To assess real-world adoption of presbyopic correction and its impact on quality of vision.
MethodThe use of visual corrections by 529 sequential patients (aged 36 years to 85 years, 50.4% female) attending 4 optometric practices in diverse areas across London were surveyed by interview and completed the quality of vision (QoV) questionnaire to evaluate visual symptoms.
ResultsOver half of the population (54.7%) managed without glasses at least some of the time, while between 30 and 40% wore distance, reading and progressive spectacles with those using Progressive Addition Lenses wearing them over 80% of the time, while those wearing reading spectacles only approximately 25% of the time. Age, sex and driving frequency had no effect of QoV (p>0.05), whereas the distance of the task significantly impacted QoV (p<0.01). In all QoV metrics, regardless of the far, intermediate or near blur assessment, QoV was rated higher by patients whose main tasks were far focused (n=231, 43.9%), than those who principally conduct intermediate tasks (n=165, 31.4%) and worse still for those whose main tasks were near (n=130, 24.7%), regardless of the form of correction.
ConclusionMajority of tasks are in the distance and these had a higher QoV than intermediate tasks with near focused tasks being even worse. It is important to discuss with patients the principal distance of the tasks they generally perform and the forms of presbyopic correction used from the outset.
Evaluar la adopción en el mundo real de la corrección de la presbicia y su impacto sobre la calidad de visión.
MétodoSe supervisó el uso de correcciones de la visión por parte de 529 pacientes secuenciales (edad de 36 a 85 años, 50,4% mujeres) que acudieron a cuatro consultas optométricas en diferentes zonas de Londres, mediante entrevistas y cuestionarios sobre calidad de visión (QoV), para evaluar los síntomas visuales.
ResultadosMás de la mitad de la población (54,7%) se manejaba sin gafa, al menos parte del tiempo, mientras que entre el 30 y el 40% utilizaban gafa de distancia, lectura y progresiva, y aquellos que utilizaban lentillas progresivas las utilizaban más del 80% del tiempo, mientras que los que utilizaban gafa de lectura la utilizaban alrededor del 25% del tiempo. La edad, el sexo y la frecuencia de conducción no tuvieron efecto sobre la QoV (p>0,05), mientras que la distancia de la tarea tuvo un impacto significativo sobre la QoV (p<0,01). En todas las métricas de QoV, independientemente de la valoración del desenfoque de cerca, media distancia, o de lejos, la QoV fue clasificada de manera superior por los pacientes cuyas tareas principales se centraban en la visión de lejos (n=231, 43,9%), que aquellos pacientes que realizaban tareas de visión intermedia (n=165, 31,4%), y aún peor por los pacientes cuyas tareas principales se centraban en la visión de cerca (n=130, 24,7%), independientemente de la forma de corrección.
ConclusiónLa mayoría de las tareas se realizan a distancia, teniendo éstas una QoV superior que las tareas de visión intermedia, siendo aún peores las tareas realizadas con visión de cerca. Es importante debatir con los pacientes la distancia principal de las tareas que realizan generalmente, y la forma de corrección utilizada desde un principio.
It has been estimated using multiple population-based surveys that around 1.04 billion people globally have presbyopia.1 The median age of the general population in the UK has shifted from 33.9 years in 1974 to 40.0 years in 2014 and it is projected to increase to 42.9 years in 2031.2,3 The traditional non-surgical methods to correct presbyopia are single-vision distance and near, bifocals, and progressive spectacles lens together with contact lens modalities. The desirability of restoring presbyopes with clear vision at all distances involves both fixed and variable focus lens systems, and surgical methods which modify the optics of the cornea, replacing the crystalline lens with different fixed optics, or attempting to at least partially restore active accommodation.4 Inadequate near vision correction due to presbyopia can have a negative effect on daily living, career opportunities and self-esteem.5 Previous epidemiology research has a greater focus on distance rather than on near visual loss.6 Research undertaken reports that functional presbyopia results in difficulty with near tasks in 53% of Indians,7 58% Brazilians8 and 70% of rural Tanzanians.9 In the developed world, inadequate near vision correction can still occur, with a Finnish study finding 6.1% of the population reported difficulty in reading while 1.5% of those could not read newsprint at all with their refractive correction.10
There are limited scientific reports on the usage of refractive correction in presbyopes. Bastawrous and colleagues11 studied the prevalence of refractive error and the spectacle coverage in patients over 50 years old and found that the myopia was more common than hyperopia (affecting 59.5% compared to 27.4%). Market reports generally do not differentiate presbyopes from pre-presbyopes, but demonstrate that the use of corrective eyewear in the UK is very common and has not changed greatly from 2011 (62% in 2011 to 69% in 2013). More women than men wear both glasses (72% versus 66%) and contact lenses (16% versus 11%), with 82% of people in the UK either wearing corrective eyewear or having had laser eye surgery.12
An indicator of satisfaction from the use of visual correction is vision-related quality-of-life among patients. Two different individuals may have the same visual function, but with different perception of their vision-related quality-of-life. There are several questionnaires that have been developed specifically for evaluating vision-related quality-of-life in patients with refractive errors.13–17
The QoV assessment tool developed consisting of a Rasch tested, linear scaled, 10-item instrument across 3 subscales (frequency, severity and bothersome) providing a QoV score between 0 (good) and 100 (poor) for each subscale.18,19 QoV is a subset of vision-related quality-of-life focusing purely on visual symptoms rather than combining aspects of visual disability and the impact on social function.20 Technology has advanced the range of options for the correction of presbyopia with excellent clinical outcomes reported.18,21,22 While distinct visual corrections for presbyopia have been examined, such as multifocal contact lens and intraocular lens designs,23,24 how individual patients utilise different forms of presbyopic correction is not known or whether some combinations outperform others in terms of subjective QoV.
Hence, the purpose of this study was to determine the use of presbyopic corrections in patients and comparing this with their subjectively reported QoV.
MethodFive hundred and twenty nine sequential patients with healthy eyes who reported using a presbyopic refractive correction, attending communities based in the Royal Borough of Kingston, Greenford, Croydon and Bromley between September 2014 and August 2016 were enrolled in the study. The age of participants were 36 years to 85 years who all reported difficulty reading at near with their distance correction, resulting in the use of a near correction. Less than 5% were under 45 years of age. This was a fair representation of the national presbyopic population due to the varied demographics represented in these locations, sample size and had acceptable degrees of freedom with enough responses for the model to calculate the power in responses. 546 patients were asked to participate and only seventeen patients (3.1%) refused to complete the survey mainly due to time constraints.
The study was approved by the Research Ethics Committee of Aston University and conformed to the tenets of the Declaration of Helsinki. All patients gave their informed consent to take part in the study.
Subjective QoV was assessed by patient's verbally completing the QoV questionnaire developed by McAlinden and colleagues.25 Patients were asked to look at and to familiarise themselves with the interpretation of each of the QoV images which simulate visual symptoms. The patient was required to rate how often they experience each symptom – frequency (never, occasionally, quite often, very often), how severely they experience the symptom – severity (not at all, mild, moderate and severe), and how bothered they were by the symptom – bothersome (not at all, mild, moderate, and severe) during their full waking hours.26 The response was based on how they felt in the past week. The raw questionnaire data was Rasch-scaled onto an interval level scale. The QoV question relating to “blur” was repeated and linked to far, intermediate and near vision, as this question did not specify a particular distance. The analysis was performed with each of these questions respectively including their average score.
Further information as to the percentage of time that they wore different forms of refractive correction, any surgical interventions, frequency of driving and the main working distance for their daily activities was elicited by asking the patient directly. Age and sex demographics were also noted. The ethnicity was not considered due to the difficulty in categorising this in a multicultural environment.
Statistical analysisMultivariate Analysis of Variance was applied to the proportion of time subjects using each refractive correction and with QoV, frequency, severity and bothersome scales as dependent variables, percentage of time wearing each corrective option as covariates and age, sex, driving frequency and principal task distance as fixed factors.
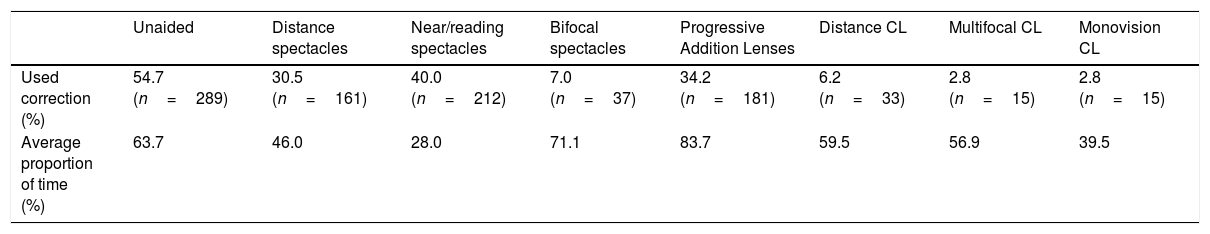
ResultsThe percentage of the cohort that utilised each form of refractive correction with their proportion of time of use is presented in Table 1. Twelve patients had corneal refractive surgery, 40 cataract surgery with the implantation of a monofocal intraocular lens and a further 3 with the implantation of a multifocal intraocular lens; the latter group were excluded from the analysis due to the small cohort size. 260 of the cohort (48.9%) were male. The age profile was: 9.8% (n=52) were under 45 years of age; 18.4% (n=98) were 45–50 years; 16.7% (n=89) were 51–55 years; 10.7% (n=57) were 56–60 years; 12.6% (n=67) were 61–65 years, 7.9% (n=42) were 66–70 years and 23.5% (n=125) were greater than 70 years of age.
The percentage of the cohort that utilised each form of refractive correction with their proportion of time of use. CL=contact lenses. N=529.
| Unaided | Distance spectacles | Near/reading spectacles | Bifocal spectacles | Progressive Addition Lenses | Distance CL | Multifocal CL | Monovision CL | |
|---|---|---|---|---|---|---|---|---|
| Used correction (%) | 54.7 (n=289) | 30.5 (n=161) | 40.0 (n=212) | 7.0 (n=37) | 34.2 (n=181) | 6.2 (n=33) | 2.8 (n=15) | 2.8 (n=15) |
| Average proportion of time (%) | 63.7 | 46.0 | 28.0 | 71.1 | 83.7 | 59.5 | 56.9 | 39.5 |
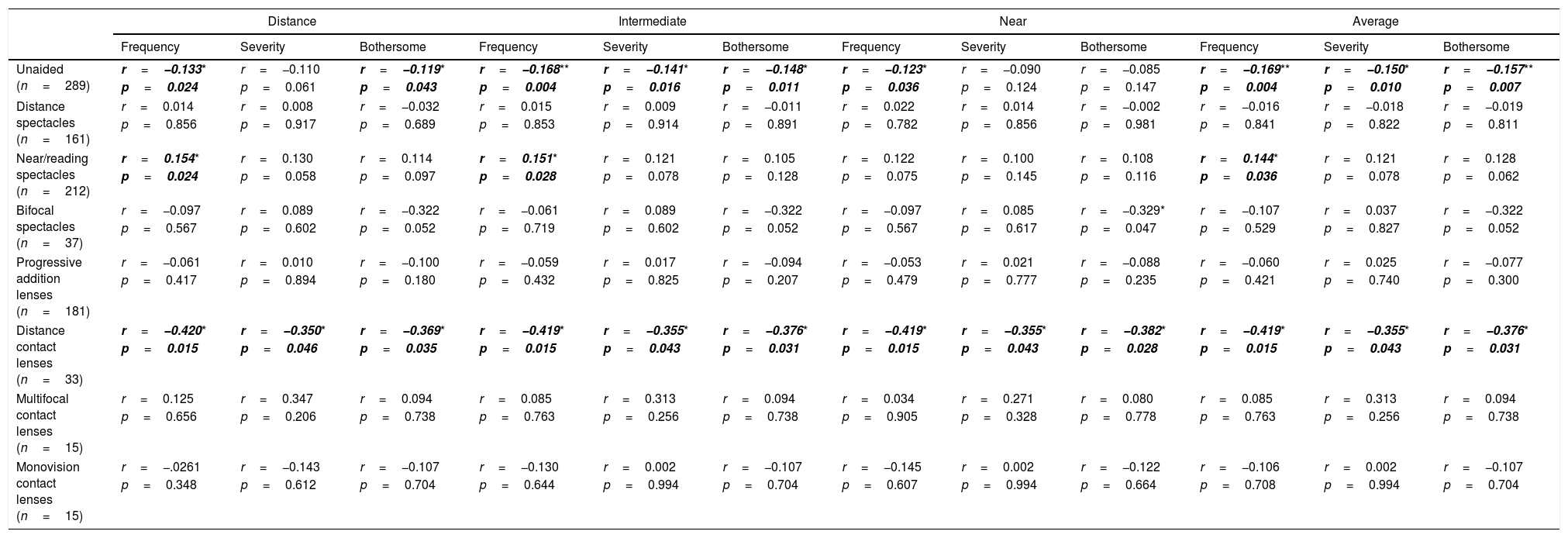
The correlation of the proportion of time the cohort used each of the refractive correction and their (Rasch-scaled) QoV score for distance, intermediate, near and overall vision is reported in Table 2 (note the sample size is limited for statistical analysis of presbyopic contact lens correction). The higher the proportion of time unaided or using distance contact lenses, the better the visual quality (lower score), whereas other corrections were generally not correlated with QoV.
Association between the proportion of time that an individual utilised different forms of refractive correction and QoV Rasch score. Significant results in bold *p<0.05, **p<0.01.
| Distance | Intermediate | Near | Average | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Frequency | Severity | Bothersome | Frequency | Severity | Bothersome | Frequency | Severity | Bothersome | Frequency | Severity | Bothersome | |
| Unaided (n=289) | r=−0.133* | r=−0.110 | r=−0.119* | r=−0.168** | r=−0.141* | r=−0.148* | r=−0.123* | r=−0.090 | r=−0.085 | r=−0.169** | r=−0.150* | r=−0.157** |
| p=0.024 | p=0.061 | p=0.043 | p=0.004 | p=0.016 | p=0.011 | p=0.036 | p=0.124 | p=0.147 | p=0.004 | p=0.010 | p=0.007 | |
| Distance spectacles (n=161) | r=0.014 | r=0.008 | r=−0.032 | r=0.015 | r=0.009 | r=−0.011 | r=0.022 | r=0.014 | r=−0.002 | r=−0.016 | r=−0.018 | r=−0.019 |
| p=0.856 | p=0.917 | p=0.689 | p=0.853 | p=0.914 | p=0.891 | p=0.782 | p=0.856 | p=0.981 | p=0.841 | p=0.822 | p=0.811 | |
| Near/reading spectacles (n=212) | r=0.154* | r=0.130 | r=0.114 | r=0.151* | r=0.121 | r=0.105 | r=0.122 | r=0.100 | r=0.108 | r=0.144* | r=0.121 | r=0.128 |
| p=0.024 | p=0.058 | p=0.097 | p=0.028 | p=0.078 | p=0.128 | p=0.075 | p=0.145 | p=0.116 | p=0.036 | p=0.078 | p=0.062 | |
| Bifocal spectacles (n=37) | r=−0.097 | r=0.089 | r=−0.322 | r=−0.061 | r=0.089 | r=−0.322 | r=−0.097 | r=0.085 | r=−0.329* | r=−0.107 | r=0.037 | r=−0.322 |
| p=0.567 | p=0.602 | p=0.052 | p=0.719 | p=0.602 | p=0.052 | p=0.567 | p=0.617 | p=0.047 | p=0.529 | p=0.827 | p=0.052 | |
| Progressive addition lenses (n=181) | r=−0.061 | r=0.010 | r=−0.100 | r=−0.059 | r=0.017 | r=−0.094 | r=−0.053 | r=0.021 | r=−0.088 | r=−0.060 | r=0.025 | r=−0.077 |
| p=0.417 | p=0.894 | p=0.180 | p=0.432 | p=0.825 | p=0.207 | p=0.479 | p=0.777 | p=0.235 | p=0.421 | p=0.740 | p=0.300 | |
| Distance contact lenses (n=33) | r=−0.420* | r=−0.350* | r=−0.369* | r=−0.419* | r=−0.355* | r=−0.376* | r=−0.419* | r=−0.355* | r=−0.382* | r=−0.419* | r=−0.355* | r=−0.376* |
| p=0.015 | p=0.046 | p=0.035 | p=0.015 | p=0.043 | p=0.031 | p=0.015 | p=0.043 | p=0.028 | p=0.015 | p=0.043 | p=0.031 | |
| Multifocal contact lenses (n=15) | r=0.125 | r=0.347 | r=0.094 | r=0.085 | r=0.313 | r=0.094 | r=0.034 | r=0.271 | r=0.080 | r=0.085 | r=0.313 | r=0.094 |
| p=0.656 | p=0.206 | p=0.738 | p=0.763 | p=0.256 | p=0.738 | p=0.905 | p=0.328 | p=0.778 | p=0.763 | p=0.256 | p=0.738 | |
| Monovision contact lenses (n=15) | r=−.0261 | r=−0.143 | r=−0.107 | r=−0.130 | r=0.002 | r=−0.107 | r=−0.145 | r=0.002 | r=−0.122 | r=−0.106 | r=0.002 | r=−0.107 |
| p=0.348 | p=0.612 | p=0.704 | p=0.644 | p=0.994 | p=0.704 | p=0.607 | p=0.994 | p=0.664 | p=0.708 | p=0.994 | p=0.704 | |
The proportion of time subjects used each refractive correction accounted for over 10% (adjusted r2≤0.1) of the variance in QoV metrics.
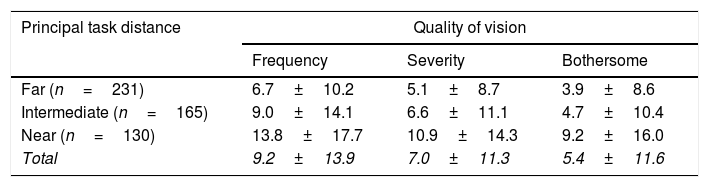
Age, sex and driving frequency had no effect of QoV (p>0.05), whereas principal task distance significantly impacted QoV (p<0.01). In all QoV metrics, regardless of the far, intermediate or near blur assessment, quality of vision was rated as better by patients whose main tasks were far focused (n=231, 43.9%), than those who principally conduct intermediate tasks (n=165, 31.4%) and worse still by those whose tasks were near focused (n=130, 24.7%), regardless of the form of correction (Table 3).
QoV scores (mean±S.D. – average of far, intermediate and near focused blur questions) with the principal task distance as identified by patients.
| Principal task distance | Quality of vision | ||
|---|---|---|---|
| Frequency | Severity | Bothersome | |
| Far (n=231) | 6.7±10.2 | 5.1±8.7 | 3.9±8.6 |
| Intermediate (n=165) | 9.0±14.1 | 6.6±11.1 | 4.7±10.4 |
| Near (n=130) | 13.8±17.7 | 10.9±14.3 | 9.2±16.0 |
| Total | 9.2±13.9 | 7.0±11.3 | 5.4±11.6 |
This study aimed to assess real-world adoption of presbyopic corrections and their impact on quality of vision. The study was representative of the presbyopic population of the UK with relatively few presbyopes below the age of 45 years and most of the population being between the ages of 45 to 65 years. The proportion of over 60 years has increased from 8% in 1950 to 11% in 2009 and it is estimated to be 22% in 205027 with advances in healthcare and quality of living standards. The main forms of optical correction in the study population were separate pairs of distance and near spectacles and progressive addition lenses with just 2.8% using multifocal and 2.8% using monovision contact lenses. Few had had refractive surgery (as has been previously identified)28 and only 8% of those who had had cataract surgery had a multifocal intraocular lens implanted. Multifocal intraocular lens are more expensive and are not normally an option within the National Health Service.29 Despite their benefits of uncorrected visual acuity at multiple distances,30 reduced contrast sensitivity, haloes and glare are greater with a multifocal intraocular lens than with a monofocal intraocular lens.31
Over half of the population managed without glasses at least some of the time; some myopes can cope unaided for near tasks, but the proportion of time the participants were unaided was also high suggesting not all visual tasks have a high acuity demand. Between 30% and 40% of patients wore distance, reading and progressive spectacles with those using Progressive Addition Lenses wearing them over 80% of the time while those wearing reading spectacles only approximately 25% of the time. This is as might be expected as reading glasses do not provide distance or intermediate vision. Bifocals were worn less commonly, but for those who did, they utilised them most of the time.
Morgan and his co-authors’ survey identified a significant under-prescribing of presbyopia-correcting contact lenses for those 45 years of age and older.27 The same finding was identified in this more systematic data collection; contact lenses worn in the presbyopic age group were mostly only for distance correction (approximately double the multifocal contact lenses and monovision usage, which were equal at 2.8%). However, distance and multifocal contact lenses wearers wore their correction longer (for about 60% of the time) whereas monovision wearers wore the contact lenses for 40% of the time. This may reflect the research showing that the current multifocal contact lens designs outperform monovision in presbyopes.32
QoV improved (score reduced) with the amount of time a patient was uncorrected or wore distance contact lenses, but generally worsened with the amount of time they wore reading glasses. There was no impact of distance spectacle use, bifocal/progressive addition lens spectacles and multifocal/monovision contact lens options on QoV, although the latter may be due to the low patient numbers wearing these forms of correction. This implies more cosmetically ‘natural’ options (uncorrected or wearing contact lenses) improve QoV while the inconvenience of physically having to change a refractive correction to see at near may hinder QoV. It was not possible to adequately model the effect of different refractive corrections on QoV.
Surprisingly, over half of the patients identified their principal tasks as generally at far distances and these individuals reported a consistently better QoV than those who identified their primary tasks as being at closer distances. Those, whose principal tasks were identified as being at closer distances reported poorer QoV, regardless of the form of correction worn. As the relative task distance observed by an individual affected their QoV results, splitting the blur question by the distance of the task should be considered for the future use of the QoV questionnaire to better understand the impact of presbyopic corrections.
In conclusion, the majority of presbyopes principally undertake far distance tasks and these individuals had a better QoV than those whose tasks were principally at an intermediate distance and even worse was the QoV of those with principally near focused tasks. Hence, it is important to ask patients about the principal distance of the tasks they generally perform. Most patients use more than one form of correction so this should be discussed with patients from the outset.
Conflicts of interestNone of the authors have a conflict of interest with the topic of the research.