.50 | 0.17 |
| Binocular Near manual PD (mm) | 57.55 ± 2.96 | 59.34 ± 5.53 | 57.10 ± 1.83 | 0.00 | 0.001< |
| RE Distance Pupillometer (mm) | 29.99 ± 1.42 | 30.90 ± 2.57 | 29.76 ± 1.00 | 58.50 | 0.48 |
| LE Distance Pupillometer (mm) | 29.90 ± 1.87 | 30.97 ± 2.93 | 29.55 ± 1.34 | 50.50 | 0.26 |
| Binocular Distance Pupillometer (mm) | 59.14 ± 3.87 | 59.36 ± 8.14 | 59.08 ± 2.11 | 70.00 | 0.91 |
| Binocular Near Pupillometer (mm) | 56.77 ± 2.94 | 58.45 ± 5.10 | 56.28 ± 2.08 | 51.00 | 0.27 |
The inter-session repeatability was assessed by calculating the mean difference between the PD values measured in the first session and the second session, as seen in Table 8. No statistically or clinically significant difference was observed between the first and the second sessions for either manual or pupillometer measurements. The mean differences were all lower than 0.6 mm. Bland and Altman analysis, summarized in Table 9 also showed no significant difference between the first and second sessions for both methods, with 70% to 100% of the observations falling within the clinical range of resolution (±1 mm).
Inter-test repeatability for manual millimeter ruler and the pupillometer.
| All subjects | Male (M) | Female (F) | ||
|---|---|---|---|---|
| RE Distance manual PD (mm) | Mean difference | −0.01 | −0.25 | 0.04 |
| SD of difference | 0.58 | 0.56 | 0.58 | |
| P value (Z Wilcoxon value) | 0.94 (-0.72) | 0.27 (1.09) | 0.57 (-0.56) | |
| LE Distance manual PD (mm) | Mean difference | 0.05 | 0.55 | −0.06 |
| SD of difference | 0.83 | 0.72 | 0.82 | |
| P value (Z Wilcoxon value) | 0.57 (-0.55) | 0.11 (-1.57) | 0.68 (0.40) | |
| Binocular Distance manual PD (mm) | Mean difference | 0.06 | 0.27 | 0.01 |
| SD of difference | 0.94 | 1.04 | 0.93 | |
| P value (Z Wilcoxon value) | 0.49 (-0.68) | 0.52 (-0.63) | 0.74 (-0.32) | |
| Binocular Near manual PD (mm) | Mean difference | 0.15 | 0.08 | 0.17 |
| SD of difference | 1.04 | 1.63 | 0.88 | |
| P value (Z Wilcoxon value) | 0.16 (-1.37) | 0.75 (-0.31) | 0.15 (-1.42) | |
| RE Distance Pupillometer (mm) | Mean difference | −0.10 | −0.02 | −0.12 |
| SD of difference | 0.54 | 0.37 | 0.58 | |
| P value (Z Wilcoxon value) | 0.45 (0.74) | 0.65 (0.44) | 0.43 (0.77) | |
| LE Distance Pupillometer (mm) | Mean difference | 0.17 | 0.12 | 0.18 |
| SD of difference | 0.52 | 0.53 | 0.52 | |
| P value (Z Wilcoxon value) | 0.10 (-1.62) | 0.89 (0.13) | 0.07 (-1.79) | |
| Binocular Distance Pupillometer (mm) | Mean difference | 0.38 | 0.05 | 0.47 |
| SD of difference | 1.81 | 0.25 | 2.02 | |
| P value (Z Wilcoxon value) | 0.10 (-1.60) | 0.70 (-0.37) | 0.14 (-1.46) | |
| Binocular Near Pupillometer (mm) | Mean difference | 0.06 | 0.19 | 0.03 |
| SD of difference | 0.34 | 0.28 | 0.35 | |
| P value (Z Wilcoxon value) | 0.42 (-0.80) | 0.13 (-1.51) | 0.86 (-0.16) |
Inter-Session comparisons for all conditions.
| Correlation | Bland and Altman Agreement | % observations within clinical range of resolution | ||||
|---|---|---|---|---|---|---|
| rs | p | Mean difference (mean ± SD) | Mean difference + 1.96 SD | Mean difference - 1.96 SD | ||
| RE Distance manual PD (mm) | 0.89 | < 0.001 | −0.01 ± 0.58 | 1.12 | −1.15 | 97 |
| LE Distance manual PD (mm) | 0.81 | < 0.001 | 0.05 ± 0.83 | 1.68 | −1.57 | 87 |
| Binocular Distance manual PD (mm) | 0.91 | < 0.001 | 0.06 ± 0.94 | 1.91 | −1.77 | 87 |
| Binocular Near manual PD (mm) | 0.89 | < 0.001 | 0.15 ± 1.04 | 2.2 | −1.89 | 70 |
| RE Distance Pupillometer (mm) | 0.81 | < 0.001 | −0.10 ± 0.54 | 0.96 | −1.18 | 97 |
| LE Distance Pupillometer (mm) | 0.94 | < 0.001 | 0.17 ± 0.52 | 1.19 | −0.84 | 94 |
| Binocular Distance Pupillometer (mm) | 0.86 | < 0.001 | 0.38 ± 1.81 | 3.93 | −3.16 | 97 |
| Binocular Near Pupillometer (mm) | 0.99 | < 0.001 | 0.06 ± 0.34 | 0.74 | −0.61 | 100 |
Correlation, agreement, mean difference, and percentage of observations within the clinical range of resolution between sessions for all comparisons.
DiscussionThis study investigated the agreement and inter-session repeatability between manual and automatic IPD measurements. The findings are especially relevant for optometric practices that vary in their method of IPD measurements, and in which measurements are repeated on different days. Specifically, the automatic Essilor Pupiilon pupillometer was assessed, as it had not been assessed in previous agreement studies. We report that the IPD measurements using the two methods are significantly different statistically, but not clinically. Both methods were also found to obtain similar values between sessions.
Clinical significanceOne mm for monocular, and 2 mm for binocular PD measurements are reported to be acceptable inter-examiner variability as well as the acceptable tolerance for differences in IPD in spectacles.44 Differences between measurements that are smaller than 1 mm for monocular and 2 mm for binocular PD measures in this study were considered clinically insignificant. There is more clinical significance in IPD measurement errors for patients with higher refractive errors, with visual consequences such as asthenopia.47 Many subjects are unable to tolerate horizontal prismatic deviations larger than 2 prism diopters48 According to Prentice's formula, the deviation of the image in prism diopters is equal to the distance of the image from the optical axis in centimeters multiplied by the focal power of the lens in diopters.49 Based on this, a prismatic deviation of 2 prism diopters is obtained with an IPD decentration of 2 mm for refractive errors of 10 diopters and above.
Manual vs. Automatic binocular IPD measurementsManual measurements examine the anatomical location of the pupil, whereas the automatic measurements examine the physiological corneal reflex.1,23 The physical pupil, and specifically, the iris, are dynamic structures. As such, the corneal reflex has an intrinsic imprecision that cannot be eliminated.50 Despite this limitation, our findings show that the two measurements do not differ clinically in the majority of subjects. Nonetheless, our findings show that between 20%-30% of the subjects do differ clinically between these measurement methods.
The mean manual binocular distance IPD of the study participants ranged between 53 mm and 69 mm. The mean measurement was 60.6 ± 3.2 mm (female mean:60.0 ± 3.0, range: 53–67 mm, male mean: 61.9 ± 3.4, range: 55–69 mm).
The mean automatic binocular distance IPD of the study participants ranged between 52 mm and 68.5 mm. The mean measurement was 59.3 ± 3.4 (female:58.6 ± 3.1, range: 52.0–66.5, male: 61.0 ± 3.7, range: 53.5–68.5 mm).
The mean difference between the manual and automatic binocular distance measurements was lower than 2 mm for all participants, the female subgroup and the male subgroup. As such, these differences cannot be considered clinically significant.
As seen in Table 10, our IPD values are lower than reported in other studies around the world, with the exception of the female participants, who had distance IPDs similar to Saudi Arabian females.
Binocular IPD Measurements Reported by Previous Studies. For each study, the number of participants, ethnicity, and binocular IPD values are reported.
| Study Name | Number of Participants: | Measurement Method | Population Ethnicity | Distance Binocular (mm) | Near Binocular (mm) |
|---|---|---|---|---|---|
| Fledelius & Stubgaard55 | N Age: 21−80 = 187 | Exophthalmometry | Denmark hospital population | Femalesages: 20−24: IPD = 62 ± 2.6; ages: 25−30: IPD = 61.8 ± 3.1; ages: 31−55: IPD = 62.9 ± 3.5.Malesages: 20−24: IPD = 64.9 ± 3.5ages:25−30: 66.4 ± 2.3ages: 31−55: IPD = 66.4 ± 2.8 | ------ |
| Osuobeni and Faden4,52 | NFemales Ages 19−25 = 311NFemales Ages 26−55 = 353NMales Ages 19−25 = 272NMales Ages 26−55 = 418 | Viktorin's method | Arab (Saudi Arabia) | Femalesages 19−25: IPD = 60.3 ± 2.8 ages 26−40: IPD = 60.9 ± 3.0Malesages 19−25: IPD = 63.3 ± 2.9 ages 26−55: IPD = 64.8 ± 2.8 | Femalesages 19−25: IPD = 58 ± 2.8ages 26−40: IPD = 58.7 ± 3.0Malesages 19−25: IPD = 60.2 ± 2.7ages 26−40: IPD = 62 ± 2.6 |
| Holland & Siderov23 | N = 49 | Viktorin’s, corneal reflection, and pupillometer | Not stated | 61.7 (mean of two examiners) | ------ |
| Evereklioglu,Dognay,Hamdi, Gunduz,.54 | NFemales Ages 16−25 = 521NFemales Ages 26−55 = 135NMales Ages 16−25 = 582NMales Ages 26−55 = 166 | Viktorin's method | Turkish | Femalesages 16−25: IPD = 61.3 ± 2.7 ages 26−40: IPD = 62.2 ± 2.7Malesages 16−25: IPD = 63.6 ± 2.6 ages 26−55: IPD = 64.3 ± 3.0 | Femalesages 16−25: IPD = 58.4 ± 2.6ages 26−40: IPD = 59.2 ± 2.6Malesages 16−25: IPD = 60.2 ± 2.5. ages 26−55: IPD = 60.9 ± 3.0 |
| Pointer 3 | NFemale = 900 Nmale = 900 | Viktorin's method | Caucasian (white,Northern European) | Femalesages 16−25: IPD = 61.7 ± 2.7ages 26−40: IPD = 62.5 ± 2.8ages 41−65:IPD = 62.5 ± 2.7Malesages 16−25: IPD = 63.7 ± 3.4, ages 26−40: IPD = 65.2 ± 3.1, ages 41−65: IPD = 65.5 ± 2.8 | ------- |
| Mommaerts et al 56 | N = 50 | Nidek pupilometer | European Caucasian dysgnathic population | Female: IPD = 59.4 ± 2.3Male: IPD = 60.6 ± 4.6 | ------- |
| Esomonu, Taura, Anas, Modibbo24 | Neach subgroup = 500 | Viktorin's method | Igbo ethnic group,Nigeria | Femalesages 16−25: IPD = 74 ± 3.0ages 26−40: IPD = 74 ± 2.0Malesages 16−25: IPD = 74 ± 5ages 26−40: IPD = 75 ± 5 | Femalesages 16−25: IPD = 68.5 ± 3.3 ages 26−40: IPD = 68.8 ± 2.6Malesages 16−25: IPD = 67.9 ± 4.7ages 26−40: IPD = 68.4 ± 5 |
| Osunwoke, Didia, Olotu, Yerikema53 | Neach group = 88 | Viktorin's method | Ijaw ethnic group, Nigeria | Femalesages 18−21: IPD = 65.1 ± 2.7Malesages 18−21: IPD = 64.9 ± 3.3 | Femalesages 18−21: IPD = 62.1 ± 2.9Malesages 18−21: IPD = 62.2 ± 3.2 |
| Fesharaki et al 57 | N = 1500 | Autorefractor | Iran Hospital Patients | Femalesages 20−29: IPD = 60.7 ± 3.5ages 30−50: IPD = 61.2 ± 3.2age > 50: IPD = 62.0 ± 4.1Malesages 20−29: IPD = 63.2 ± 3.3ages 30−50: IPD = 63.5 ± 3.3age > 50: IPD = 64.2 ± 4.6 | ------- |
| Present Study | N = 199 | Viktorin's and pupillometry | Jews and Arabs, Israel | Femalesages:19−46: IPD = 60.6 ± 3.0Malesages 19−53: IPD = 61.9 ± 3.4 | FemalesAges 19−46: IPD = 56.5 ± 2.8Malesages 19−53: IPD = 60.0 ± 3.0 |
*This study reported IPD of children aged 1 month to 18 years whereas this study sample included adults. Therefore, only data from the 18 year-old age group is tabulated.
The mean manual binocular near IPD of the study participants ranged between 51 mm and 65 mm. The mean measurement was 57.1 ± 3.1 mm (female mean: 56.5 ± 2.8 mm, range: 50.5–63.0, male mean:58.6 ± 3.2 mm, range: 51.5–65.0 mm).
The mean automatic binocular near IPD of the study participants ranged between 48.5 and 65 mm. The mean measurement was 56.3 ± 3.3 mm (female mean:55.6 ± 2.9 mm, range: 48.5–63.5 mm, male mean: 58.0 ± 3.6 mm, range: 51.0–65.0 mm).
The mean difference between the manual and automatic binocular near measurements of the cohort were lower than 2 mm for all participants, the female subgroup and the male subgroup. As such, these differences cannot be considered clinically significant.
As seen in Table 10, these measurements are lower than reported in other studies around the world, with the exception of the male participants who had near IPD similar to Turkish males.
Similar to some studies,1,23 but in contrast with another,38 the present study found wider binocular IPD measurements using the manual as opposed to the automatic measurement method. These differences, though not clinically significant, have been attributed to the fact that automatic and manual measurements are based on different points of reference.1 Automatic measurements are based on the locations of the corneal reflexes, which essentially measure the visual axes.51 The corneal reflex generally is offset nasally with respect to the pupillary center.3 Manual measurements are based on anatomical locations, of either the pupil or the limbus. As such, differences between the two methods are to be expected.
The mean difference between the manual distance and near IPD measurements in the present study is 3.5 mm for females and 3.3 mm for males. The mean difference between the automatic distance and near IPD measurements is 3.0 mm for females and 3.1 for males. These differences between distance and near IPD are substantially smaller than the 5.0 mm differences reported by Esomonu et al.24 and 4.4 mm differences reported by AlAnazi et al.,38 and larger than the 2.0 mm differences reported by Osuobeni & Faden.4,52 However, the differences in our cohort are similar to the 3.0 mm differences reported by Osunwoke et al.53 and 3.0–3.5 mm differences reported by Everklioglu et al.54 Discrepancies between the present study and Esomonu et al.24 could be attributed to the distance IPDs. As stated in the introduction, the vergence demand is dependent on the IPD,22 and their subjects had a much larger distance IPDs than our cohort. The discrepancy with the results of AlAnazi et al.38 can be attributed to the large variation in their subjects. They reported that the differences between distance and near IPDs in their subjects varied from 2.2 mm to 6.6 mm.
Manual vs. Automatic monocular PD measurementsAs indicated earlier, monocular PD measurements are indicated in cases of craniofacial surgery43 unequal pupillary locations due to facial asymmetry,42 progressive lenses,18,39 and spectacles with prisms.40 However, to the best of our knowledge, monocular PD is not commonly studied and is rarely reported in the literature. Therefore, the present study also compared the monocular PD determined by the manual and automatic methods.
The mean manual right distance PD of the study participants ranged between 27 mm and 35 mm. The mean measurement was 30.4 ± 1.7 mm (female mean:30.1 ± 1.6, range: 27.0–34.8 mm, male mean: 31.4 ± 2.0, range: 27.5–35.0 mm).
The mean automatic right distance PD of the study participants ranged between 25.5 mm and 36.0 mm. The mean measurement was 29.6 ± 1.9 mm (female mean: 29.4 ± 1.7, range: 25.5–36.0 mm, male mean: 30.4 ± 2.1, range: 26.5–34.5 mm).
The mean difference between the manual and automatic right eye measurements is less than 1 mm for the entire cohort as well as the female sub-group. The mean difference of the male sub-group was 1 mm. These mean differences are considered insignificant clinically.
The mean manual left distance PD of the study participants ranged between 25.5 mm and 35 mm. The mean measurement was 29.9 ± 1.5 mm (female mean:29.7 ± 1.5, range: 25.5–34.0 mm, male mean: 30.4 ± 1.6, range: 27.0–35.0 mm).
The mean automatic left distance PD of the study participants ranged between 25.5 mm and 34.5 mm. The mean measurement was 29.7 ± 2.0 mm (female mean: 29.2 ± 1.8, range: 25.5–34.0 mm, male mean: 30.7 ± 2.0, range: 26.5–34.5 mm).
The mean difference for all the comparisons is lower than 1 mm and considered clinically insignificant.
The monocular PDs of the right and left eyes, as measured with both methods, were slightly asymmetric. Specifically, the PD of the right eye of 114 participants (57%) was wider than the PD of the left eye. Facial asymmetries between the two halves of the face are not uncommon.58
Gender variationsThere was a significant difference between the mean age of the female (mean age: 23.7 ± 4.6, range: 19−46) and male participants (mean age: 25.5 ± 5.0, range: 19−53) of this study. The mean difference in age was 1.8 years. Although IPD has been shown to vary with age24,38,54 data typically are grouped in intervals of 10 years, and both the females and males in our cohort would have been grouped within the same age interval. Additionally, the IPD typically stabilizes in adults within the second decade of life.59,60 Therefore, we can assume that variations in IPD between the two sub-groups are linked with gender and size more than they are linked with age differences.
In the present study, male and female distance binocular manual and automatic measurements differed by 1.9 mm and 2.4 mm respectively. The near binocular manual and automatic measurements differed by 2.1 mm and 2.4 mm respectively. Given the clinical range of agreement of 2 mm for binocular measurements, aside from the distance manual measurements, the mean differences between the female and male participants are clinically significant. As seen in Table 10, the differences between female and male IPDs reported in this study are similar to studies from other regions around the world.
Ethnic differencesThe current study included 199 Israeli adults. Compared to the Bura ethnic group of North-Eastern Nigeria whose mean distance and near IPDs, measured manually, are 73.1 ± 2.8 and 67.1 ± 2.7, respectively, the IPDs of Israeli population are much narrower.61 Israeli IPDs also are narrower than reported distance IPD values for African Americans (64.1 mm12 and 66.3 mm62), Chinese males and females (64.6 mm and 61.3 mm, respectively63), Turks (62.5 ± 4.1 mm64) and European Caucasians (62.9 ± 3.455). The IPD of the Israeli population appears to be similar to the Arab population (60.9 ± 3.0 in females and 62.0 ± 2.6 in males4), which could be due to the fact that our cohort included 53 Israeli Arabs and that the two ethnic groups are genetically similar.65,66
Inter-session repeatabilityThere was no significant statistical or clinical difference between the sessions for all conditions. In the Bland and Altman analysis, 87% or more of the observations for all conditions were within the clinical range of resolution (±1 mm), except for the manual near binocular IPD. In this condition, nine of the manual near binocular IPD measurements differed by more than 1 mm between the first and second sessions. In other conditions, a maximum of four participants differed by more than 1 mm between the sessions.
Limitations of this studyThis study has some limitations. First, as tabulated in Table 10, some previous studies examined larger cohorts,3,4,24,52–54 although the present study includes more participants than some of the other studies.55,56
The current study has an imbalanced gender cohort, with 58 males and 141 females. Accordingly, the IPDs of the male sub-group have higher standard deviations than the female sub-group, though the mean differences in standard deviations are all lower than 1 mm and are not clinically significant. If the standard deviations are proportional to the mean IPD, males would be expected to have slightly larger standard deviations than females. Some, though not all of the studies listed in Table 10 reported larger standard deviations for males than female IPDs.
Two outcome measures reported in this study (Table 2) did not include the entire cohort. The stereoacuity of three female participants, and the binocular near VA of four males and 22 females were missing. As mentioned in the methods, these parameters were measured as part of a vision screening. It is possible that not all participants completed all the stations. The main outcome measures of the study are the manual and automatic binocular and monocular PD measurements. These values were reported for the entire cohort. The near VAs were missing for two subjects aged 20, and two subjects aged 25. The distance decimal VAs for these subjects were 0.8, 0.67, 1.00 and 1.00, respectively. Given the fact that the subjects are all pre-presbyopic, their near VA is also expected to be within normal limits. This assumption is further supported by the fact that their stereo-thresholds were lower than 70″ (the mean stereopsis of these four participants: 44″ ± 21″). Stereopsis requires similar values of good visual acuity in the two eyes.67 Furthermore, in IPD measurements, subjects are asked to either view the examiner’s eye (manual) or a circular large target (automatic). These large visual targets do not require very precise visual acuity. As such, we can assume that the missing outcome measures do not affect our conclusions.
The distribution of IPD values in our study was found not to be normally distributed based on statistical tests. We would have expected a normal distribution of IPD values in a wide range of ages. Given the age range in our cohort (ages 19−46 for the females and 19−53 for the males), in which the IPD is expected to stabilize without much change59,60 our results are not surprising. These findings are also consistent with other studies reporting a non-normal distribution of IPD.57 Based on the non-normal distribution, the agreement of the two IPD measurement methods was assessed using the Bland and Altman analysis of non- normally distributed data.46 This analysis includes the application of a clinical range of resolution as opposed to the calculated 95% limits of agreement. In our data, the clinical range of resolution was smaller than the calculated 95% limits of agreement for all comparisons. As a result, a smaller proportion of observations were found to fall within the resolution limits. Additionally, Bland and Altman consider two measurement methods interchangeable if only three observations fall outside the limits of agreement.45 This was not the case for all conditions (monocular RE and LE and binocular distance and near IPD). We state this as a potential limitation though based on the fact that a vast majority of the observations were well within the clinical resolution limit, we concluded that the measurements were interchangeable.
Another potential limitation is the fact that the Essilor Pupillon pupilometer does not provide the individual values of the four measurements and only displays the mean of the consecutive measurements. This does not allow examination of the intra-test repeatability of the pupillometer. Furthermore, if three consecutive measurements are to be taken by the experimenter in order to assess the intra-test repeatability, in reality 12 measurements are taken. This would have potentially introduced a bias in the results (12 measurements in one instrument compared to four with the ruler). In addition, the four consecutive pupillometer measurements are time consuming, especially relative to ruler measurements, thereby affecting patient cooperation and the measurements.
ConclusionsMean differences between manual ruler and automatic Essilor pupillometer measurements are not clinically significant. Mean differences between distance and near IPD were approximately 3 mm. Female IPDs are approximately 2 mm narrower than male IPDs. The mean IPD in our cohort was similar to values reported previously. Both manual and automatic methods of measurement present good inter-session repeatability.
FundingThis study was partially funded by a grant by IRISS Medical Technologies Ltd., UK.
DeclarationsThe authors have no competing interests to declare
Data availability statementThe datasets generated during and/or analysed during the current study are available from the corresponding author on reasonable request.
We would like to thank Profs. Harold Bedell and Ariela Gordon-Shaag for helpful suggestions, Prof. Avi Besser for statistical advice, and Drs. Joan Gispets Parcerisas and Judy Kupersmith for assistance with the abstract. We thank Dr. Simon Barnard, Vanessa Elbaz, Ruth Wolff, Gabrielle Chiche, Rasha Ghantous, and Medicha Duchi for assistance with the vision screenings, and Ms. Oralie Assayag for assistance with the inter-session repeatability study.
Manual IPD Measurement using a specially marked ruler. The ruler is placed on the bridge of the nose in the center of the subject's face, approximately in the back vertex plane of the spectacle lens. Demonstrated is the near IPD measurement with the examiner closing his left eye and asking the subject to fixate on the examiner's open right eye. The examiner notes the location of the center of the subject's right eye pupil. Then the examiner opens the left eye and closes the right eye. The subject is asked to fixate on the right eye and the examiner notes the location of the center of the subject's left eye.