To calibrate the new ZEISS VisanteTM anterior segment optical coherence tomographer (OCT) using references with known physical thickness and refractive index equal to the human cornea and to compare the Visante measures to those from a previous generation OCT (Zeiss-Humphrey OCT II).
MethodsTwenty two semi-rigid lenses of specified thicknesses were manufactured using a material with refractive index of 1.376. Central thickness of these lenses was measured using VisanteTM and Zeiss-Humphrey OCT II OCT's (Zeiss, Germany). Two data sets consisting of nominal measures (with a standard pachymeter) of the lenses and one obtained using a digital micrometer was used as references. Regression equations between the new physical and optical (OCT) measures were derived to calibrate the devices.
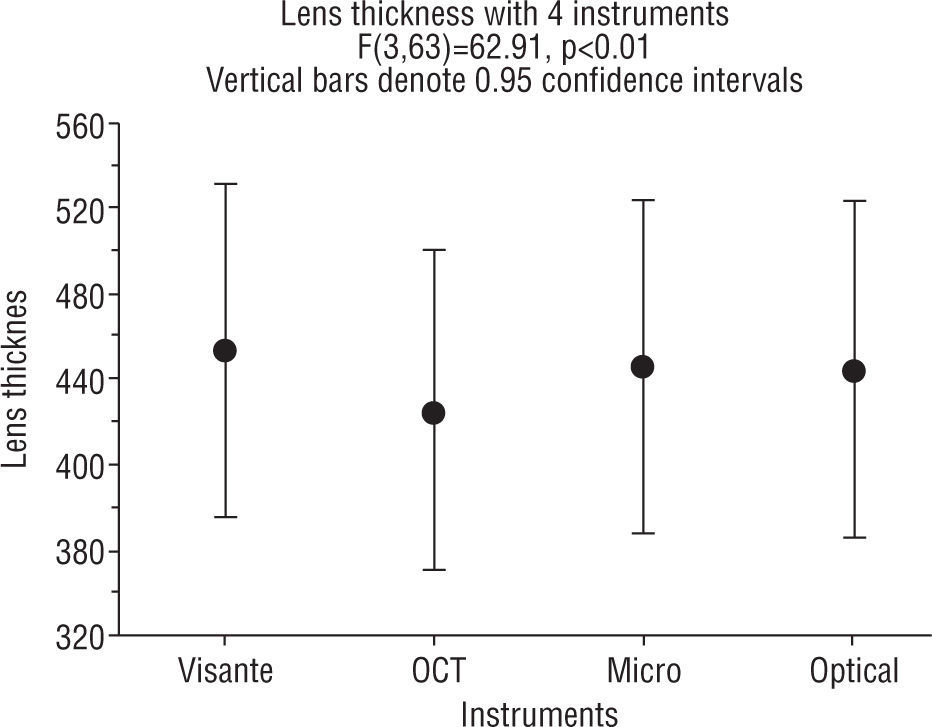
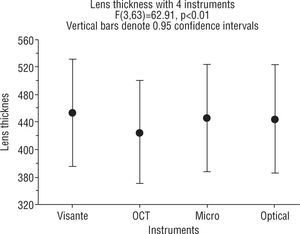
ResultsBefore calibration, repeated measures ANOVA showed that there were significant differences between mean lens thicknesses from each of the measurement methods (p<0.01), where Visante measurements were significantly different from the other three (OCT II, MG and OP) methods (p<0.001). Visante thickness was significantly higher than the microgauge measures (453±37.6 compared to 445.1±38.2) and the OCT II was significantly lower (424.5±36.1 both, p<0.001). After calibration using the regressions between physical and optical measurements, there were no differences between OCT II and Visante (p<0.05).
ConclusionsUsing references lenses with refractive index of the cornea (1.376) allows rapid and simple calibration and cross calibration of instruments for measuring the corneal thickness. The Visante and OCT II do not produce measurements that are equal to physical references with refractive index equal to the human cornea.
Calibrar el nuevo tomógrafo de coherencia óptica (OCT) del segmento anterior ZEISS VisanteTM utilizando referencias con índice de refracción y espesor físico conocido equivalentes a la córnea humana y comparar las medidas del Visante con las del OCT de la generación anterior (Zeiss-Humphrey OCT II).
MétodosSe fabricaron 22 lentes semirrígidas de espesores específicos utilizando un material con un índice de refracción de 1,376. El espesor central de estas lentes se midió con los OCT VisanteTM y Zeiss-Humphrey OCT II (Zeiss, Alemania). Como referencias se utilizaron dos conjuntos de datos compuestos de medidas nominales (con un paquímetro estándar) de las lentes, uno de ellos obtenido mediante un micrómetro digital. Para calibrar los dispositivos se derivaron las ecuaciones de regresión entre las nuevas medidas físicas y ópticas (OCT).
ResultadosAntes de la calibración, las mediciones repetidas con el ANOVA mostraron que había diferencias significativas entre las medias de espesor de la lente a partir de cada método de medición (p<0,01), en los cuales las mediciones con Visante fueron significativamente diferentes de los otros tres métodos (OCT II, MG y OP) (p<0,001). El espesor con Visante fue significativamente mayor que en las mediciones con micrómetro mecánico (453±37,6 en comparación con 445,1±38,2) y con el OCT II fue significativamente inferior (424,5±36,1 ambos, p<0,001). Después de la calibración utilizando las regresiones entre las mediciones físicas y ópticas, no hubo diferencias entre el OCT II y el Visante (p<0,05).
ConclusiónEl uso de lentes de referencia con índice de refracción equivalente al de la córnea (1,376) permite calibrar e intercalibrar rápida y fácilmente los instrumentos para medir el espesor corneal. El Visante y el OCT II no proporcionan mediciones equivalentes a las referencias físicas con un índice de refracción equivalente al de la córnea humana.
The measurement of corneal thickness has various important clinical and research applications. Some of these may be to measure corneal swelling after overnight wear of continuous wear contact lenses,1 after overnight orthokeratology,2 or to monitor thickness changes in patients with thinning disorders such as keratoconus3 or for refractive therapy techniques.4,5 Corneal thickness can be measured optically6,7 or using ultrasound techniques.8,9 One of the advantages of optical measures over ultrasound is the non-contact nature of the technique. Despite the reported accuracy of ultrasound measures, corneal contact and with the use of anaesthetics makes this methods more inconvenient.10,11 Also, the indentation of the cornea has resulted in an under-estimation of corneal thickness when compared to other methods.11
Optical Coherence Tomography (OCT) is a newer non-contact optical imaging technique that can measure biological tissue thickness with higher nominal resolution, ranging from 2 to 20 microns.12–16 OCT works on the Michelson interferometry principle and images are typically two-dimensional data sets which represent optical backscattering in a cross-sectional plane through the tissue.17,18 OCT (TdOCT) has been useful in the visualization of different ocular tissues including the cornea.12 Its main disadvantage is a longer acquisition time causing a decrease in image quality and thus limiting its clinical applications. On the other hand, the spectral OCT (SOCT) has a shorter acquisition time eliminating many of the motion artifacts currently commercial available instruments have also been used for cross sectional imaging of the cornea.12,19–21
Previous work has suggested that corneal and particularly epithelial thickness can be measured using the Zeiss-Humphrey retinal OCT II (model 2010, Zeiss Humphrey systems, Dublin, CA), a posterior segment instrument, that has been a dapted to measure the anterior segment.22–24 The OCT II uses a super-luminescent diode as a low-coherence light source with the wavelength of 830–850nm and the band width of 32nm. The axial resolution is about 10–15 microns.25 A scan width of 1.13mm was used for the OCT II tomographer.
Similarly, a recently marketed anterior segment OCT instrument, the VisanteTM OCT (Zeiss Meditec, Dublin, CA) calculates corneal thickness throughout the entire corneal surface (in eight meridians simultaneously) which would be advantageous in characterizing areal corneal thickness.26,27 The VisanteTM OCT is a time-domain OCT and produces high resolution images of the entire anterior segment and was used in this study.28–31 The VisanteTM OCT uses a wavelength of 1310nm. This longer wavelength of the VisanteTM OCT allows better delineation of the anterior and posterior surfaces of the cornea and helps in better penetration past the limbus and the sclera. Its high speed scanning system enables the generation of pachymetry maps, in addition to linear cross-sectional images, in seconds. The axial resolution of the image is 18μm and the transverse resolution is 60μm. The tissue depth for each scan is 6mm deep by 16mm wide for anterior segment scans, 3mm deep by 10mm wide for the pachymetry.26,29,30
Anterior segment OCTs are now more commonly being used for a range of diagnostic and post-surgical analyses.7,32–35 For instance, there are a number or reports of the assessment of patients prior to specific surgical procedures and postsurgical evaluation of surgical outcomes such as corneal oedema and ectasia.7,36–40
Despite strong associations among measurements of corneal thickness using various measurement techniques,10,27,41 there is no gold standard to cross calibrate these instruments and to assess their accuracy, though attempts have been made.42,43
Although there is abundant literature on the precision of instruments measuring corneal thickness,44,45 no information about the accuracy of the methods exists. There are a number of reports comparing various methods of measuring corneal thickness.10,23,27,41,46
A clinician can make clinical decisions based on the repeatability and accuracy of the measures. Measurements could be repeatable and not accurate and therefore, in addition to precision a measurement technique should also be demonstrably accurate. The purpose of this study was first, to measure the accuracy of the Visante OCT as it compared to a direct measure with callipers (mechanical gauge [MG]) of a transparent plastic material with refractive index similar to the cornea, that is n=1.376.
The second purpose was to compare these results with an Optical Pachymeter (OP) and the Zeiss-Humphrey retinal OCT II. In order to calibrate the two OCT's (Visante OCT and Zeiss-Humphrey retinal OCT II) the measurements using the MG were taken as true measurements.
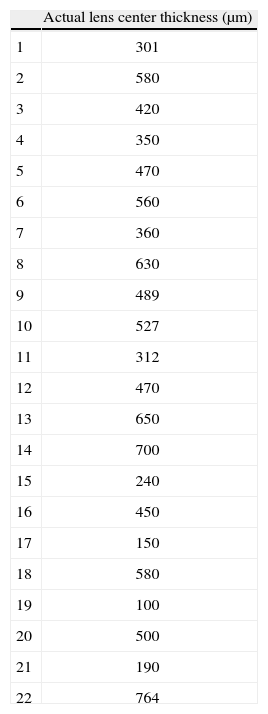
MethodsLensesTwenty two semi-rigid lenses with varying thicknesses were manufactured using a plastic material with a refractive index of 1.376±0.0005 (at 589nm). The refractive index of the material was verified with the manufacturer. This plastic material was developed by Optical Polymer Research, Inc., Gainesville, Florida. All the lenses were made with plano power (parallel anterior and posterior surfaces) with a base curve of 8.6mm and no prism. The physical center thickness of the calibration lenses (ranging from 100 to 764μm) were measured four times and then averaged (Table 1).
InstrumentationThe central thicknesses of the same set of lenses were also measured using the following three instruments: a computerized optical pachymeter (OP) mounted onto a Zeiss 30 SL-M biomicroscope, Zeiss-Humphrey retinal OCT II (Zeiss Meditec, Germany), and VisanteTM OCT (Zeiss Meditec, Germany).
With the VisanteTM OCT the “high resolution” mode was used in the scanning session for the semi-rigid contact lenses to optimise visualization. The corneal image of the VisanteTM OCT comprises 512 axial scans. The scan dimensions for this scan mode were 10mm length (512 A-scans) and 3mm (in tissue) depth.
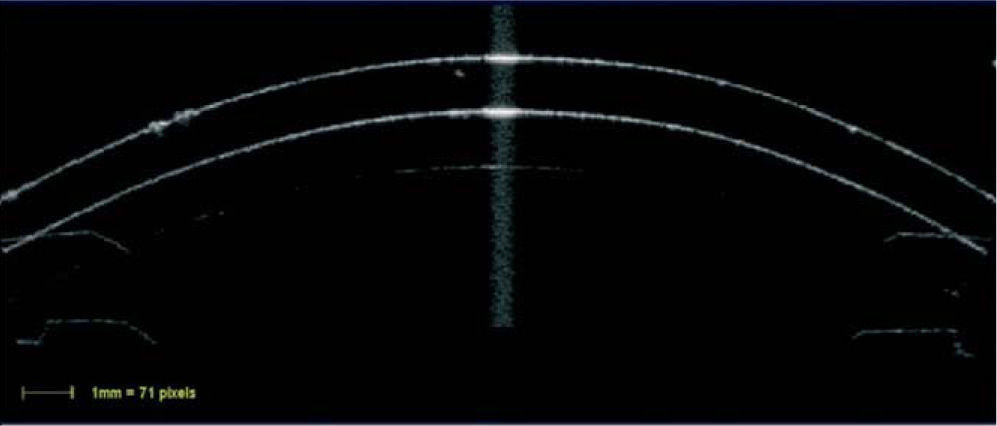
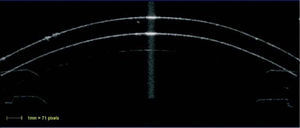
The scanned image was considered to be optimally aligned when the specular reflex, which is a high intensity reflection from the center of the front surface of the contact lens (Figure 1), was visible on the screen.
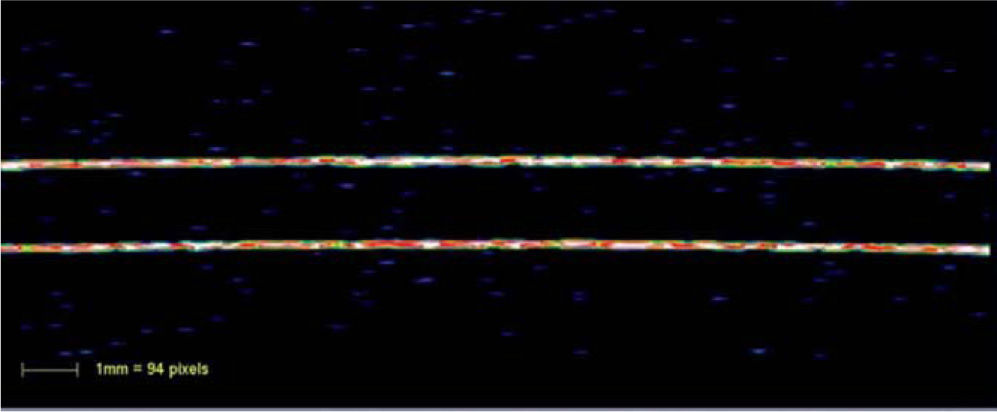
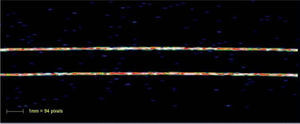
Acceptable scans were selected as soon as they appeared and images were judged to be of adequate quality based on the following criterion: good demarcation of the anterior and posterior boundaries of the contact lens and absence of artefacts. Instead of using the built in callipers provided by the instrument, custom software was used which automatically delineated the anterior and posterior borders of the cross-sectional images of the contact lens using the reflectivity plot produced by the instrument and then, the radial distance between the anterior and posterior surface were obtained, that is, the central thickness of the contact lens. The version 2.0 VisanteTM software was used and the raw unaltered binary image file (*.bin) was used to export the VisanteTM data for analysis. To convert pixels obtained from the binary image, to millimeters, a conversion factor was used (71 pixels=1mm). With the Zeiss-Humphrey retinal OCT II similar methods were used where one hundred axial scans (1.13-mm width) were processed and the central contact lens thickness was obtained using the same custom analysis software. Custom software read the raw files consisting of position vs. reflected intensity for each of the 100 sagittal scans (Figure 2).
The software imports the raw data from the instrument and then located the peak reflectance's that corresponded to front and rear lens surfaces. From the curves fit to these surfaces thicknesses (the shortest distance to the posterior surface) were calculates for each pixel point along the front surface. The averages of these thicknesses were then used.
The software imports the raw data from the instrument and then located the peak reflectance's that corresponded to front and rear lens surfaces. From the curves fit to these surfaces thicknesses (the shortest distance to the posterior surface) were calculates for each pixel point along the front surface. The averages of these thicknesses were then used.
ProcedureThe lenses were installed on a circular holder in a random order. A number was assigned to each with no reference to the thickness of the lens. All the measurements with the mechanical gauge (MG), optical pachymeter (OP) mounted onto a Zeiss 30 SL-M biomicroscope, Zeiss-Humphrey retinal OCT II and VisanteTM were performed by the first author. All the lenses were measured four times with the Zeiss-Humphrey retinal OCT II and VisanteTM OCT and the average of the four readings was taken and are reported in the results. Multiple measurements were necessary in order to minimize measurement variability.44,47 The measurement order with the instruments was randomized in the study.
The accuracy of the measurements of the two OCT instruments was determined by comparison of the physical CT of the lenses obtained using the mechanical gauge (MG) and the optical pachymeter (OP) with the OCT instrument measures.
Data analysisUsing a repeated-measures analysis of variance, the effects of measurement devices were examined. P values<0.05 were considered statistically significant. Tukey post hoc paired tests (significant level p<0.05) were used to determine the significance of specific pairs. Regression equations between the MG and both OCT measures were derived to calibrate the devices. The Bland & Altman recommendations were used to show the limits of agreement between pre and post calibration.48
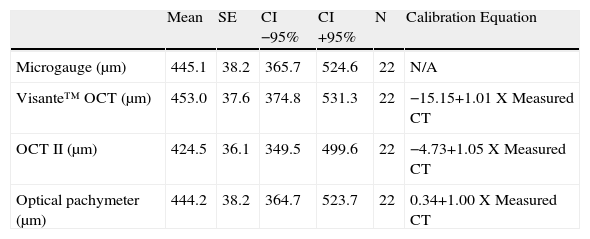
ResultsWith repeated measures ANOVA there was a significant difference in the lens thickness among all the methods of measurement before calibrating the instruments, as shown in Figure 3. Tukey post hoc tests revealed that the VisanteTM OCT measurements were significantly higher than the other three (OCT II, OP and MG) methods (p=0.001). The Visante thickness was 453.0±37.6 compared to 445.1±38.2 with the microgauge and the OCT II was significantly lower (424.5±±36.1) compared to the other three methods of measurement (both, p=0.001). There was no statistically significant difference (p>0.05) in thickness obtained using the microgauge (445.1±38.2) and the optical pachymeter (OP) (444.2±38.2).
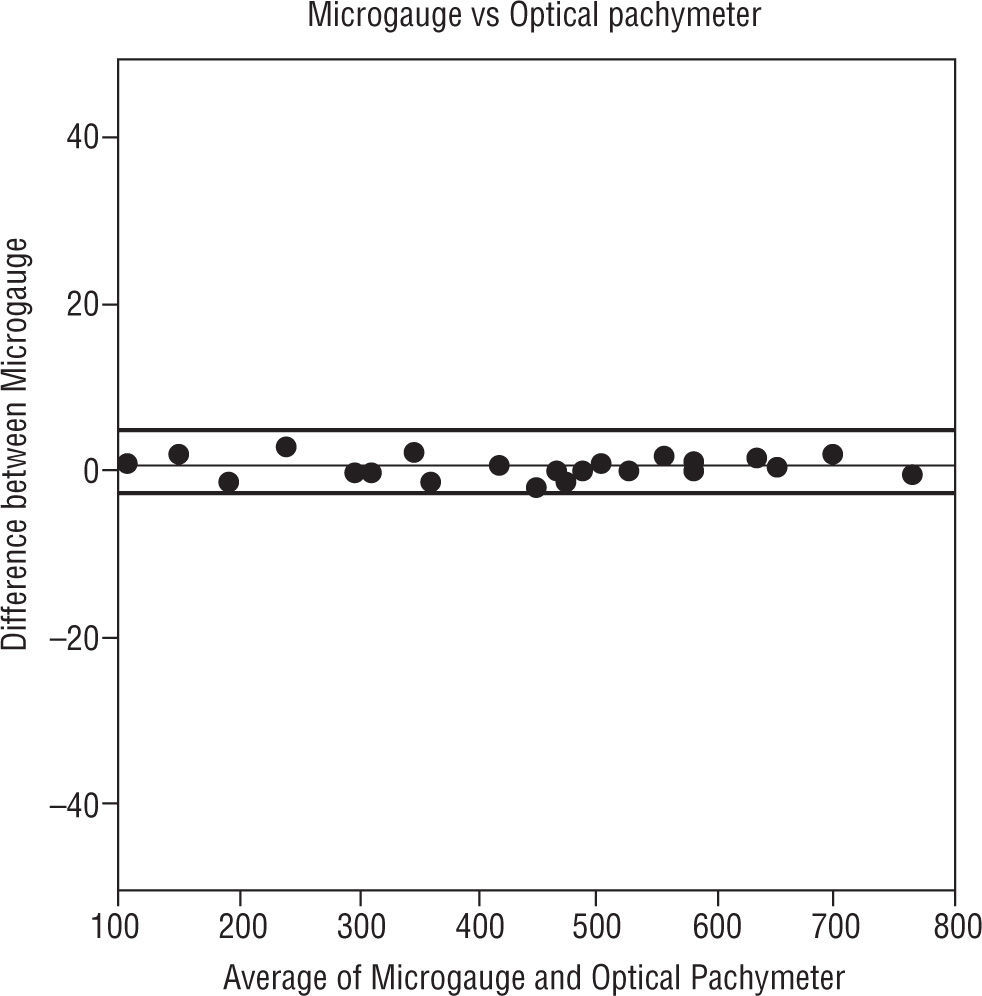
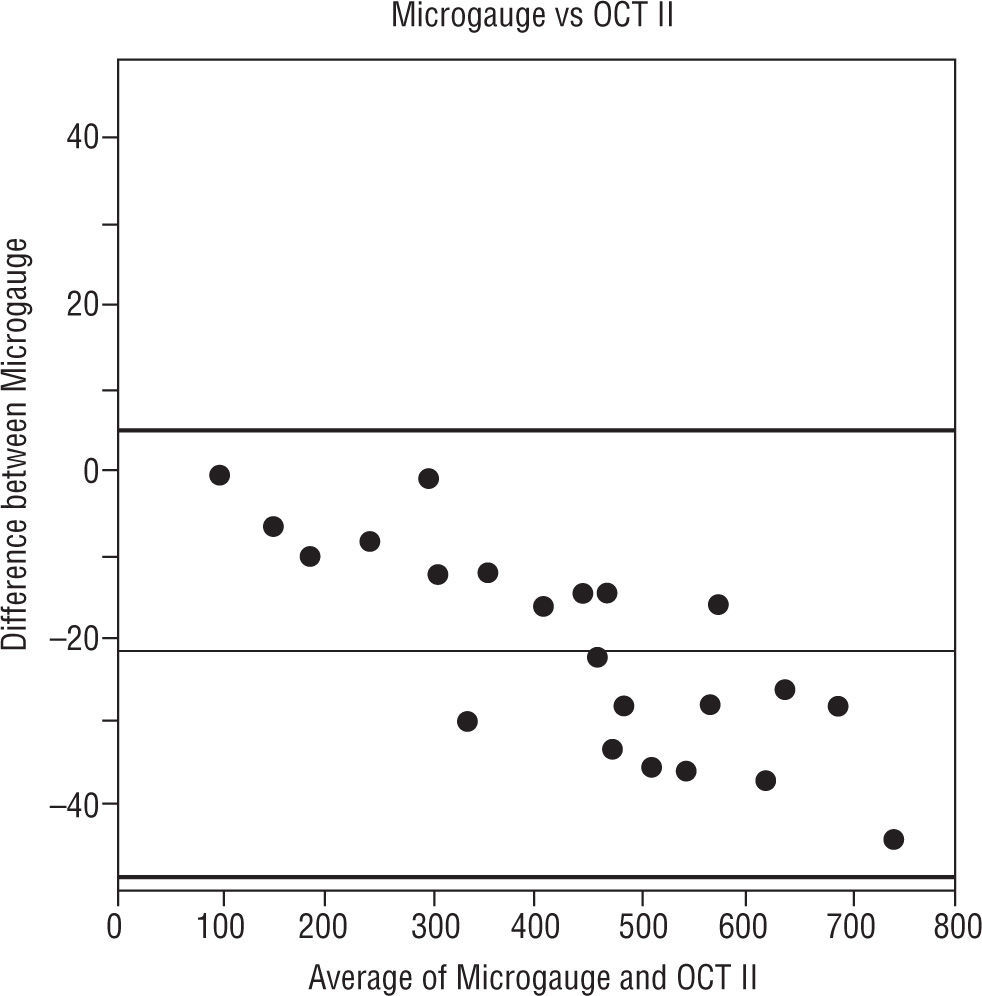
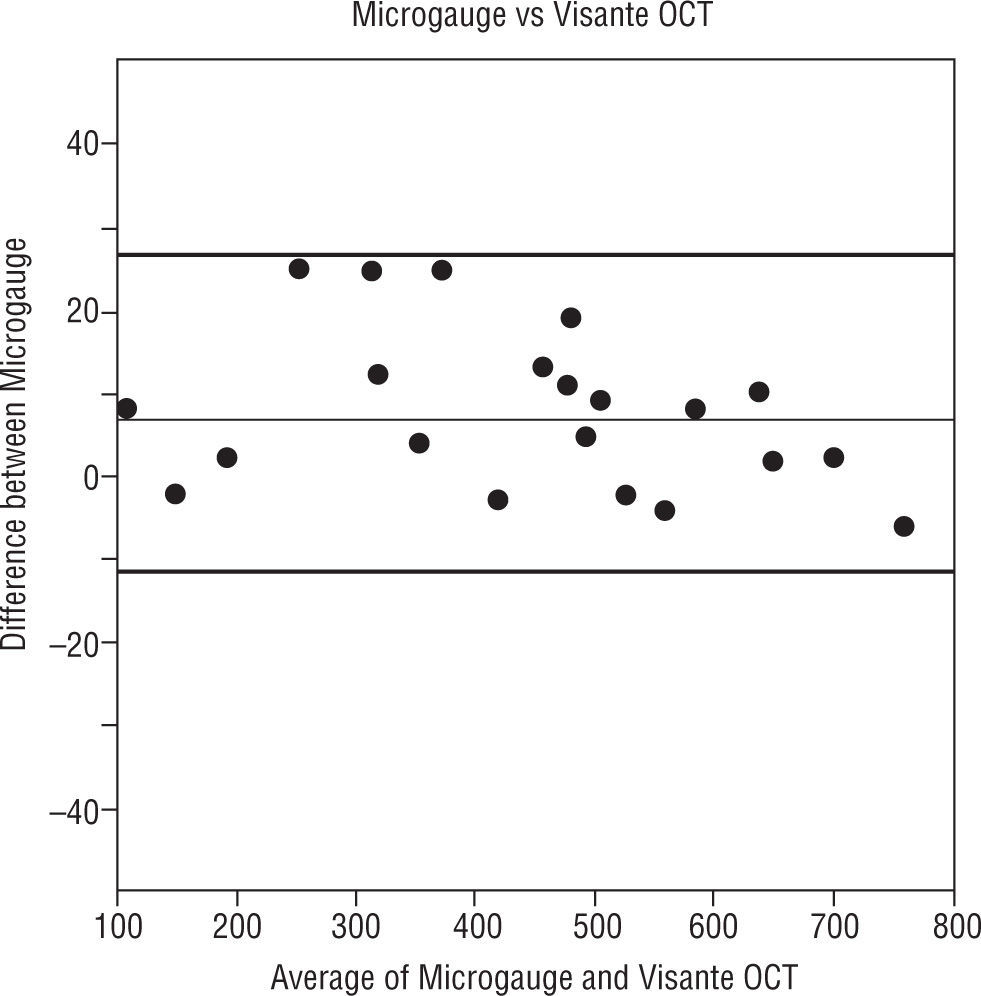
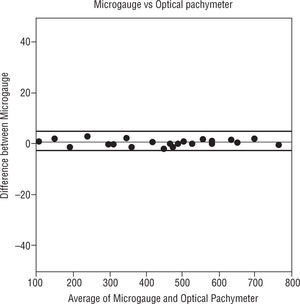
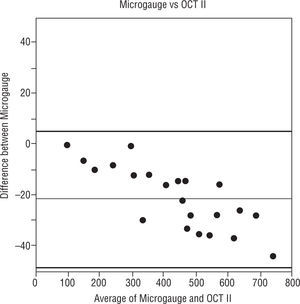
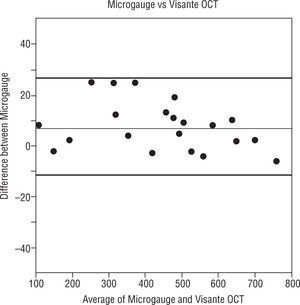
The Figures 4, 5 and 6 compare the standard microgauge measures to each of the measurements made by the three instruments (using Bland-Altman plots). Figure 4 compares the microgauge versus the optical pachymeter before calibration and shows that there was no difference. Figure 5 demonstrates the differences comparing the OCT II and the microgauge for all lenses and indicates that the thickness of thicker lenses (450μm and up) were over-estimated by the instrument. On the other hand, the Visante (Figure 6) when compared to the microgauge under-estimated the thickness especially when lenses were thinner (250 to 400μm).
Bland-Altman plot. The distribution of means of microgauge and optical pachymeter versus the distribution of differences between the microgauge and optical pachymeter. The thin line in the figure represents the mean difference and the thick lines in the figure represent the 95% limits of agreement.
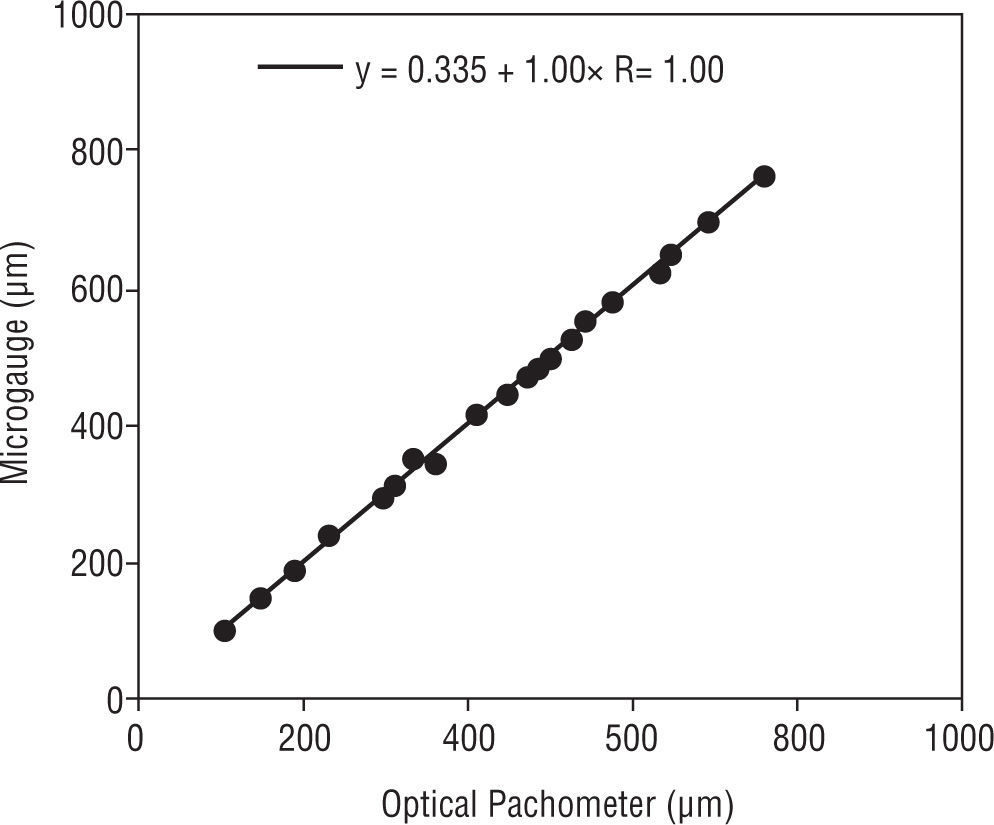
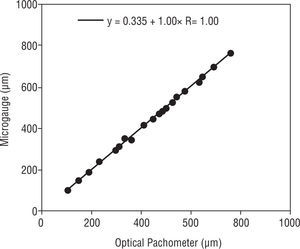
Regression equations between the OP measurements and the lens thickness measurements from the MG showed that there was a statistically insignificant difference (p>0.05) (Figure 7).
The MG measurement was taken as the “true” measurement for the following comparisons.
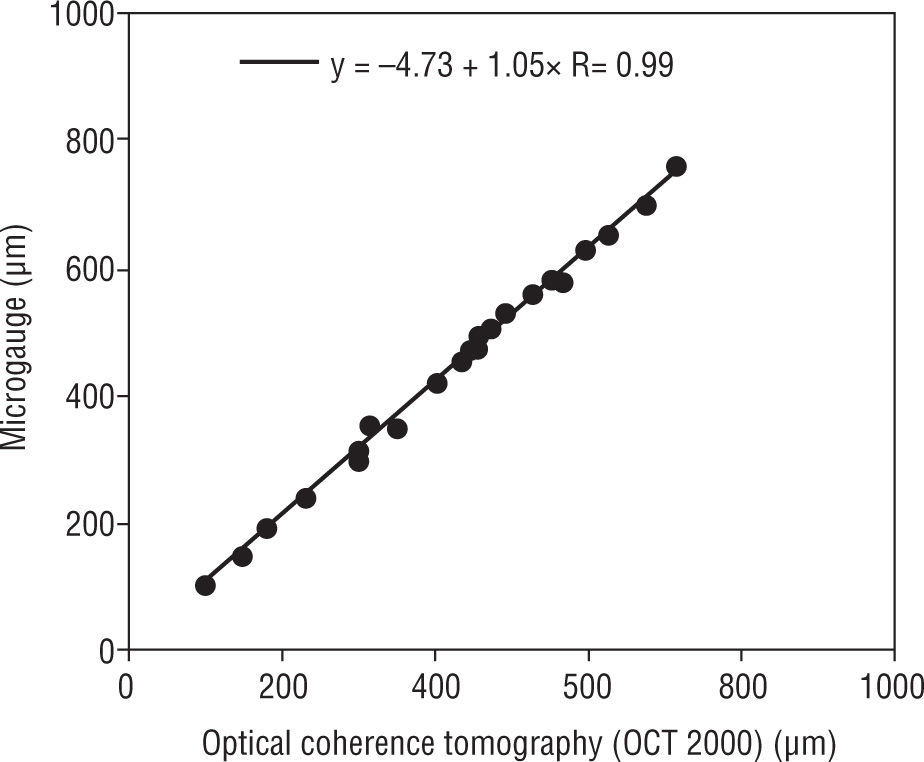
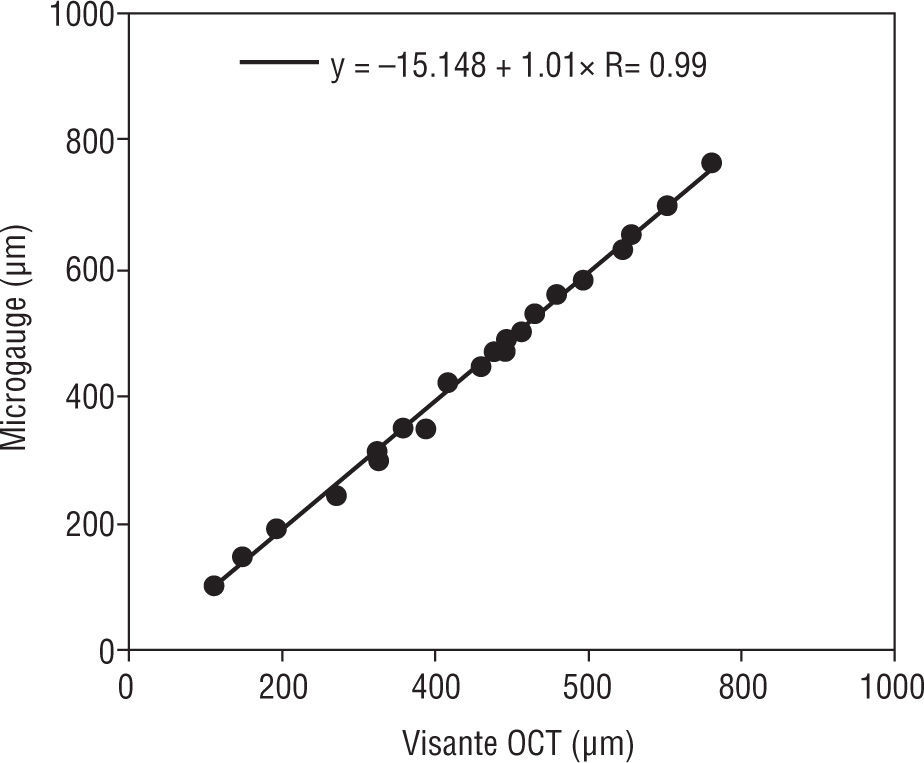
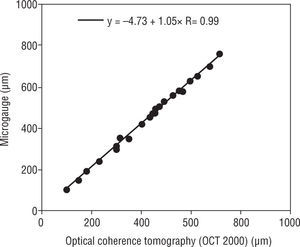
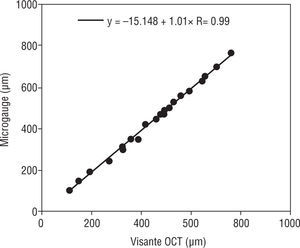
The correlations of pre calibrated Humphrey retinal OCT II and the VisanteTM versus the MG were estimated. The pre calibrated Humphrey retinal OCT II and VisanteTM OCT were significantly correlated (R=0.99, for both) when compared to the microgauge (p=0.001) (Figures 8 and 9).
The calibration equations that were derived from the regression analysis were then used to calibrate the instruments.
The differences between the two OCT instruments and the MG were eliminated after applying the calibration equations to each of these devices (Table 2).
The average centre thicknesses of the twenty-two lenses for each of the instruments tested and the respective calibration equations.
| Mean | SE | CI −95% | CI +95% | N | Calibration Equation | |
| Microgauge (μm) | 445.1 | 38.2 | 365.7 | 524.6 | 22 | N/A |
| Visante™ OCT (μm) | 453.0 | 37.6 | 374.8 | 531.3 | 22 | −15.15+1.01 X Measured CT |
| OCT II (μm) | 424.5 | 36.1 | 349.5 | 499.6 | 22 | −4.73+1.05 X Measured CT |
| Optical pachymeter (μm) | 444.2 | 38.2 | 364.7 | 523.7 | 22 | 0.34+1.00 X Measured CT |
These equations are not general equations for the devices. These equations are specific for individual instruments. CT, center thickness
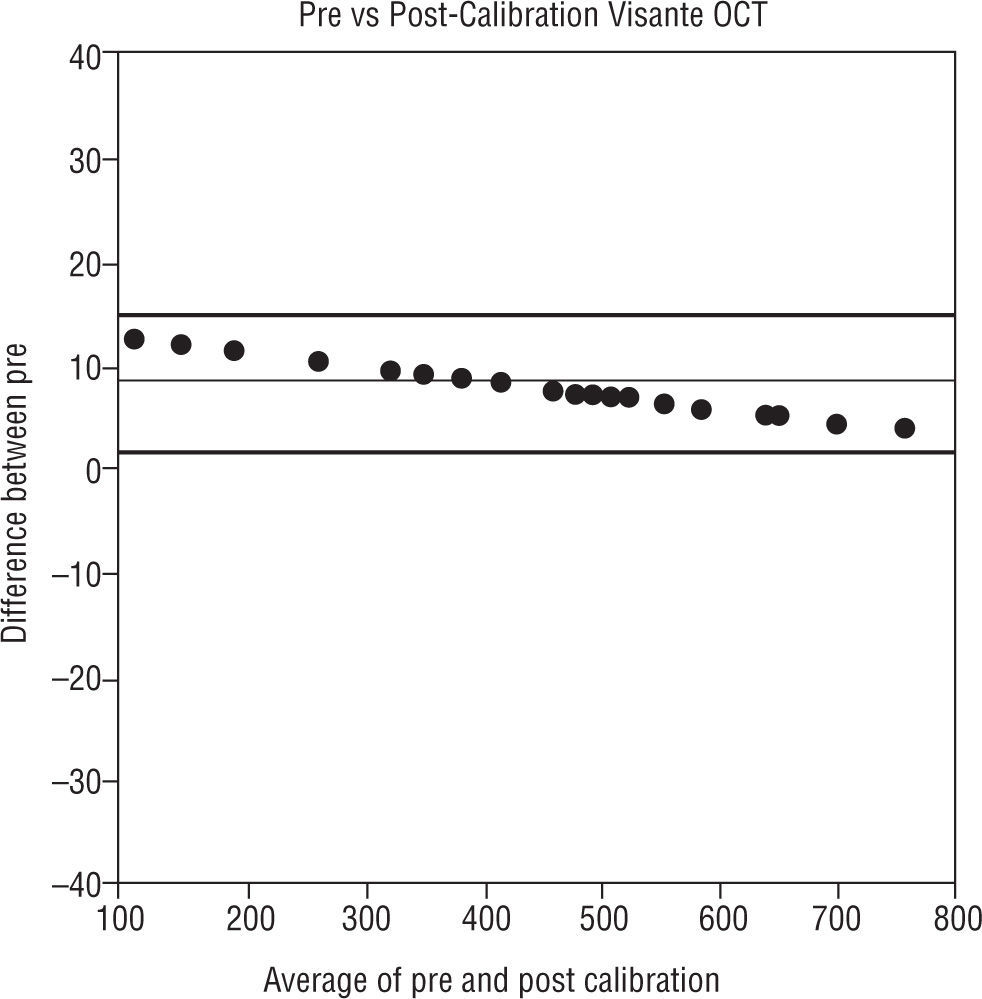
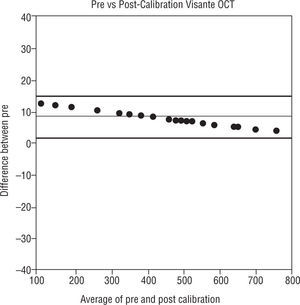
The difference between pre and post calibration versus the average of the pre and post calibration thickness values are shown in Figure 10.
Bland-Altman plot. The distribution of means of pre and post calibrated Visante OCT versus the distribution of differences between the pre and post calibrated Visante OCT. The thin line in the figure represents the mean difference and the thick lines in the figure represent the 95% limits of agreement
The intent of the experiments was to explore whether there are differences among the optical devices that are used to perform pachymetry. There were differences and so the method proposed by42 Moezzi et al was used to remove the differences. The calibration equations that were derived enable the direct comparison among devices so that the commonly reported differences among pachymetric methods are now unimportant.49 The importance of having accurate (post-calibrated) corneal thicknesses when measured with any of these devices is that they are necessary for measurement of corneal hypoxia50,51 in CL wearers and in diabetics52 and for accurate IOP measurements,53 in cases of pre-surgical patients for refractive surgery,4 pre54 and post-surgical55 keratoconus patients and contact lens wearing patients for ortho-keratology.22
Most instruments which are being used to measure corneal thickness can be calibrated for the anterior surface with the use of a solid reference sphere or an asphere, but, the posterior surface cannot be calibrated with this device. The refractive index of the cornea is a variable common to all techniques for measuring corneal thickness by optical methods.56 Therefore, the ideal remedy, at least for the optical measurement techniques, would be calibrating the instruments using a transparent material with a similar refractive index as the human cornea in the form of a contact lens (that is with a visible posterior surface), as has been reported by Moezzi et al42 and in this study. Although previous studies show regional variation of corneal refractive index as well as variation of refractive index between different layers of the cornea,57 a refractive index of 1.376 is regarded as the overall corneal refractive index.58,59 Using reference lenses with refractive index of the cornea (1.376) allows rapid and simple calibration and cross calibration of these optical instruments for measuring central corneal thickness. This method demonstrates that in measuring lenses within the “average” corneal thickness range (from 375 to 550 microns) the instruments are quite accurate, but, with thicker or thinner reference lenses the error is increased. Thinner measures are over-estimated and thicker measurements are under-estimated with the VisanteTM OCT (Figure 10). Possibly the internal calibration of the Visante using its own solid calibration sphere is limited in the range of accuracy. These central thickness differences outside this average range can be clinically significant if decisions regarding refractive surgery are being made and regarding correction factors for the measurement of IOP, though it has been stated that a 20 micron difference may be considered clinically significant by others based on mathematical models.60,61 On the other hand, when decisions are made about eligibility for surgery using a thickness criterion, it is not at all clear that ±20 microns is used to define a range of uncertainty, it would be considered to be much less.62
Calibration requires that our ‘phantom corneas’ have two optical characteristics. The first is that the refractive index is as specified by the manufacturer and that this index is the “same” as the cornea. The second is that the refractive index is constant over the samples we used. Problems with the former (e.g. misspecification of refractive index) would result in the absolute measures of central corneal thickness obtained after calibration of each device being fractionally in error (the amount being a function of the misspecification). However, the calibration between devices would still be valid. Assuming that the cornea has a homogeneous refractive index is in itself an approximation since; it varies in depth and extra-axially.57,63 Therefore, in a sense, the phantom corneas with a single refractive index are only a first approximation. The second problem of heterogeneity of the refractive index across the sample lenses, provided it was non-systematic, would not be expected to affect the calibration equations significantly. Dunne et al examined the inaccuracy of the VisanteTM OCT using ray tracing of OCT images of contact lenses with a refractive index of 1.493 and centre thicknesses ranging from 0.3 to 0.7mm (in 0.1mm steps). Their results indicated that there was no variation in accuracy with thickness.60 Our approach was different to theirs, there were differences in measured/assumed refractive indices and also how the images were acquired differed. They used the anterior segment map (with custom software callipers) while we used the high resolution map (with the custom software).
A drawback of the study is perhaps that central thickness accuracy was examined and not peripheral. First, since this is a comparison of devices and there is no specific reason that one devices peripheral measurement is more or less accurate than another, we believe that the results can be generalized to the periphery.
Second, the range of the thickness of the rigid reference lenses included what might be expected for peripheral corneal thickness64 and so, again the results apply to peripheral measurements.
SummaryUsing reference lenses with refractive index of the cornea (1.376) allows rapid and simple calibration and cross calibration of instruments for measuring the central corneal thickness. The VisanteTM OCT and OCT II do not produce measurements equal to physical references with refractive index equal to the human cornea.
In clinical settings the possible inaccuracies in equipment may directly impact the treatment of the patient. We hope that the method that has been illustrated in this article will be useful in both research and clinical settings. Attention should be given when measuring corneas that are especially thinner or thicker than average as in cases of keratoconus and post-refractive surgery as well as post-penetrating keratoplasty, respectively, as these measurements may not be as accurate. The procedure used in the present study has not been applied to measurements from the VisanteTM OCT but does show that the measures can be calibrated and that multiple instruments can perform identically on lenses with the optical characteristics of the cornea.