Uveal coloboma results from incomplete closure of the optic cup fissure. While conducting an evaluation of a new ultra-wide field retinal imaging camera (Optomap), which provides a view of the fundus up to 200° at one time without mydriasis, we discovered a case of bilateral chorioretinal coloboma in a 21-year-old student. The lesion was located in the midperiphery of each eye less than 2disc diameters (DD) below the optic disc in the inferonasal quadrants. The size of the coloboma in the right eye was 1.8DD in height and 1.3DD in width, while the left lesion was 2.4DD in height and 2.6DD in width. The subject was totally asymptomatic and without any complication such as retinal detachment or choroidal neovascularization, which often accompany this type of lesion. The visual field of each eye displayed an absolute scotoma corresponding to the size and location of the coloboma. No management was necessary but the subject was advised to report for visual examination at regular intervals because complications can occur at any age.
El coloboma uveal tiene su origen en el cierre incompleto de la fisura de la copa óptica. Al realizar la evaluación de la funcionalidad de una nueva cámara de imagen retiniana de campo ultra-amplio (Optomap), que proporciona una visión del mismo de hasta 200° de una sola vez y sin midriasis, descubrimos un caso de coloboma coriorretiniano en un estudiante de 21 años de edad. La lesión se situaba en la media periferia de cada ojo, a menos de dos diámetros de disco por debajo del disco óptico, en los cuadrantes inferonasales. El tamaño del coloboma en el ojo derecho era de 1,8 diámetros de disco (DD) de altura, y 1,3DD de anchura, mientras que la lesión en el ojo izquierdo era de 2,4DD de altura y 2,6DD de anchura. El paciente era totalmente asintomático y sin complicación alguna tales como desprendimiento de retina o neovascularización coroidea, las cuales acompañan a menudo a este tipo de lesión. El campo visual de cada ojo reflejaba un escotoma absoluto que correspondía al tamaño y localización del coloboma. No fue necesario ningún tratamiento, aunque se informó al paciente de que debía someterse a exámenes visuales regulares, puesto que las complicaciones pueden manifestarse a cualquier edad.
Ocular coloboma results from incomplete closure of the embryonic fissure of the neuroectodermal optic cup around weeks 5–8 of gestation.1 Closure starts at the equator and continues anteriorly and posteriorly. Any insult during this time could create defects of varying size and location. A coloboma may extend from the iris margin to the optic disc and involve one or more defects along the fusional lines.
A coloboma affecting the posterior segment of the eye can be unilateral or bilateral. It is bilateral in about 60% of cases.2 If the fetal fissure fails to close posteriorly, then a coloboma affecting the retinal pigment epithelium (RPE), neurosensory retina, or choroid may occur. The defect is essentially a bare sclera with the overlying RPE, retina, or choroid missing. In some cases, although the retina is present, it is hypoplastic and gliotic.3 Typically occurring in the inferonasal quadrant, it may extend to include the optic nerve. Usually, a chorioretinal coloboma is asymptomatic, despite significant upper visual field defects.
Chorioretinal coloboma have numerous associated systemic conditions involving the cardiovascular, central nervous, musculoskeletal, gastrointestinal, genitourinary and nasopharyngeal systems.4
The data on the prevalence and incidence of ocular coloboma is sparse. The incidence depends upon the population studied, ranging from (number of cases per 10,000 births) 0.5 in Spain,5 1.4 in France,6,7 2.6 in the USA8 to 7.5 in China.9 Colobomas have been reported in 0.6–1.9% of blind adults in Canada10 and 3.2–11.2% of blind children worldwide.11 However, under-ascertainment of posterior segment coloboma is most probable.9 It is likely that the chorioretinal colobomas would not have been detected in some of the aforementioned studies if they had not affected vision. In fact, only one study explicitly examined chorioretinal coloboma at birth5 and found an incidence of 0.2 per 10,000.
While conducting an assessment of the ocular fundus of several hundred young people with a new ultra-wide field retinal imaging device we incidentally discovered one case with bilateral chorioretinal coloboma, which we describe in this report.
Case reportThe Department of Optometry at Hadassah Academic College in Jerusalem offers vision screening to all incoming first year students during orientation week. The students are encouraged to identify visual problems that might interfere with their studies and the compliance rate is approximately 50%.
A 21-year-old first year female student presented to our clinic for vision screening. The patient was entirely asymptomatic and had completed high school registration. She did not present with any condition for which she needed to take medication on a regular basis.
A visual screening examination revealed an uncorrected visual acuity of 6/6 OD and 6/5 OS using the Snellen visual acuity chart. Her stereopsis was shown to be normal by 30s of arcs. Autorefraction with the L80 wave+(Visionix Luneau, Chartres, France) revealed sphere/cylinder X axis of −0.50/−0.45×34 and −0.40/−0.20×175 for OD and OS, respectively. Auto-keratometry and aberrometry results were unremarkable. Ocular motility was full.
Ultra-wide field retinal imaging with the Panoramic200 Scanning Laser Ophthalmoscope (Optos plc, Dunfermline, UK) is part of our regular screening examination. This instrument uses a patented ellipsoidal mirror to capture ultra-wide-field, high resolution digital retinal images (2000×2000 pixels) without the need for pupil dilation, corneal contact or high levels of illumination. The image produced is named the Optomap Retinal Exam and can be viewed and manipulated in red and green wavelengths, allowing different layers of the retina to be viewed.12 The green laser (532mm) images mainly the sensory retina and pigment epithelium, while the red laser (633mm) images mainly deeper structures of the retina, from the pigment epithelium to the choroid. The advantage of this system is that it allows the retina to be scanned over a large portion of the ocular fundus with a field of up to 200° without pupil dilation, as opposed to the view with a standard fundus camera of only 45° and that of an SLO of 20–60°.13–15 The exam involves asking the patient to focus on a target in the instrument and takes less than one minute for each eye to position the patient and capture the image.
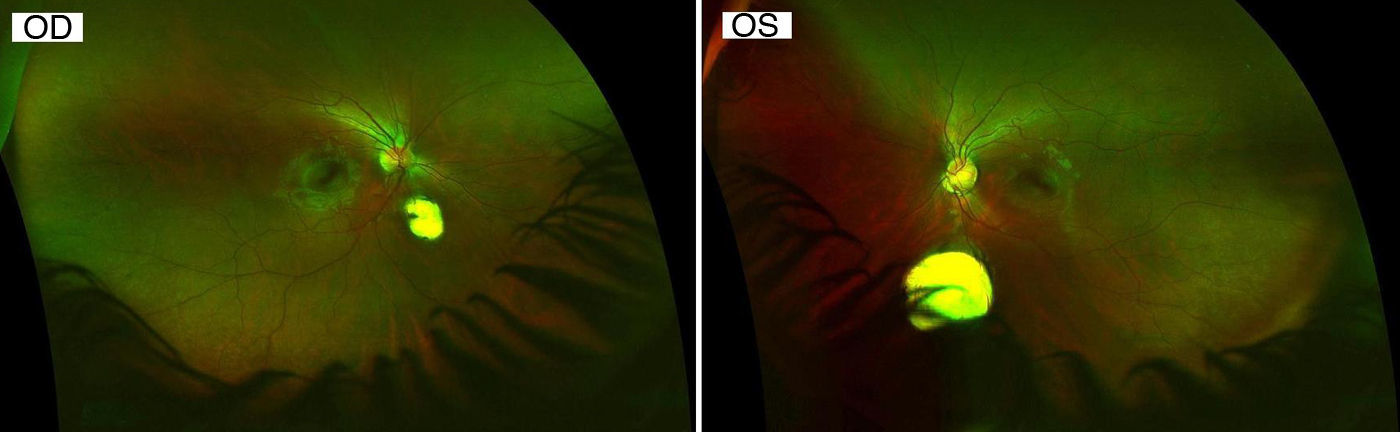
The Optomap Retinal Exam images revealed an oval shaped lesion in each retina in the inferonasal quadrant (Fig. 1, right and left). The lesions were measured in pixels using the Optos review software and converted to disc diameter (DD) based on the pixel measurement of the optic disc. The lesion on the right retina was 1.1DD inferior to the disk with a height and width of 1.8 and 1.3DD, respectively. The lesion on the left retina was larger (2.4×2.6DD) and 1.7DD inferior to the disc. The patient was referred to our clinic for a full ocular examination.
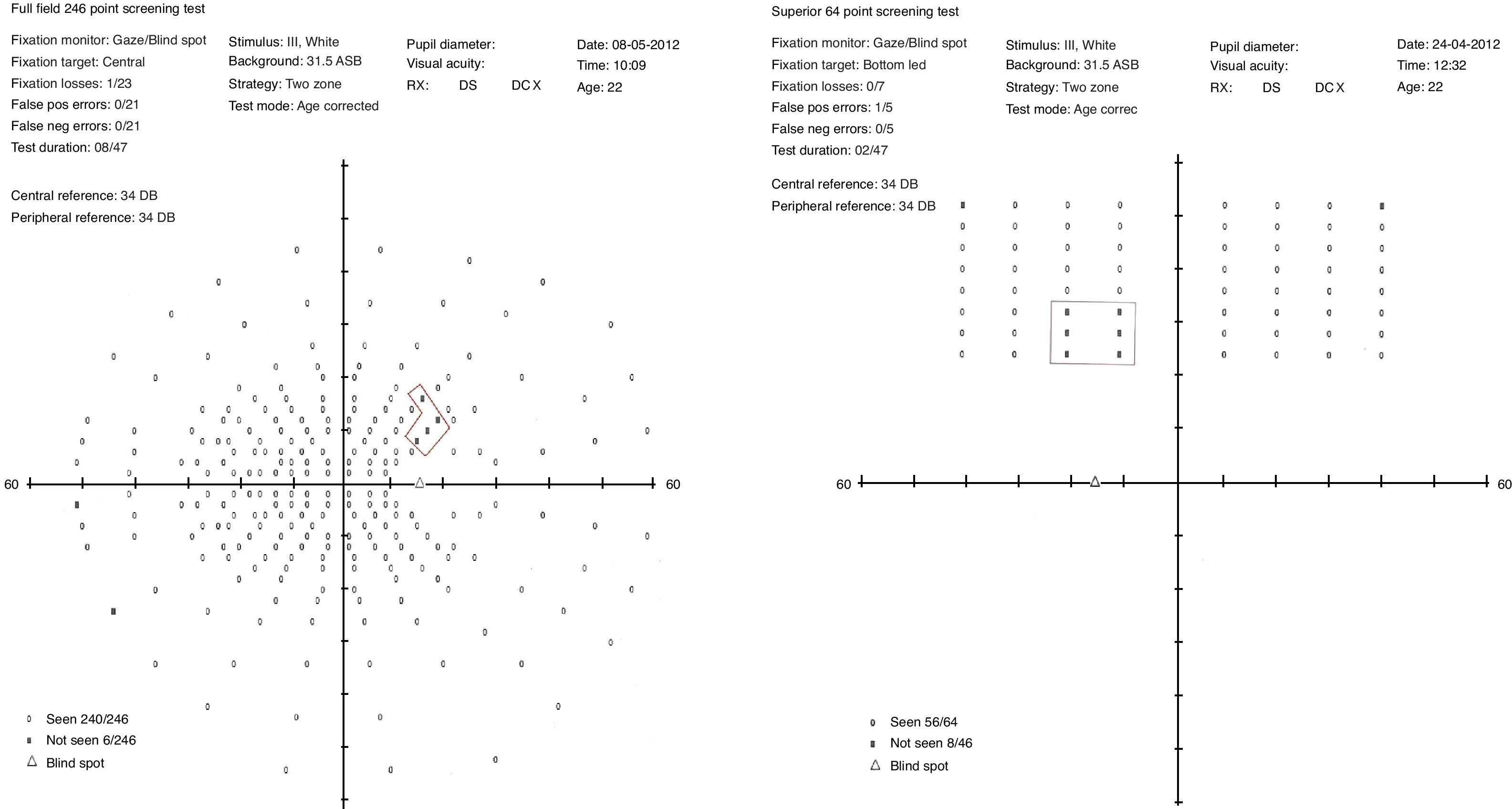
Fundus examination by slit-lamp biomicroscopy did not reveal any other pathology. An absolute scotoma corresponding to the size and location of the lesion was apparent in the visual fields of each eye using a supra-threshold strategy on the Humphrey Visual Field Analyzer (Fig. 2A and B). Since the size of each lesion was small, screening field programs that would maximize the number of test points in the suspected areas were used.
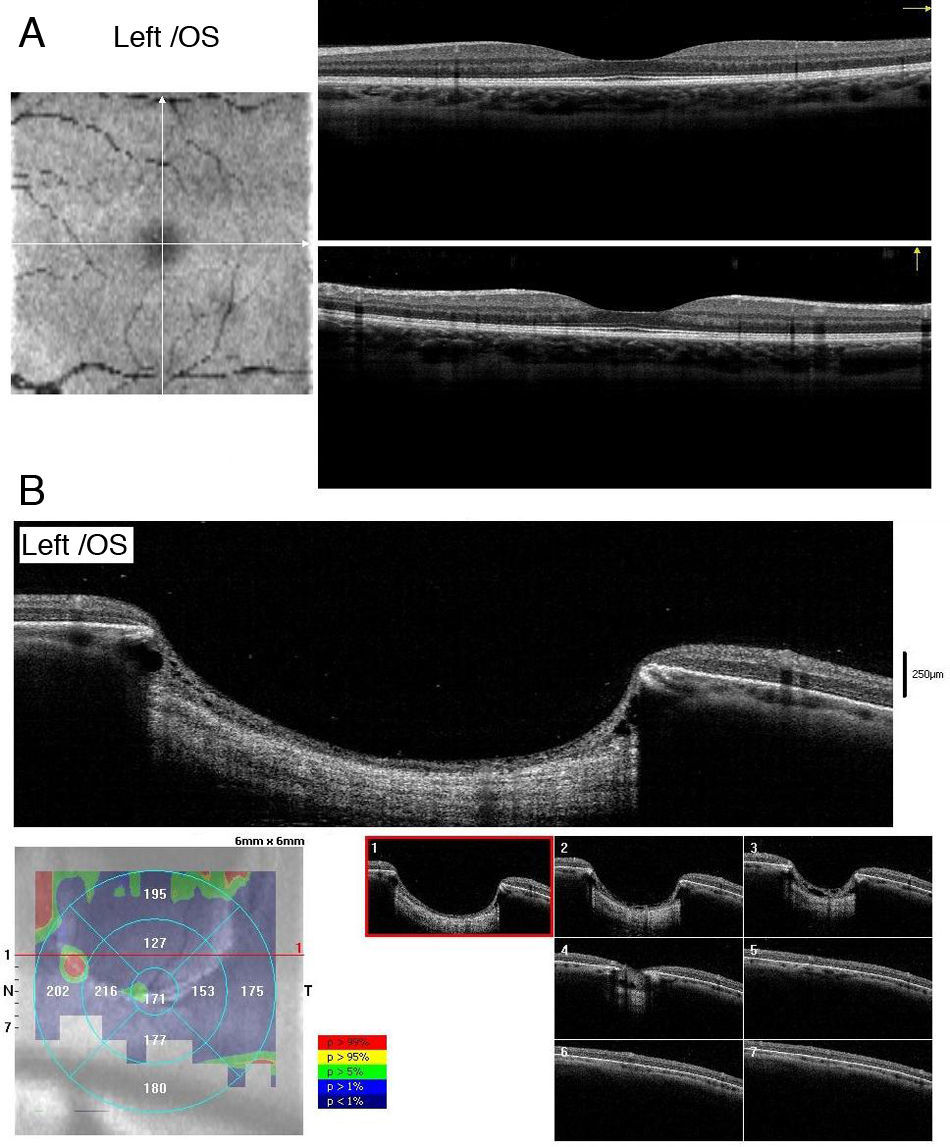
An OCT scan (Optovue Inc., Fremont, CA, USA) of her left eye (Fig. 3A) showed a normal fovea. The OCT image of the lesion in that eye (Fig. 3B) showed an associated atrophic neurosensory retina, with an absence of the retinal pigment epithelium, following the contour of a crater-like depression created by the absence of the underlying choroid. This appearance is consistent with an inferonasal chorioretinal coloboma and with the visual field defect.
DiscussionIt is possible that this case of chorioretinal colobama could have been detected during a thorough ophthalmoscopic examination of the fundus. However, this is not very likely at present as this subject is young and asymptomatic. In addition, in Israel not all optometrists examine the ocular fundi, and patients only visit ophthalmologists if they are symptomatic. The casual discovery of this malformation was enabled by the use of the Optomap, a wide-field retinal imaging device which provides a view of the central and mid peripheral retina of up to 200 degrees at one time without mydriasis.
The incidental finding of a bilateral chorioretinal coloboma in a healthy asymptomatic subject raises the notion that this malformation may be more prevalent than once thought. To give a better estimate of the prevalence of chorioretinal coloboma, a large epidemiology study needs to be carried out using similar methodology.
Chorioretinal colobomas are congenital.16 They can be sporadic with no other affected family member or inherited. Bilateral chorioretinal coloboma is usually inherited in an autosomal dominant fashion with variable penetrance,17 but some cases of recessive inheritance have been reported,18 especially if the individual is the offspring of a consanguineous marriage as noted in a southern Indian population.19 We do not have any evidence regarding this issue in the present case as we would have needed to test the parents in order to determine if it was inherited and the type of inheritance. There is evidence of mutation in the PAX6 gene in 1-year-old boy who had a large coloboma of the optic nerve, retina and choroid.20 In a patient with chorioretinal coloboma, Asai-Coakwell et al.21 identified a chromosome 8q21.2–q22.1 segmental deletion.
Chorioretinal colobomas are in many instances asymptomatic as is the present case in which the coloboma, although relatively large, is located in the mid-periphery away from either the macula or the disc. However complications are not uncommon and they often cause diminished visual acuity or distorted vision, especially when extending to the macula or optic disc.16 The most common complications are retinal detachment, which occur in 8.1–43% of cases16,22–27 and for which surgical treatment has variable success,27,28 and choroidal neovascularization.16,26,29–31 This latter complication often involves the optic nerve head.32–36 The risk of a complication can develop at any age throughout life. Of the few cases of chorioretinal colobomas in which choroidal neovascularization occurred that have been reported in the literature, two were aged 1 year old,32,35 four were in their 20s16,26,31,36 and two were aged 65 and 70 years old, respectively.29 Although our 21-year-old subject is at present totally asymptomatic we have advised her to attend for a visual examination at regular intervals or if she notices blurred or distorted vision.
Summing up, using the Optomap, we discovered a case of bilateral chorioretinal coloboma in a patient without any symptom. This raises the importance of visual screening using a wide-field retinal imaging device.
We would like to thank Optos plc for loaning the Panoramic200 Scanning Laser Ophthalmoscope to the clinic at our Department. Dr. Simon Barnard has a consulting contract with Optos plc. Dr. Shneor was supported by a grant from the Israel Society for Psychobiology. We would like to thank Ms. Dinah Paritsky for critical reading of the manuscript.