To determine the prevalence of accommodative insufficiency (AI) and its relation with age, gender, and refractive errors in a college-age student population in Iran.
MethodsThe present study was conducted cross-sectionally in 2017. All students had optometric tests including measurement of visual acuity, objective and subjective refraction, as well as binocular vision and accommodative examinations. Amplitude of accommodation was measured with the Donders’ push-up method using the Royal Air Force (RAF) rule. Monocular accommodative facility was measured with ±2.00diopter flipper lenses. The accommodative response was tested using dynamic retinoscopy with the monocular estimation method (MEM).
ResultsThe prevalence of AI in the studied population was 4.07% (95% CI: 2.61–5.52). The rate was 6.04% (95% CI: 3.58–8.50) in females and 2.01% (95% CI: 0.53–3.48) in males, and logistic regression showed a significantly higher odds of AI in females (OR=3.14, 95% CI: 1.33–7.45, p-value=0.009). The prevalence of AI was 2.59% (95% CI: 0.55–7.56) in the 18–19-year-old age group and 4.08% (95% CI: 0.09–8.07) in the 24–25-year-old group (p-value=0.848). The prevalence of AI among emmetropic, myopic, and hyperopic individuals was 3.74% (95% CI: 1.88–5.61), 4.44% (95% CI: 2.07–6.81), and 5.26% (95% CI: 4.79–16.32), respectively (p-value=0.869). In the multiple regression model, only gender showed significant relationship with AI (Odds ratio=3.14, 95% CI: 1.33–7.45; p-values=0.009).
ConclusionThe prevalence of AI in the present study is lower than the most prevalence rates reported in previous studies. In the present study, gender and AI showed a strong association, such that AI prevalence was significantly higher in females than males.
Determinar la prevalencia de la insuficiencia acomodativa (IA) y su relación con la edad, sexo, y errores refractivos en una población universitaria de Irán.
MétodosEl presente estudio se realizó de forma transversal en 2017. Se realizaron pruebas optométricas a todos los estudiantes, incluyendo medición de la agudeza visual, refracción objetiva y subjetiva, visión binocular y pruebas de acomodación. La amplitud de acomodación se midió con el método de Donders (push-up) utilizando la regla de la RAF (Royal Air Force). La flexibilidad acomodativa monocular se midió con flippers de ±2 dioptrías. La respuesta acomodativa se evaluó mediante retinoscopía dinámica utilizando el método de estimación monocular (MEM).
ResultadosLa prevalencia de IA en la población de estudiantes fue de 4,07% (95%ICI: 2,61–5,52). La tasa fue de 6,04% (95%IC: 3,58–8,5) en mujeres y 2,01% (95%IC: 0,53–3,48) en varones, y la regresión logística reflejó un odds ratio significativamente superior de IA en mujeres (OR=3,14, 95%IC: 1,33–7,45, valor p=0,009). La prevalencia de IA fue de 2,59% (95%IC: 0,55–7,56) en el grupo de edad de 18–19 años, y de 4,08% (95%IC: 0,09–8,07) en el grupo de 24–25 años (valor p=0,848). La prevalencia de IA entre los individuos emetrópicos, miopes e hipermétropes fue de 3,74% (95%IC: 1,88–5,61), 4,44% (95%IC: 2,07–6,81), y 5,26% (95%IC: 4,79–16,32), respectivamente (valor p=0,869). En el modelo de regresión múltiple, únicamente el sexo reflejó una relación con IA (Odds ratio=3,14 95%IC: 1,33–7,45; valor p=0,009).
ConclusiónLa prevalencia de IA en el presente estudio es inferior a la mayoría de las tasas de prevalencia reportadas en estudios previos. En el presente estudio, sexo e IA reflejaron una fuerte asociación, en el sentido de que la prevalencia de IA fue significativamente superior en las mujeres con respecto a los varones.
According to the definition by the American Optometric Association, accommodative insufficiency (AI) is a type of accommodative dysfunction in which the amplitude of accommodation (AA) is lower than the age-expected norm for an individual and is not due to sclerosis of the crystalline lens.1 AI is in fact a sensory motor anomaly of the visual system, and the main feature is the inability to focus or sustain focus at near.2 AI leads to various vision-related symptoms in affected individuals, including blurred vision, diplopia, eyestrain, headaches, difficulty in adjusting the focus from one distance to another, inability to concentrate, and loss of comprehension over time.3,4 All these symptoms occur during near work and significantly affect an individual's performance during near visual activities.5 Also, these symptoms can prevent a person from engaging in near work such as reading.6 Hence, AI can interfere with learning and impair academic and educational performance, which is especially important for school-age children and students.7,8 According to Borsting et al., individuals with symptomatic accommodative disorders have a higher frequency of behaviors related to school performance and attention.9 Accommodative disorders, including AI, can also impair occupational performance, especially in occupations that involve considerable amounts of close work (such as extensive computer users) or reading.1,10 It should be noted that accommodative dysfunction is one of the most important factors in the occurrence of computer vision syndrome (CVS), which has recently received great attention in light of the increased use of computers and electronic devices.11 Other impacts of AI include the effect on sport performance.1 Based on the results of previous studies, athletes have better accommodative and binocular function than non-athletes, and accommodative and binocular disorders can interfere with successful sporting performance.12,13 In light of the above, it can be concluded that AI can reduce patients’ quality of life, therefore, the diagnosis and effective treatment of this accommodative dysfunction is one of the most important issues in the optometric practice.14
Availability of epidemiological information about a condition has clinical implications for generating a hypothesis regarding the possible diagnosis, and subsequently, deciding about the process to follow.15,16 Epidemiological information is also important for planning screening programs to identify cases, research projects, and adopting political strategies for vision health.16 Despite the importance of AI, there is no accurate epidemiological information on its prevalence in the general population. Although many clinicians believe that accommodative disorders such as AI are commonly seen in clinical practice, there are few scientific studies in this area.3 Most existing studies are of clinical nature, in which a non-randomized population has been selected, and thus, their results are not applicable to the general population.16 Knowledge of the accurate prevalence in a population requires population-based studies using proper sampling and randomization.17 According to a systematic review published by Cacho-Martinez in 2010, there is not enough scientific information on the true prevalence of accommodative disorders, including AI, in the general population, and the need for population-based studies is strongly felt in this regard.16,18 On the other hand, most existing studies focus on pediatric populations, with very little information about college-age students and young adults,18 while this age group is of particular importance due to their high volume of near work. Significant differences in the prevalence rates reported in previous studies is another problem and limitations of the literature in this field, and the highest degree of disparity is seen with AI,16,18 such that its reported prevalence rates range from 0.2 to 61.7%.18–26 With the above background in mind, the purpose of the present population-based study is to determine AI prevalence among college-age students in Iran. In addition, the association between this disorder and certain parameters such as age, gender, and refractive errors are investigated to improve our understanding of the nature of this disorder.
Material and methodsThis cross-sectional study was conducted in 2017. In this study, the target population was students of Shahrekord University, one of the central cities in Iran. Students were selected through multi-stage cluster sampling. Each academic major was considered as a stratum. From each major, in proportion to the total number of students, samples were selected randomly from the student rosters. Selected students were then invited to participate in the study, and informed consents were obtained. First a series of demographic information was collected from each interviewed student. Optometric tests were then performed for each student.
Optometric examinationsAll optometric examinations were performed under normal illumination conditions at the mesopic level by a single examiner. Overhead lighting was also provided with a stand lamp on the target for accommodative and binocular vision tests.
First, uncorrected distance visual acuity (UCVA) was measured using the Snellen E-chart at a distance of 6m Then objective refraction was done using an auto-refractometer (Topcon RM8800 auto-refractometer, Topcon Corporation, Japan), and the results were refined through retinoscopy (Heine Beta 200, Heine Optotechnik, Germany). In the next step, subjective refraction was done to determine the best optical correction, and the best corrected visual acuity (BCVA) was recorded.
The next stage included binocular and accommodative examinations with the best optical correction in place. First, unilateral and alternating cover tests were carried out at far (6m) and near (40cm), respectively, and the magnitude of far and near heterophoria was measured using the prism bar. The target used for the cover test was one line above the far and near BCVA (in the eye with worse BCVA), on the far and near Snellen chart, respectively.
Next, the amplitude of accommodation (AA) was measured using the Donders’ Push-Up method with the Royal Air Force (RAF) rule separately for each eye starting with the right eye and then the left eye. For this test, the examinee was properly positioned in front of the instrument, and the instrument's target, which contained a row of letters equivalent to a visual acuity of 20/30, was slowly brought closer in the midline. The individual was asked to keep letters clear as far as possible and report as soon as the letters became blurred and the examinee was no longer able to achieve clear vision (first sustained blur). At this time, the near point of accommodation (NPA) was recorded in centimeters (cm) from the dial on the device. To improve testing reliability, NPA measurement was repeated three times, and the average of the three measurements was recorded as the final NPA, which was then converted to the AA in diopters (D) by dividing it into 100.
In the next step, monocular accommodative facility (MAF) was measured starting with the right eye and then the left eye using ±2.00 diopter flipper lenses. To perform this test, a Snellen near chart was placed at a distance of 40cm from the examinee who was then asked to look at the row that was equivalent to his/her corrected visual acuity. It was explained to the participants that plus and minus lenses would be placed alternately in front of their eyes, and that they should say “clear” whenever the chart's letters were clearly identifiable through each lens. Each instance of clearing both plus and minus lenses, was counted as one cycle, and the number of cycles per 1min (cpm) was recorded as the MAF.
Next, the accommodative response (AR) was tested using dynamic retinoscopy with the monocular estimation method (MEM). For this purpose, the examiner was positioned at the distance of 40cm from the examinee, and she/he was asked to read out the chart attached to the retinoscope's head, which included small print letters (equivalent to 20/30 visual acuity). In this fashion, binocular dynamic retinoscopy was performed, and the AR (lag or lead of accommodation) was measured by placing plus or minus lenses in front of the person's eye to neutralize with or against movement of the retinoscopic reflex, starting with the right eye and then the left eye. Finally, ocular health status was evaluated through slit lamp examination, and the posterior segment was examined with a +90D lens.
Exclusion criteria included strabismus, amblyopia, BCVA less than 20/30 in either eye, history of eye trauma, history of intraocular surgery, any pathologic or systemic disease affecting accommodation or binocular vision, and use of any ocular or systemic drugs affecting accommodation or binocular vision.
DefinitionsMyopia and hyperopia were defined as a subjective spherical equivalent refraction less than −0.50D and greater than +0.50D, respectively. Near exophoria and esophoria were defined as more than six prism diopters (PD) exophoria and any esophoria at a near distance of 40cm, respectively.3 In order to define AI, the following three criteria were used in accordance with the guidelines suggested by Scheiman and Wick.3 A definite diagnosis of AI required meeting the first criterion plus either of the other two criteria.
- 1.
Reduced AA by 2diopters (or more) compared to the expected average based on the Hofstetter's formula; 18.5D−[0.3D×(age in years)].
- 2.
MAF less than 6cpm, such that the individual has difficulty focusing with the minus lens.
- 3.
Accommodative lag more than +0.75D in MEM retinoscopy.
The Ethics Committee of Mashhad University of Medical Sciences approved the study protocol, which was conducted in accordance with the tenets of the Helsinki Declaration. All participants signed a written informed consent.
ResultsOf the 854 selected students, 726 participated in this study, and after applying the exclusion criteria, analyses were performed with data from 713 people. The mean age of these students was 21.35±1.87 years (from 18 to 25 years) and 364 of them (51.1%) were female. The mean of spherical equivalent in myopic and hyperopic individuals were −1.83±1.67 (−0.63 to −14.55) and 1.01±0.65 (0.63 to 2.63), respectively.
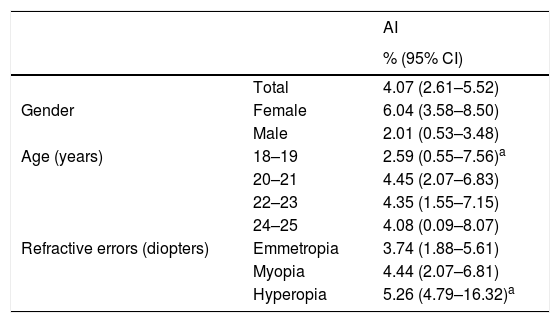
The prevalence of AI has been shown in Table 1. The overall prevalence of AI in this study was 4.07% (95% CI: 2.61–5.52); 6.04% (95% CI: 3.58–8.50) in females and 2.01% (95% CI: 0.53–3.48) in males. Logistic regression analysis showed significantly higher odds of AI in females (OR=3.14, 95% CI: 1.33–7.45, p-value=0.009). As demonstrated in Table 1, the prevalence of AI showed no linear trend with age. Overall, chi-square test showed no significant relationship between age and the prevalence of AI (p-value=0.848). Table 1 also shows the prevalence of AI in different groups of refractive status; there was no significant difference in AI prevalence among these three groups (p-value=0.869).
The prevalence of accommodative insufficiency (AI) by age, gender and refractive errors.
| AI | ||
|---|---|---|
| % (95% CI) | ||
| Total | 4.07 (2.61–5.52) | |
| Gender | Female | 6.04 (3.58–8.50) |
| Male | 2.01 (0.53–3.48) | |
| Age (years) | 18–19 | 2.59 (0.55–7.56)a |
| 20–21 | 4.45 (2.07–6.83) | |
| 22–23 | 4.35 (1.55–7.15) | |
| 24–25 | 4.08 (0.09–8.07) | |
| Refractive errors (diopters) | Emmetropia | 3.74 (1.88–5.61) |
| Myopia | 4.44 (2.07–6.81) | |
| Hyperopia | 5.26 (4.79–16.32)a |
CI: confidence interval.
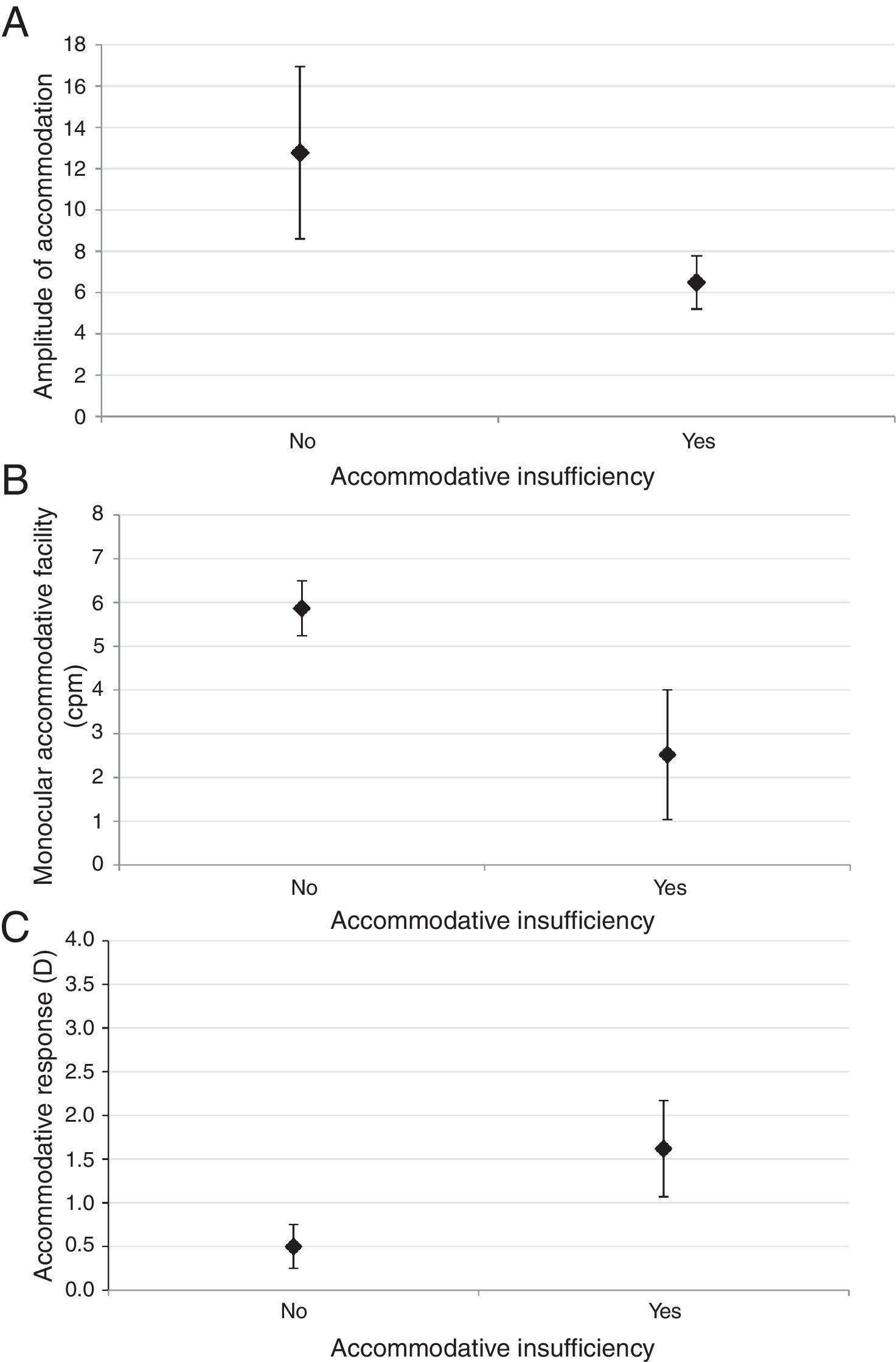
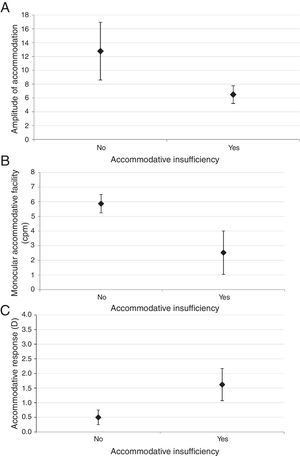
Fig. 1 shows the distribution of AA, MAF and AR in participants with and without AI. As seen in Fig. 1, all of these parameters showed statistically significant differences between two groups (all p-values<0.001). In the multiple regression model, only gender showed significant relationship with AI (Odds ratio=3.14, 95% CI: 1.33–7.45; p-values=0.009).
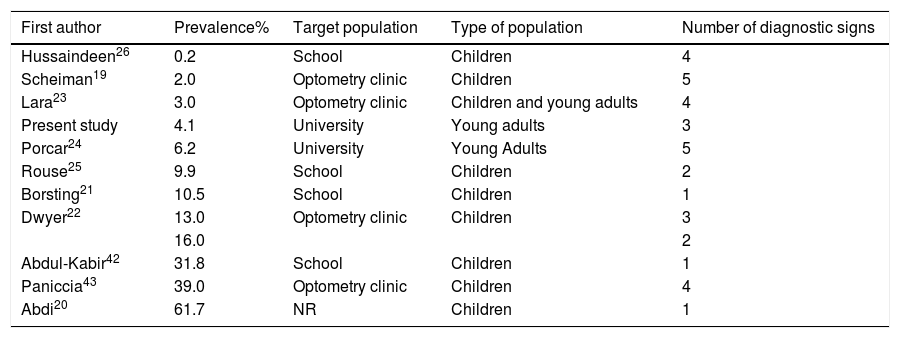
DiscussionIn the present study, we examined AI prevalence and its association with certain factors in Iranian students aged 18–25 years. The present study is one of the few population-based studies on AI prevalence in young adults, and the only study conducted on the prevalence of this accommodative disorder in an Iranian population. Based on the results of the present study, the overall prevalence of AI was 4.07%. Table 2 shows the prevalence of AI reported in previous studies, which ranges widely from 0.2% to 61.7%. The large differences among studies can be examined from several aspects. Firstly, differences in the target populations in these studies. As presented in Table 2, most previous studies have been conducted on children, and only two studies looked at AI prevalence in adults. As the data in this table indicate, most studies conducted on children have reported a higher prevalence of AI compared to adult studies. In justifying this finding, it should be noted that AI diagnosis is mainly based on the interpretation of subjective clinical tests, including AA, accommodative facility, and relative accommodation. The endpoint of all these subjective accommodative tests is the report of sustained blur by the examinee.27 It can be assumed that children differ from adults in their ability to discern and report sustained blur, and their delayed response can be interpreted as accommodative dysfunction, and thus, a higher AI prevalence in children. This issue influences the comparability of studies in children and adults.
The reported prevalence of accommodative insufficiency (AI) in the literature.
| First author | Prevalence% | Target population | Type of population | Number of diagnostic signs |
|---|---|---|---|---|
| Hussaindeen26 | 0.2 | School | Children | 4 |
| Scheiman19 | 2.0 | Optometry clinic | Children | 5 |
| Lara23 | 3.0 | Optometry clinic | Children and young adults | 4 |
| Present study | 4.1 | University | Young adults | 3 |
| Porcar24 | 6.2 | University | Young Adults | 5 |
| Rouse25 | 9.9 | School | Children | 2 |
| Borsting21 | 10.5 | School | Children | 1 |
| Dwyer22 | 13.0 | Optometry clinic | Children | 3 |
| 16.0 | 2 | |||
| Abdul-Kabir42 | 31.8 | School | Children | 1 |
| Paniccia43 | 39.0 | Optometry clinic | Children | 4 |
| Abdi20 | 61.7 | NR | Children | 1 |
NR: not reported.
Secondly, the inter-study differences can lie in different diagnostic criteria used in these studies. As presented in Table 2, different studies have used different diagnostic criteria for the definition and diagnosis of AI. As such, some used only one criterion (reduced AA) and some have applied more criteria (up to 5 diagnostic criteria). Looking closely at Table 2, it appears that studies with more diagnostic criteria for AI have mostly reported a lower prevalence of this disorder. On the other hand, in studies that only rely on reduced AA, AI prevalence rates are significantly higher. It should be noted that in previous studies, Hofstetter's formulas were used to interpret whether the AA was normal or not. Hofstetter's formulas assume a linear relationship between AA and age,28 so the expected mean and minimum for each age can be estimated using 18.50−0.3×age and 15−0.25×age formulas, respectively.29,30 If the AA is 2diopters (or more) lower than the expected mean or minimum AA based on Hofstetter's equations, it is considered as a diagnostic criterion for AI.31 In recent years, a number of studies have examined the efficacy of Hofstetter's formulas for estimating the true AA. These include studies by Hashemi et al.,29 Ovenseri-Ogbomo et al.,32 and Sterner et al.31 According to the findings of these studies, there are significant differences between the true AA and the estimated values calculated from Hofstetter's formulas in children; they suggest that Hofstetter's formulas overestimate the AA and may lead to erroneous clinical interpretation and a false positive diagnosis of AI. According to the above discussion, the high prevalence reported in studies with reduced AA as the only diagnostic criterion (which are also performed on children) is justifiable. Therefore, the prevalence rates reported in these studies do not seem true and are believed to be mainly due to error in the diagnostic criterion. This issue is further confirmed in another study by Hashemi et al.33
Another aspect of existing inter-study differences is the designs and sampling methods of these studies. Accurate estimation of the prevalence of a disorder in epidemiologic studies requires a considerably large sample size with a proper sampling method (multistage cluster sampling) and randomization to allow for generalizability of the estimated prevalence. A look at previous studies summarized in Table 2 shows that this is not true in case of AI. Some previous studies focus on specific clinical populations, and their results cannot be generalized to the total population, given that mostly people with disorders present to clinics, these samples are biased. In non-clinical studies, which are mostly done at schools or universities, randomization has not been applied, and while it seems that these studies have a more accurate prevalence compared to clinical studies, the problem of non-generalizability is one of their serious limitations, because their setting has mostly been a single school or college, and as a result, the findings will not be generalizable to the entire population of school children or students.
In this study, we also examined the association between AI and certain factors such as age, gender, and refractive errors in order to get a better understanding of the nature of this disorder and its identification. According to the findings of this study, there was a significant relationship between AI and gender, such that the prevalence of AI in women was three times higher than that in men (6% versus 2%), and this significant relationship was confirmed in the regression model in the presence of other factors. In our review of the literature, we only found one study that examined the gender distribution of AI. The study, conducted by Marran et al.,4 similar to our study found that AI prevalence was significantly higher in females than in males, but there was no discussion about possible reasons. It should be noted that literature has little and contradictory information on the association between accommodative performance and gender. In the study by Ogbomo et al.32 who measured AA among Ghanaian children, the AA was significantly lower in girls than boys, and this observation was attributed to the higher number of boys in the sample. In another similar study by Hashemi et al.,29 the mean AA, after controlling for age, was higher in girls than boys. In this study, there was no clear explanation for these findings, and it was argued that this finding may be due to the effect of confounding factors. In the study by Pandian et al.,34 there was no significant difference in accommodative facility between boys and girls. Yekta et al.35 reported a higher positive relative accommodation (PRA) in women than men, and this was attributed to the possibility of more active accommodation in women. In a meta-analysis by Hickenbotham et al.36 on the relation of gender to accommodative performance and the onset of presbyopia, the authors concluded there is no physiological differences between men and women concerning accommodation, and the younger onset of presbyopia in women is due to other differences such as type of near work and the reading distance. In a study by Horwood,37 concerning the early development of the accommodative and vergence systems, which was conducted on full-term 1–6 month old infants, the authors pointed to physiological differences between genders. According to the results of their study, the accommodative system develops better and faster in boys during this age range. Based on the above, there is no clear evidence of a relationship between accommodative function (and thus, the prevalence of accommodative dysfunction) and gender. Although the presence of this relationship can be discussed based on assumptions such as inter-gender physiological differences in accommodation mechanism and hormonal differences, currently there is not enough evidence to confirm or reject it. On the other hand, the observation in this study regarding significant inter-gender differences in the prevalence of AI can have important clinical implications. It is recommended that this issue be studied in future epidemiological studies in other racial populations.
In the present study, we also examined the association between age and AI prevalence. As seen in Table 1, the lowest prevalence of AI (2.59%) was observed in the 18–19-year age range, and the highest prevalence (4.45%) was in 20–21-year-olds. Except for 18–19-year-olds who had a relatively low AI prevalence, the rates were approximately similar in other age groups. Overall, the results of this study did not show a significant relationship between AI prevalence and age. It should also be noted that there is no evidence of a relationship between AI and age in the literature either. Theoretically, given the age-related reduction in the elasticity of lens fibers as well as the lens capsule and the increased lens size (which is associated with reduced AA),38 we expected AI prevalence to increase with age, nonetheless, our findings do not support this theory. It should be noted, however, that the age range of the participants in the present study was limited and therefore, any interpretation about the association between age and AI should be done with caution.
In this study, we also investigated the association between refractive errors and AI. According to the results, the emmetropic group showed the lowest AI prevalence at 3.74%, and the hyperopic group had the highest prevalence at 5.26%; however, this relationship was not statistically significant. It should be noted that some studies have reported lower AA in hyperopic compared to myopic and emmetropic individuals,33,39,40 which is in agreement with the results of the present study suggesting a higher AI prevalence in hyperopes. Regarding the reason for lower AA in hyperopic individuals, the theory proposed by McBrien and Millodot40 can be mentioned. Based on this theory, the association between refractive errors and AA can be explained on the basis of differences in autonomic nerve control of accommodation in cases with different refractive errors. Hyperopes have a strong sympathetic innervation or weak parasympathetic innervation to the ciliary muscle, and thus, they have lower AA compared to myopic and emmetropic cases.40 This theory was also confirmed by Charman.41 Based on our findings, another point to take in consideration in interpreting the relationship between refractive errors and AI prevalence is latent hyperopia. It should be noted that since cycloplegic refraction was not performed, we were not able to control for the effect of this factor. It is possible that latent hyperopia has a role in the higher AI prevalence in hyperopic cases of the present study. The relationship between refractive errors and AI is clinically important and further studies in this field are needed to confirm or reject the findings of this study.
ConclusionIn this population-based study, we examined the prevalence of AI in college-age students in Iran for the first time. The prevalence of AI in this study was 4.07%, which is lower than the most prevalence rates reported in previous studies. Gender had a significant relation with AI, such that the prevalence was significantly higher in females than males. No significant association was found between AI and age or refractive errors.
FundingThis project was supported by Mashhad University of Medical Sciences (grant code:950486).
Conflicts of interestThe authors report no conflicts of interest. The authors alone are responsible for the content and writing of the paper.