To report the practice of orthokeratology (OK) in Algeria and to investigate the visual outcomes, safety and subjective responses with this technique in myopes.
MethodsA retrospective chart review of 48 participants using OK lenses since January 2010 were included in the study. Lenses were selected and fitted according to the manufacturer’s recommendations using their respective software and the number of lenses required for a successful fit was recorded. Visual acuity (VA) in logMAR units and biomicroscopic findings were recorded for each visit. Subjective ratings was determined with analogue rating scale was filled in by the investigator, the participants were divided into Group 1 (> 4.00D) and Group 2 (< 3.75D) myopic groups for analysis.
ResultsFirst lens fitting success rate of 64.58%. There was also a significant difference between the BCVA at baseline and VA at Day 1 (P < 0.05), and no significant difference at Day 7, Day 30 and the final visit (P = 0.51, P = 0.93, P = 0.62, respectively), for Group 2. There was a significant difference between the BCVA at baseline and VA at Day 1, 7, 30 and the final visit (P < 0.05), for Group 1. the patients of the second group were happier but the results from the survey were not statistically significant (P = 0.10), no serious complication was reported.
Conclusionthe technique was efficient and safe as we didn’t have any serious complication, with a high success rate for first lens fitting.
Due the increasing prevalence of myopia worldwide in the last century,1 myopia control (MC) is increasing in practice to help control this epidemic.2 In order to prevent retinal complications due to high myopia (>6D),3 North America, Asia and Europe healthcare systems4,5,6 have been established protocols to control this epidemic and prevent the visual burdens resulting from devastating complications such as retinal detachments, glaucoma and cataracts.1,7 Africa has many epidemics related to healthcare, however eyecare programmes in this continent were mainly focused on managing diseases such as cataracts and retinal pathology related to diabetes.8,9 In fact, Algerian and North African populations are growing quickly and myopia is the most common refractive error due to hereditary and genetic factors.9,10 However, the exact data of myopia or refractive errors prevalence in Algeria is not available.
In their worldwide survey of myopia management attitudes and strategies in clinical practice, Wolffsohn et al.11 investigated MC globally and found that Orthokeratology (OK) is perceived as the most effective tool in MC by practitioners from 971 completed survey responses. Seven of these responses were from Africa but were not included in the analysis. In fact, Algeria currently has a few orthokeratology practitioners (7–10), either ophthalmologists or optometrists, who mostly work in referral contact lens centres.
Examining Orthokeratology internationally, a recent survey12 was done to investigate the extent of this technique’s use worldwide and to characterize associated demographics and fitting patterns. Differences were found from one continent to others as well as countries, attributed to the training, attitudes and the culture of rigid lens fittings supported by local laboratories.
The safety of the technique is also well investigated13,14 as it may lead to dangerous and irreversible complications such as Acanthamoeba keratitis15 and other corneal infectious disorders.16 Although, contact lens (CL) wear is associated with an increased rate of microbial keratitis (MK), Stapleton et al. reported an incidence ratio of 1.9 per 10 000 in daily wear soft CL wearers and 19.5 per 10 000 for soft CL overnight wear.17 On the other hand, Bullimore et al. reported an incidence of MK of 7.7 per 10,000 for overnight corneal reshaping contact lenses (OK). However, the rates are still very low with both modalities and there is no vision loss when treated appropriately.18
Orthokeratology has been practiced in Algeria for over 10 years but to the author’s knowledge no study has been published to investigate the outcomes of this refractive technique in this part of the world. Patients’ subjective rating of satisfaction needs to be investigated and compared between high and low myopia as it may differ.19
The purpose of this study is to report the practice of orthokeratology in Algeria and to investigate the visual function results, safety and subjective responses with this technique in myopes.
Despite the missing myopia control data reported in this study (cycloplegic refraction, pupil size, axial length, evolution over time, etc), the ultimate purpose of this article is to encourage this technique in Algeria, North Africa and the middle east in order to prevent myopia progression and its increasing prevalence.
Materials and methodsParticipantsData were gathered from 48 eyes (48 patients) from the clinical charts at the Contact Lens and Ophthalmology Centre, Ibn Al Haythem, Algiers, Algeria, Informed consent was obtained from all participants according to the Tenets of the Declaration of Helsinki.
Contact lensesTwo types of lenses were fitted, the first type was the DRL or Double Reservoir Lens (DRL) (Precilens, Paris, France)20 which was empirically calculated according to the manufacturer’s software which considered the corneal topographic values and refractive error.
The Double Reservoir Lens is a five-zone lens which main characteristics is the third curve (after the reverse curve) flatter than the second one, and the fourth curve steeper than the third one in order to create a second lacrymal reservoir.
DRL lenses are made of a Boston XO2 (Hexafocon B) material with an oxygen permeability of 141 barriers, refractive index of 1.424 and wetting angle of 38 degrees measured with the captive bubble method.
The second type of lens was the Z Night, Menicon ZNight (NKL Contactlenzen, Netherlands) that is manufactured with Menicon Z material Tisilfocon A (Menicon Co, Ltd, Nagoya, Japan) having an oxygen permeability of 189 barriers, refractive index of 1.44 and wetting angle of 24 degrees measured with the captive bubble method.
Menicon Z Night is a reverse geometry contact lens. The base curve is responsible for central flattening and the reverse curve is the link between the central and tangential peripheral parts of the lens. The tear reservoir zone is located in the reverse curve, which, together with the three fenestrations, allows optimum tear exchange. The tangential curve allows adequate centration.
Fitting philosophyAll fittings were optimized until centration and the correct refractive outcomes were achieved.
For the fitting of DRL orthokeratology lenses, we used the empirical method using the Click&Fit software calculator and for the Menicon Z Night, the Easyfit software calculator based on refractive and topographic readings, the modifications of parameters were also based on fluorescein pattern, corneal topography follow-ups.
The first lens success rate data was also collected.
Study designA retrospective chart review of all participants using OK lenses since January 2010 were included in the study.
Exclusion criteria: patients who stopped the treatment or didn’t came back for follow-up before 1 month were excluded from the study.
Patients with higher myopia (above 6D) at baseline were excluded.
ProcedureCorneal topography was measured at their initial trial fitting appointment using the Keratron™ Piccolo Topographer (Optikon, Italy).
The visits that were examined after baseline were at 1,7–10,30 days and the final exam was after 1–6 years from the initial fitting. Visual acuity (VA) in logMAR units and biomicroscopic findings were recorded for each visit.
Over-refraction was evaluated but not gathered in the data collection.
The analysis was limited after 1 year of wear for all participants.
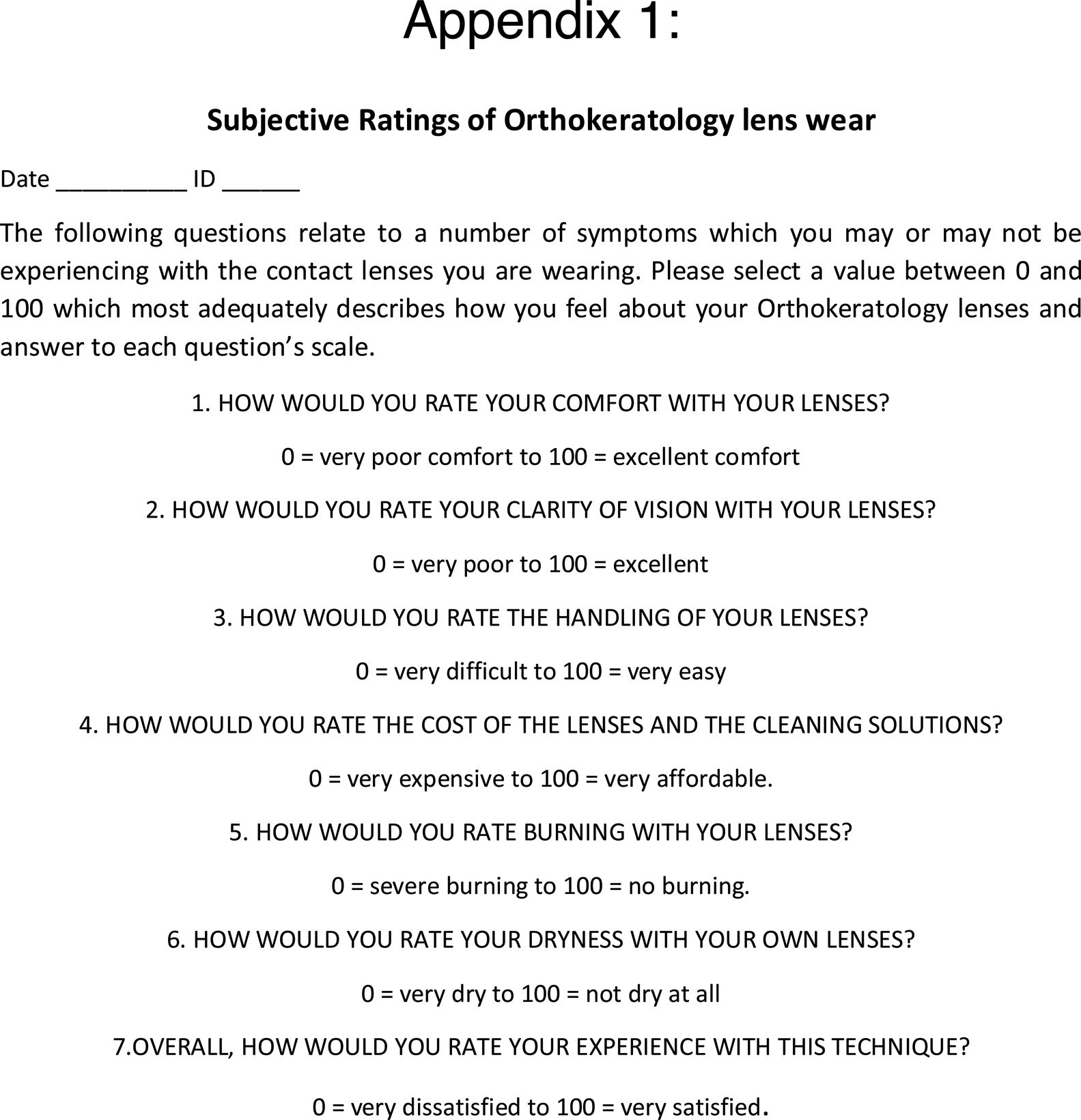
For the subjective ratings of comfort, vision and quality of life, a phone call was conducted and a subjective analogue rating scale from 0 (Poor) to 100 (Excellent) was filled in by the investigator according to the participants’ responses.
Statistical analysisAll data described above was analysed from both eyes of each participant from each visit. Data analysis were conducted using STATISTICA 7 (Statsoft Inc., Tulsa,
TX, USA). Descriptive statistics are provided for information regarding baseline variables (age, gender, refractive error distribution, etc.) and the number of lenses required for a successful fit were tabulated.
The participants were further divided into Group 1 (> 4.00D) and Group 2 (< 3.75D) myopic groups for analysis, and comparisons between the 2 groups, regarding vision and subjective analogue rating scales were completed using RM-ANOVA and Student’s t-test. P values less than 0.05 were considered significant.
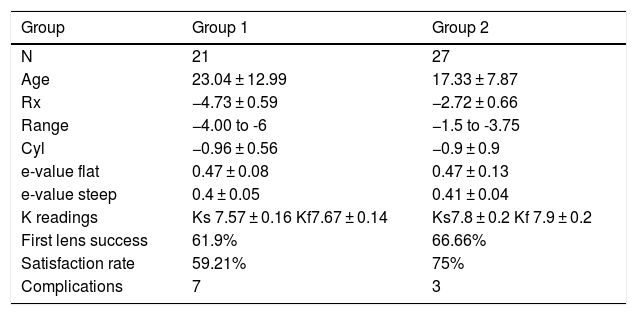
ResultsA total of 48 participants (eyes) with a mean age of 20.63 ± 10.81 (ranging from 5 to 55 years), 33% males and 67% females were analysed. The results with the participants divided into two groups are summarised in Table 1.
The Group 1 had 28% Males and 72% females, Group 2 had 30% Males and 70% Females.
| Group | Group 1 | Group 2 |
|---|---|---|
| N | 21 | 27 |
| Age | 23.04 ± 12.99 | 17.33 ± 7.87 |
| Rx | −4.73 ± 0.59 | −2.72 ± 0.66 |
| Range | −4.00 to -6 | −1.5 to -3.75 |
| Cyl | −0.96 ± 0.56 | −0.9 ± 0.9 |
| e-value flat | 0.47 ± 0.08 | 0.47 ± 0.13 |
| e-value steep | 0.4 ± 0.05 | 0.41 ± 0.04 |
| K readings | Ks 7.57 ± 0.16 Kf7.67 ± 0.14 | Ks7.8 ± 0.2 Kf 7.9 ± 0.2 |
| First lens success | 61.9% | 66.66% |
| Satisfaction rate | 59.21% | 75% |
| Complications | 7 | 3 |
This study had a success rate of 64.58% for first lens fitting in the overall sample. 27.55% of the changes were only after a single change. The high myopes had 61.9% and low myope group had 66.66% of first lens success which was significantly different (P = 0.018).
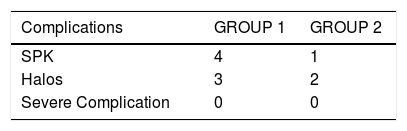
There were 7 non-significant complications such as SPK and halos. 70% of the complications were in the first group, whereas 30% were in the second group. All the complications were non-significant and all the participants who had an interruption of lens wear were able to resume wear of their OK lenses.
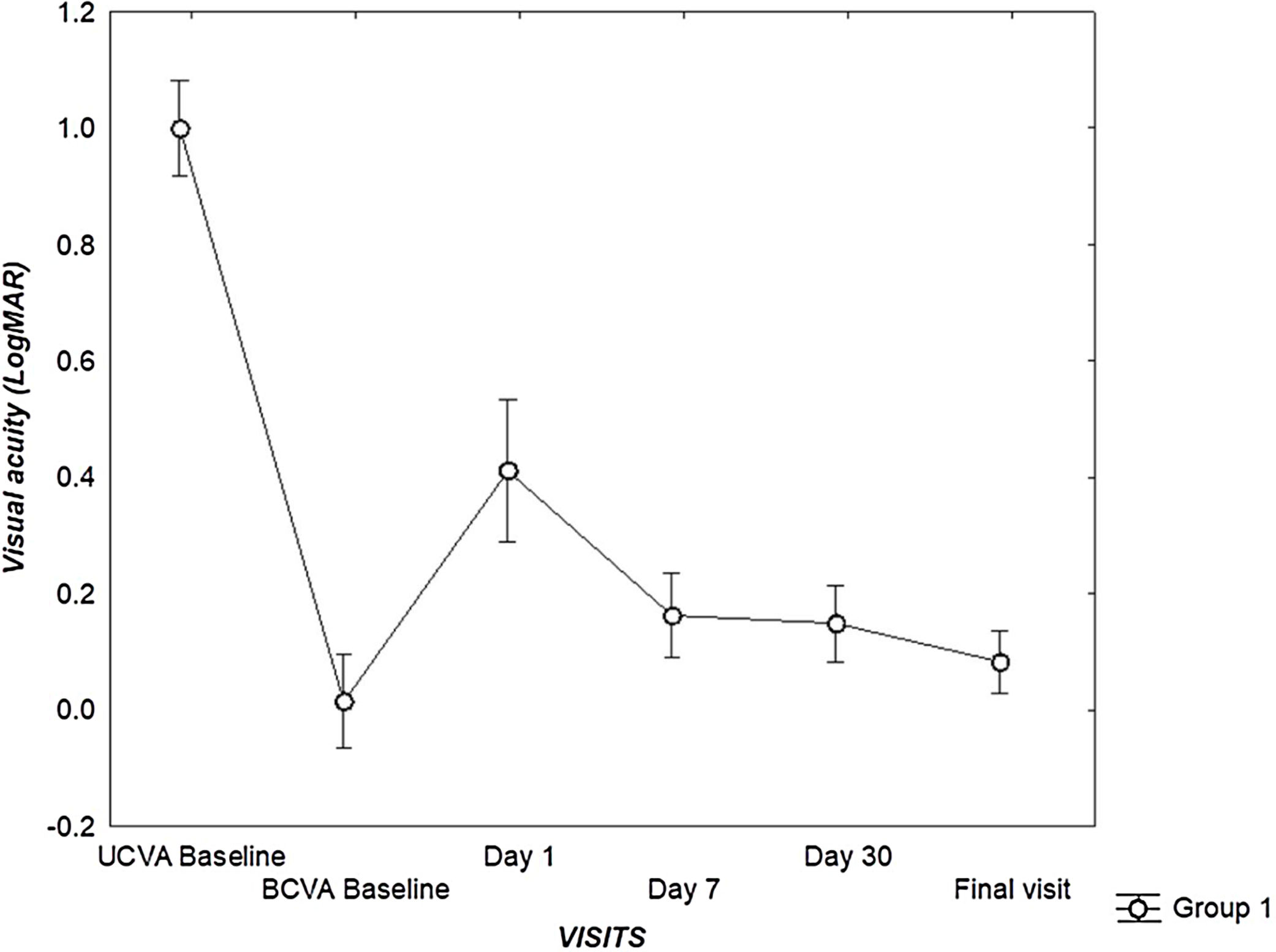
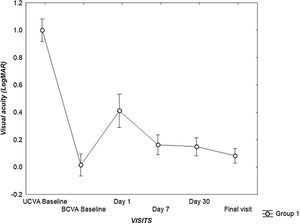
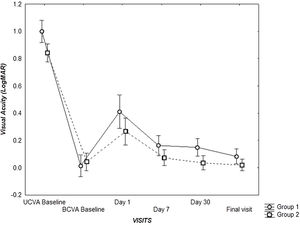
There was a significant difference between the BCVA at baseline and VA at Day 1, 7–10, 30 and the final visit (P < 0.05), for Group 1.
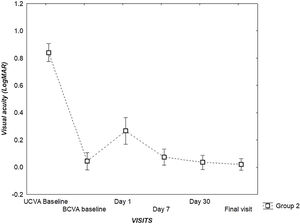
There was also a significant difference between the UVA at baseline and VA at Day 1,7–10,30 and the final visit (P < 0.05), for Group 1. (Fig. 1).
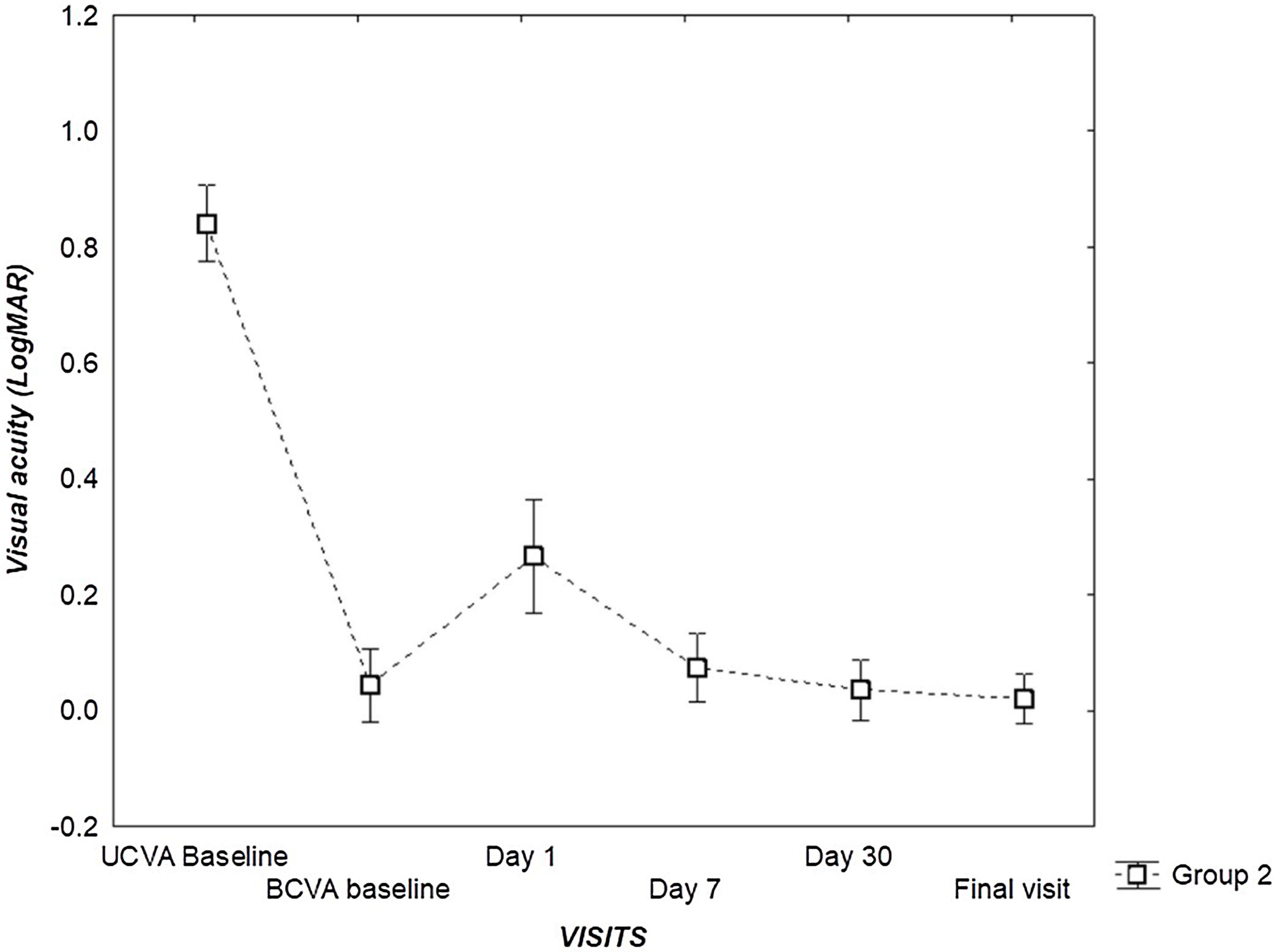
There was a significant difference between the UCVA at baseline and VA at Day 1, Day 7, Day 30 and the final visit (P < 0.05), for Group 2.
There was also a significant difference between the BCVA at baseline and VA at Day 1 (P < 0.05), and no significant difference at Day 7, Day 30 and the final visit (P = 0.51, P = 0.93, P = 0.62, respectively), for Group 2. (Fig. 2).
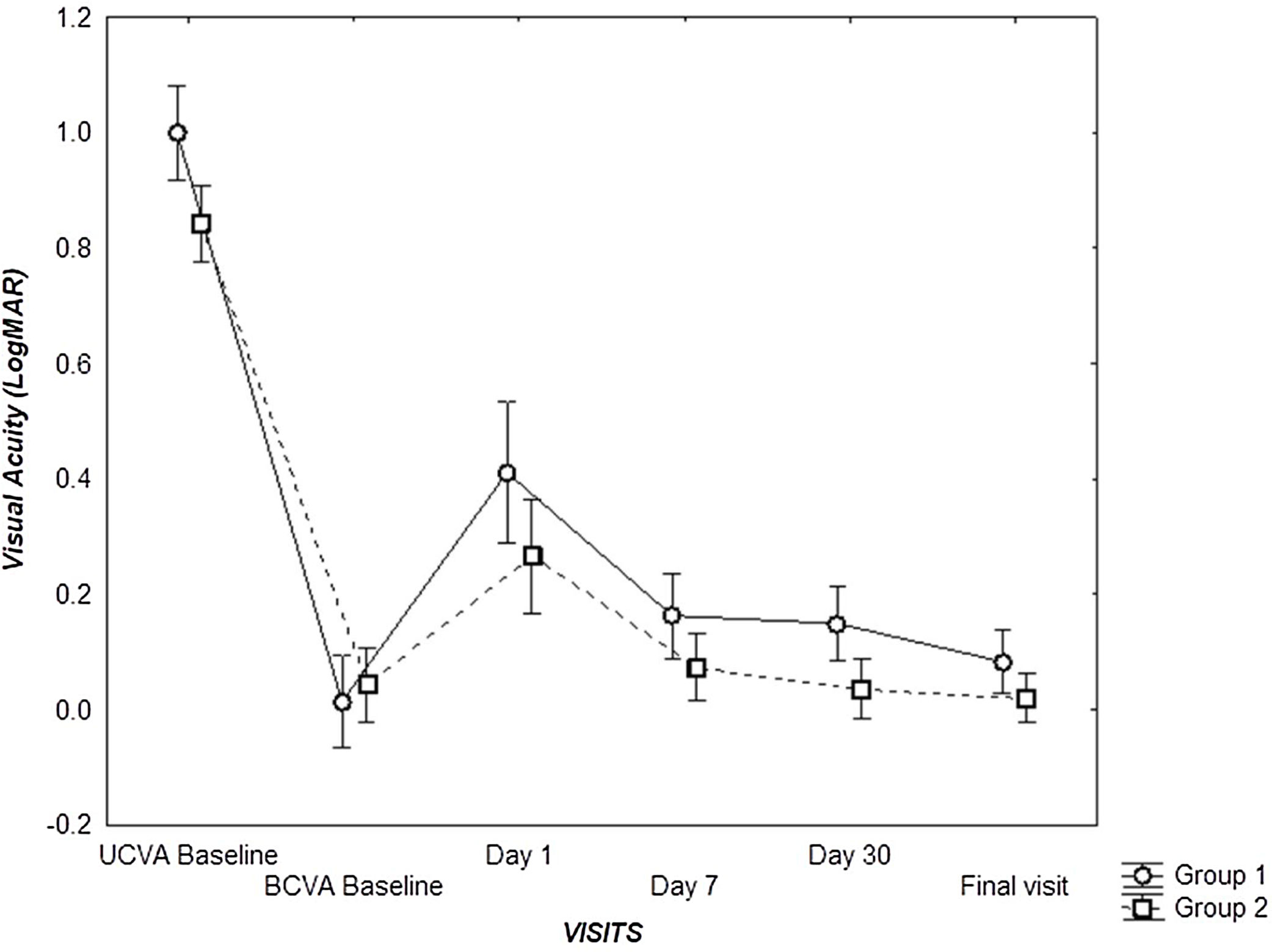
There was a significant difference between the two groups for the unaided VA at baseline P = 0.02, but no difference for the BCVA at baseline.
There was a significant difference between VA for the two groups at day 30, and at final visit (P = 0.001), but no difference at Day 1 and Day 7 visits (P = 0.13) (Fig. 3).
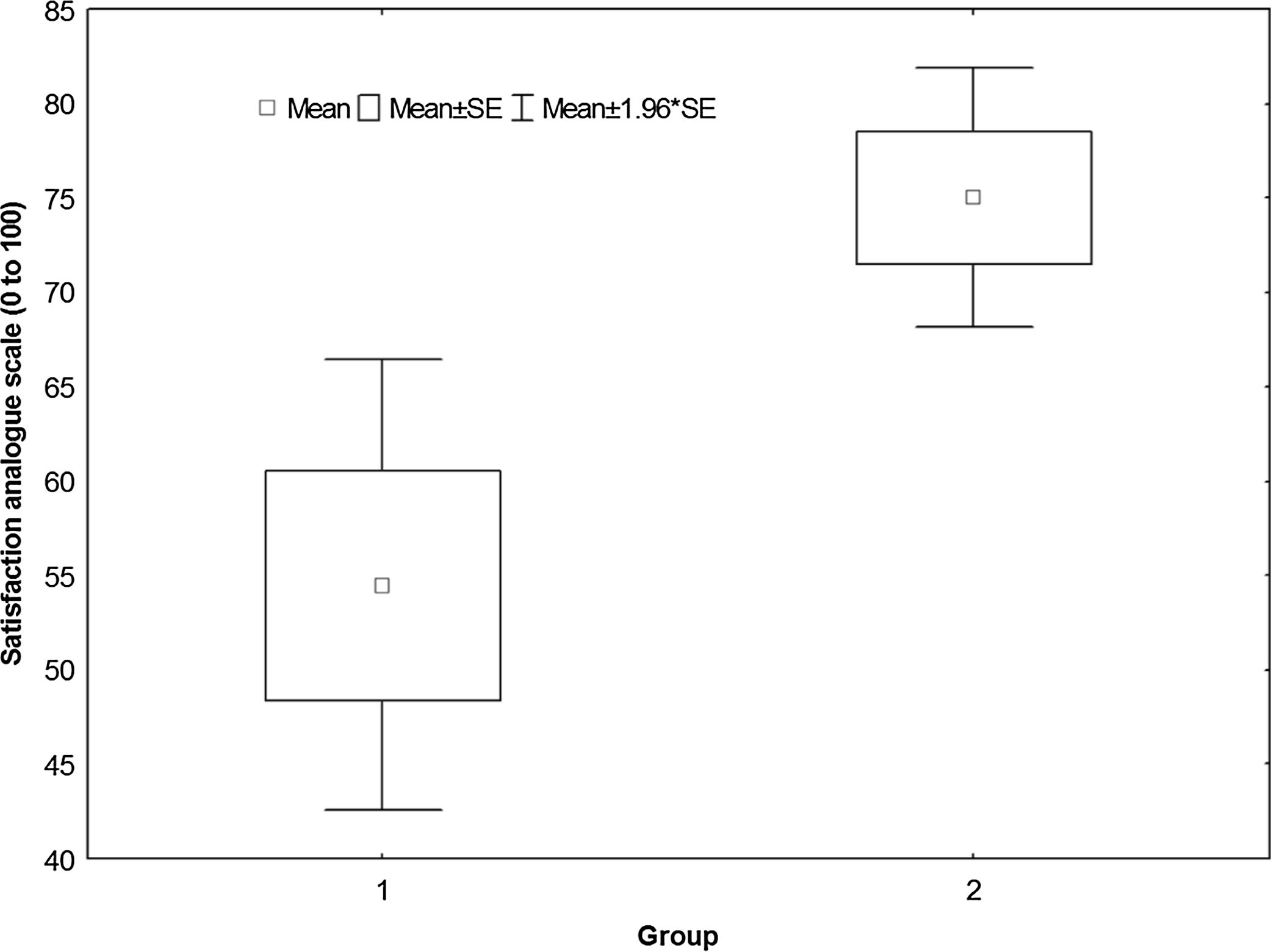
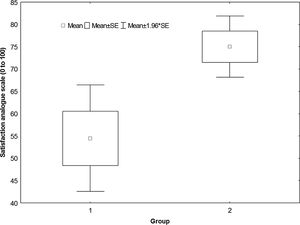
There was no significant difference between the subjective responses for the two groups (P = 0.10), with means of 59.21 ± 38.37 for the Group 1 and 75 ± 26.58 for the Group 2 (Where: 0 = Poor, 100 = Excellent) (Fig. 4).
DiscussionThis study investigated the outcomes of orthokeratology for myopia control in a clinical population at a national referral contact lens clinic in Algeria.
There were more females than males in this study. This was reported in several studies.21 On the other hand, Morgan et al.12 had a male dominance in their survey, and declared that the reason for the higher proportion of OK fits among males is unclear. The mean age of the sample was also young, likely because orthokeratology has been used for myopia control. It is common to find OK studies with younger participants.22,12
With modern orthokeratology, most of manufacturers prefer to use computer software for the fitting of OrthoK lenses for their customers. This software appears to be optimized for the low myopic group as they had a higher first lens success as the outcomes of this technique and study have predicted. Chan et al.23 published a study to report the clinical performance of the OrthoK lens fitted with a computer assisted system and showed 90% of first fit success rate. Maldonado et al.24 also investigated the first lens success rate, comparing fitting approaches and designs, where for the nine subjects who completed this study, six were fitted successfully with the first lens manufactured. The three other participants needed changes in the first manufactured lens. One of these participants was successfully fitted with the second lens, however modifications were needed again for the last two patients. The success rate was similar to this study.
It is well established that vision correction is efficient with orthokeratology treatment.25,26 In this study there was no difference in vision for the second group but significant decrease in vision for the first group when compared to their best corrected spectacles. Hiraoka et al. revealed that post-OrthoK treatment UCVA and pre-OrthoK treatment myopic error were significantly correlated. It is reasonable for post-treatment UCVA to be a major factor that affects patient satisfaction, and they explained this importance because candidates for orthokeratology have a fundamental desire to be free from optical aids by improving UCVA.27 In addition, in our study the vision got slightly worse as the baseline myopia increases.
This difference could be addressed by the fitting spectacles for any residual error, as Charm et al. reported a high myopia partial correction with orthokeratology, where they targeted a 4 dioptres of myopia with the lenses and corrected the residual error with single vision spectacles.28
However, it is known that orthokeratology induces changes in epithelial pachymetry with thinning centrally and mid-peripheral thickening,30,31 It was also shown that orthokeratology treatment alters some corneal biomechanical properties.32 In their pilot study, González-Méijome et al., assume a faster response to orthokeratology and faster recovery for corneas with lower resistance in short term.33
Lifshitz et al.34 performed a clinical study to attempt to correlate central corneal thickness (CCT) with participants’ baseline CCT and they effectively found that participants of North African origin had statistically significantly thinner corneas than participants of other origins (P < 0.00001). Lazreg et al.35 later in one of the rare studies with this population investigated the corneal pachymetry and biomechanics compared to French participants presenting to refractive surgery clinics, where they also found thinner and lower elastic resistant (biomechanics) corneas in this North African population. Moreover, many studies of corneal shape and curvature have shown that there is no difference with other ethnicities and the compatibility with current OrthoK lenses designs.36,37,38
It may be induced that the North African population having thinner and less elastic resistance may not be able to be easily deformed, or does not maintain its shape, when high refractive errors are attempted to be corrected with orthokeratology.
By modifying the anterior corneal shape with OK lenses, light distortion specially halos, are frequently reported by patients after wear, it could be transient or permanent, Santolaria et al. analysed subjective satisfaction in long-term orthokeratology patients, and concluded that patient subjective satisfaction with visual outcomes is high and improves over the first year of treatment, and explained the improvement by a possible form of neuroadaptation.39 In this study we did not objectively measured high order aberrations but patients did reported halos.
Hiraoka et al.27 in the first study where UCVA and baseline myopia error were associated with patient satisfaction after overnight orthokeratology, used a visual analogue scale to find factors that influence patient satisfaction. The analogue scale was also used by Rushood et al.29 to measure the level of satisfaction after refractive surgery for low myopia in a simple, reproducible, and a quick manner, Rose et al19 in their study of quality of life with 112 myopic patients, who were divided into groups by degree of refractive error, concluded that high myopia has an adverse effect on quality of life equivalent to that of keratoconus. In this study, we investigated for low myopia also, the subjective responses of myopes corrected with Orthokeratology categorised by their degree of refractive error. There was also a reduction in the subjective rating correlated with increasing myopia when corrected with OK lenses, the patients of the second group were happier but the results from the survey were not statistically significant, the reasons of the rating were mainly about vision, comfort, cost and lenses handling, however we did not used a peer reviewed questionnaire available for the analysis of quality of life impacts for refractive procedures e.g. Lasik.
Microbial keratitis is the most common complication with orthokeratology.18,21 Many OK studies13,16,14 have shown the presence of complications and have shown serious sight threatening complications that can occur, but they did not occur in this study, where the most concerning complication we had, was superficial punctate keratitis, mostly in the first group and less in the second one.
Careful monitoring of corneal health was conducted and when staining was more frequently observed, lens wear was temporarily discontinued until resolution, which lead to this positive result. It appears that central corneal staining may be related to the amount of corneal flattening induced by OK. In a systemic review, Liu et al. reported that higher baseline myopia was reported to be positively associated with the level of staining,13 which was also noticed in our results.
A limitation of this study is the sample size, which, compared to the prevalence of myopia, may be considered to be low. It may be preferred to have had a clinical research trial in order to collect the quality of life (using a peer reviewed questionnaire) information while the study was being conducted rather than retrospectively. Future studies could include Axial length measurements, pachymetry and topographic curvature changes to better describe the differences that we found in our results compared to other populations.
ConclusionThis study reported that the use of orthokeratology in 48 young myopes in Algeria is safe as no serious complication were observed with a high success rate for first lens fitting. The results are promising and encourage to use orthokeratology in the region.
Conflicts of interestThe authors have no conflicts of interest to declare.
Financial disclosuresThis research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
The authors thank Dr Luigina Sorbara and Dr Gabriella Courey for editorial advice.