Optical coherence tomography (OCT) is a non-invasive method for diagnosis and monitoring of retinal (typically, macular) conditions. The unfamiliar nature of OCT images can present considerable challenges for some community optometrists.
The purpose of this research is to develop and assess the efficacy of a novel internet resource designed to assist optometrists in using OCT for diagnosis of macular disease and patient management.
MethodsAn online tool (OCTAID) has been designed to assist practitioners in the diagnosis of macular lesions detected by OCT. The effectiveness of OCTAID was evaluated in a randomised controlled trial comparing two groups of practitioners who underwent an online assessment (using clinical vignettes) based on OCT images, before (exam 1) and after (exam 2) an educational intervention. Participants’ answers were validated against experts’ classifications (the reference standard). OCTAID was randomly allocated as the educational intervention for one group with the control group receiving an intervention of standard OCT educational material. The participants were community optometrists.
ResultsRandom allocation resulted in 53 optometrists receiving OCTAID and 65 receiving the control intervention. Both groups performed similarly at baseline with no significant difference in mean exam 1 scores (p = 0.21). The primary outcome measure was mean improvement in exam score between the two exam modules. Participants who received OCTAID improved their exam score significantly more than those who received conventional educational materials (p = 0.005).
ConclusionUse of OCTAID is associated with an improvement in the combined skill of OCT scan recognition and patient management decisions.
Optical Coherence Tomography (OCT) has become a key diagnostic technology for retinal disease, most notably macular disease. In modern spectral-domain OCT technology, two- or three-dimensional cross-sectional tomographic images of optical reflectivity are captured by this non-invasive technique which delivers a micrometer-scale, cross-sectional image through retinal tissue. This resembles a histological section which is visible without the need for removal and processing of tissue samples.1 OCT scans enable microscopic defects to be easily viewed. In addition, results are reproducible and quantitative. These properties help to explain the widespread use of OCT in clinical practice.2
Although OCT provides accurate and reproducible information in qualitative and quantitative formats, it is challenging for the novice user to acquire the skills to interpret this information correctly. This is because OCT scans reveal retinal detail previously unseen by clinicians and limited guidance exists to assist practitioners using OCT to make diagnostic and referral decisions.3 There is, therefore, a need for training tools to provide optometrists with the knowledge and skills to use OCT for accurate diagnosis and to help them make appropriate management decisions (e.g., what cases to refer to an ophthalmologist and with what urgency, how frequently to monitor, etc.).
Age-related macular degeneration (AMD) is the leading cause of blindness in the developed world.4 The prognosis for an increasing number of patients with neovascular (wet) AMD has improved due to recent developments in anti-vascular endothelial growth factor (anti-VEGF) treatments. This has resulted in an influx of new patients into specialist retinal clinics.5 The timing of the referral is crucial in wet AMD as delay in diagnosis and treatment is associated with severe visual loss.6,7 Ideally, treatment of confirmed wet AMD should be within two weeks of initial development of symptoms or detection of a treatable lesion.8 It has been reported that fewer than half of people suffering from wet AMD in the United Kingdom (UK) receive treatment within the recommended two-week timeframe and 3.5% wait more than eight weeks for an appointment following referral. These statistics are likely to worsen as a result of clinical capacity challenges from the COVID-19 pandemic.
AMD services in the UK hospital eye service have had to adapt to increased demand and this is mirrored in Spain9 and other European countries.10,11 Intravitreal injection of anti-VEGF agents is associated with substantial hospital workload because frequent follow-up of these patients is required and it is difficult to discharge patients to free capacity for new referrals.12,13 The challenges of meeting the demand for these services have been exacerbated by the COVID-19 pandemic.
Community follow-up of previously treated and stable AMD patients by suitably trained optometrists may reduce the burden on hospital-based AMD services and has the advantage of bringing services into the community, closer to the patient. New imaging techniques such as (OCT) are helpful in identifying fundamental diagnostic features of AMD and conditions that can mimic AMD.
Macular disease has a widely variable clinical presentation and a sometimes unpredictable natural history.14 OCT has become a mainstream technology in clinical practice, and is even performed by non-specialist personnel in some settings.15 However, the question of whether OCT becomes the new standard for ocular assessment in optometric practice will be heavily influenced by the quality of education and training of optometrists in interpreting OCT images.
Learning conducted via electronic media is employed by medical educators and web-based delivery of education (e-learning) has revolutionised modes of exchanging information. Optometric educators are embracing this trend. In today’s increasingly technologically-driven learning environment, it is important for optometric educators to consider how to reach students in the most effective way.16 This concept is strongly embedded in this study’s design and rationale.
The aim of this research is to develop and test an online diagnostic guide designed to improve the diagnosis and optometric management of central retinal lesions using OCT.
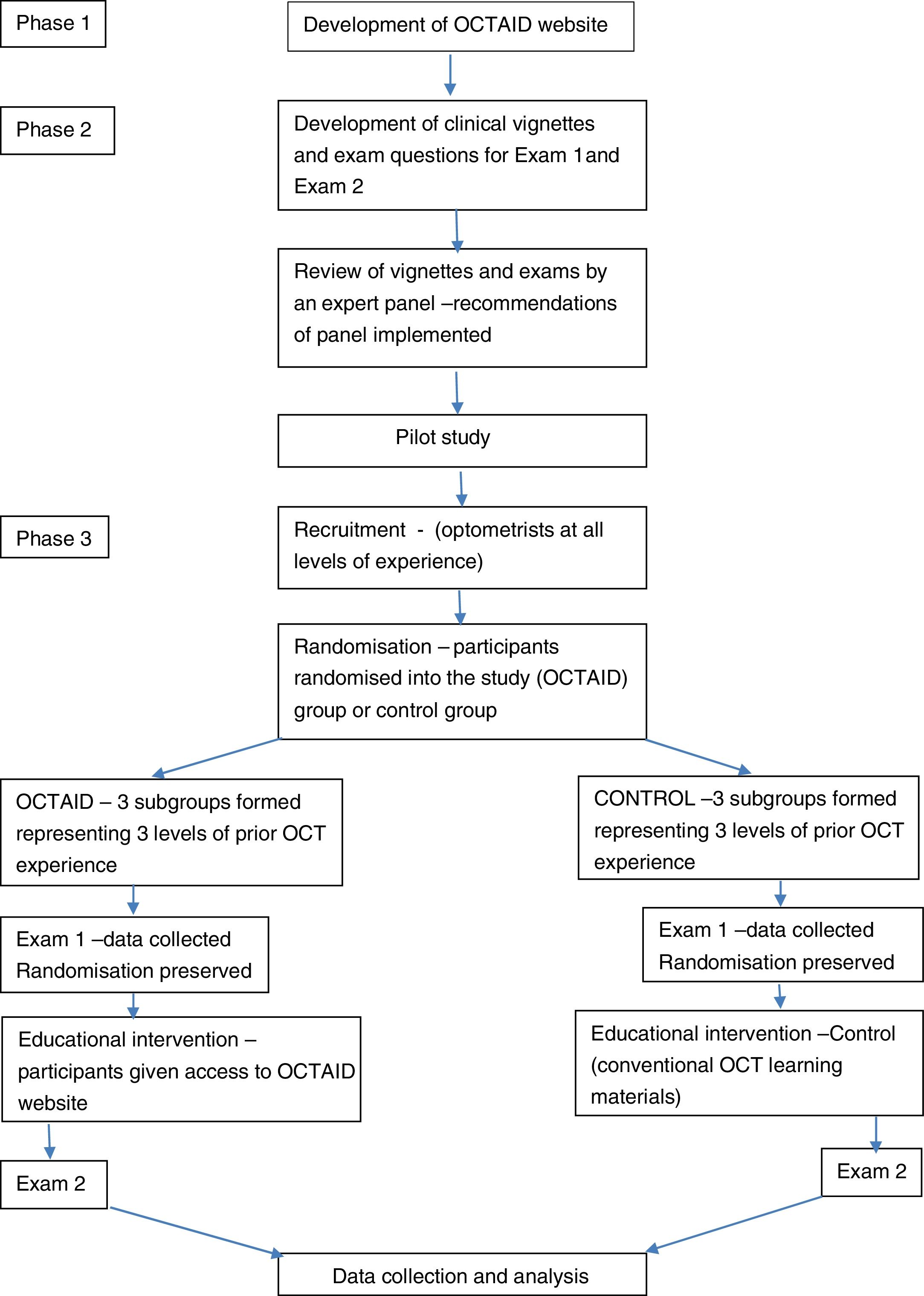
Materials and methodsAn overview of the study is presented in Fig. 1. This highlights the three phases of the research which, together with their aims, are summarised below:
- 1.
Development of an online diagnostic guide (OCTAID) with the aim of improving the diagnosis and optometric management of central retinal lesions using OCT.
- 2.
Design an online assessment in the form of two exams using the ‘Visual Recognition and Investigation of Clinical Signs’ (VRICS) format based on OCT images. The assessment uses online clinical vignettes, and questions are presented in multiple choice format. The aim of developing the exams is to provide a tool for the assessment of OCTAID in a randomised controlled trial.
- 3.
Conduct a randomised controlled trial using the online vignettes to compare the improvement in performance of two groups of optometrists, after receiving different educational interventions to aid and improve OCT diagnostic skills: the experimental group received OCTAID and the control group received a control intervention. The aim of the randomised controlled trial is to investigate the efficacy of OCTAID compared with conventional OCT resources.
The internet has become an essential part of everyday life and has also become central to the education of healthcare practitioners.18,19
For the present research, a new information resource, diagnostic algorithm and training platform for OCT interpretation was developed (OCTAID). OCTAID is an interactive website that uses branching logic and contains over 390 images.
The main diagnostic arm of the OCTAID website (Start Diagnosis) is organised with the branching logic of an algorithm and essentially invites the clinician to describe what they are seeing and identify what retinal layer is involved (“What is it and where is it?”). Novice OCT practitioners might choose this route when searching for a diagnosis, as inexperienced clinicians often adopt an algorithmic approach to diagnosis. Experienced practitioners may instantly recognise a condition (pattern recognition) but may wish to confirm this. Their starting point might then be from the alternative diagnostic arm (“I know what this is”). This section of the OCTAID site contains the same type of branching logic of an algorithm (both sections are linked). At the conclusion of this diagnostic arm the user is invited to consider an alternative diagnosis. This is particularly important in the diagnosis of ‘wet’ AMD which has several mimicking conditions for which the OCT appearances are very similar but patient management decisions are markedly different. The OCTAID site also contains sections on scanning protocols, instrument artefacts and the normal macula.
The control interventionSome educational materials for OCT data interpretation are freely and readily available online, but it was not assumed that all participants would have access to these materials or would have sufficient background knowledge of OCT to conduct an effective search for relevant resources/materials. For this reason, the control group was given access to a paper on OCT interpretation (with permission from the copyright holder). This paper provided an introduction to OCT of sufficient quality and relevance to the vignettes used in this study to enable further searches for information required to answer questions within the assessments. The publication contained images of common macular conditions and advice on their interpretation and it was designed primarily for clinical reference by interns and doctors as well as a student resource. This guide was developed as part of a Master of Science in Vision Science project by Pacific University College of Optometry students.19
Participants allocated to the control group were given the control intervention and also permitted to use whatever OCT information resources they would normally use. Participants allocated to the OCTAID (experimental) intervention were permitted to use whatever OCT resources they would normally use and additionally received access to the OCTAID website.
The expert panelAn expert panel was recruited to play an advisory role in the design of OCTAID and to act as a ‘reference standard’ in assessing practitioners’ skills by forming a consensus opinion on diagnosis and management, based on OCT scans. The panel comprised two optometrists, two consultant ophthalmologists with a special interest in medical retina conditions and a biomedical scientist with specialist knowledge of OCT. All panel members were familiar with OCT imaging and interpretation. There is a case for the use of a heterogeneous panel made up of experts with different backgrounds (within the area of interest) which reduces the risk of domination by a particular expertise.20
The exam tasksThe exam tasks were online assessments designed to evaluate OCT diagnostic skills. The first assessment took place at the beginning of the research (before participants received their interventions) and the second after the interventions. The exam tasks were not time-limited and an “open book” approach was used. The rationale for this decision is that a “closed book” timed examination would be likely to impact adversely on recruitment and it would be impossible to measure the degree of compliance to a closed book assessment in a non-invigilated exam setting.
When developing the exam tasks the research team and expert panel scrutinised the OCTAID site and the control educational intervention to ensure that exam questions were not biased to favour either intervention. Similarly, the expert panel verified that exam questions were pitched at a reasonable level of difficulty and concentrated on macular conditions which optometrists would regularly encounter in community practice.
Each exam task consisted of 8 sets of questions (3 questions in each set) presented as clinical vignettes and including OCT images, followed by a further 8 questions which tested the participant’s general OCT knowledge. Both exams used multiple choice question (MCQ) format. The software did not allow participants to return to a question once it had been answered because, in some cases, the answer to a question was revealed in subsequent questions. The first exam task, containing 32 questions, was presented before the educational intervention. The second examination, containing 32 different questions, was presented after the educational intervention. Each exam had a specific release date (separated by 3 weeks). It was not possible for all participants to start the exam tasks together but participants were prevented from proceeding with the second exam until they completed the first. Participants were encouraged to use the time interval between exams to familiarise themselves with the educational material provided (the interventions). There was no need to memorise any of the educational material because the participants had access to the materials during the exams, as they would in clinical practice. Although the exam questions were different for each exam task, they tested participants on a similar range of ocular conditions with equivalent levels of difficulty. Some questions for each OCT image tested participants' diagnostic skills (image interpretation) with the remainder testing participants’ management skills (referral decision, review period, likely treatment). Questions were structured in a stepwise fashion. The maximum score available for each exam was 32.
Recruitment and maskingParticipants were recruited by the researchers publicising the research to the optometric community primarily via a number of online optometry forums and by snowball sampling (chain referral sampling) whereby forum members were asked to forward details of the study to their optometric acquaintances. The only inclusion criterion was that all participants were required to be community optometrists with an interest in OCT. Further criteria were not necessary because the goal was to recruit optometrists with varying levels of OCT experience including those who may not have had access to OCT equipment. The study was conducted between 2nd May 2016 and 22nd July 2016 and involved community optometrists from the UK.
The study did not take account of variables such as participant age or length of time qualified because, due to the novel nature of OCT images in optometric practice in the UK at the time of the study, few if any participants would have significant prior experience of OCT. It was considered much more relevant to assess their experience with OCT than their age or time since qualification.
When participants responded to publicity about the study, they were sent a questionnaire designed to establish previous OCT experience. Participants were asked to estimate how often they assessed OCT scans, which was thought preferable to asking participants to arbitrarily rank themselves as ‘novice’, ‘intermediate’ or ‘expert’. Participants were asked to choose one of three options in a questionnaire about how many OCT scans they viewed and assessed, in any context or situation, in a typical month: less than 5; between 5 and 10; more than 10. Participants were not excluded on the basis of previous OCT experience but the analysis investigated the effect of experience.
A pragmatic approach to masking was adopted because the researcher dealing with recruitment (PG) was required to upload participant details onto the online exam host (LearnUpon) platform to assign participants to the correct group (OCTAID or control). This ensured participants were assigned to the appropriate intervention and involved registering an email address for each participant in preparation for automated invitations and reminders from LearnUpon. The researchers required contact via participants’ email throughout the study, not only to answer queries and deal with IT issues but also to keep participants engaged, focussed and motivated. Participants were not informed which study group they were assigned to and remained unaware until after completion of the first exam task, at which point they were provided with a live link to the relevant OCT training intervention (OCTAID or control). Obviously, it was not possible to avoid participants recognising the nature of the interventions they received.
All participants were informed that they would have free access to the OCTAID site after completion of both exam modules. It was hoped that this would reduce participant attrition from the control group.
The online exam host (LearnUpon) hosted two courses for this study (OCTAID and control) which were identical except for the educational intervention following completion of the first exam task. Once assigned to a course on LearnUpon (and a subgroup for more detailed analysis), participants could not be moved to another group, even in the event of unequal sized groups following withdrawals, failure to register or enrol or failure to start or finish the course. The integrity of the original process of randomisation was therefore preserved at the risk of attrition affecting the number of participants in one study group disproportionately.
UK optometrists are required to provide evidence of continuing education and training (CET) in the form of CET points from a statutory regulatory body, the General Optical Council. The interventions and vignettes were approved for CET points and points were awarded for successful completion of each of the two exams within the study.
RandomisationParticipants were given a unique identification code and divided into 3 groups depending on their prior level of OCT experience. Both the unique ID and level of OCT experience were written on a piece of paper, folded and placed in one of 3 boxes based on OCT experience. The contents of each subgroup box were further divided in half by a third party randomly choosing half of the pieces of paper. Half of each subgroup was allocated to the study (OCTAID) group, with the other half being allocated to the control group. The authors played no part in allocating participants to study groups.
Pilot studyThe study was piloted by 6 optometrists with varying degrees of OCT experience, selected on the basis of their previous OCT experience as defined by the questionnaire used in the main study. Pilot participants all recommended that the MCQ exam modules should be shortened. In response, each exam task was shortened from 40 questions in the pilot exam to 32 questions for the main study. Care was taken to ensure that the abridged assessment covered the same range of macular conditions and remained comprehensive and thorough. Pilot participants expressed no other concerns.
Statistical analysisStatistical analysis was conducted using SPSS (21) software. Categorical data were summarised as numbers and proportions. Participants’ pass/fail rate was described and groups formally compared using Chi-square tests. In the case of the second exam assessment, there were low numbers in one cell (only 3 fails in exam 2 for the OCTAID group). Because of these low numbers Fishers Exact test was the appropriate test to use for the 2 × 2 table for the second exam results and, to maintain consistency, this test was also used for comparing groups in the first exam assessment.
The main outcome variable was the improvement in exam score, calculated as the score in exam 2 minus the score in exam 1, which could be positive or negative. The improvement variable was tested for normality by inspecting the frequency distribution and carrying out the Shapiro–Wilks test in each group. The improvement in each of the two groups was compared using an unpaired t-test or Mann–Whitney U test as appropriate.
ResultsOCTAID v controlOf the 160 signed consent forms returned by potential participants, 50% (80) were randomly allocated to the OCTAID group and 50% to the control group. A total of 118 participants who returned their signed consent forms (74%) participated fully in training and completed both assessments.
Participants were randomly allocated to groups and enrolled at the outset of the study and, therefore, before the results of the first assessment were known. Fifty-three participants from the study (OCTAID) group completed the first exam with a mean score of 67.2% (SD 14.2). Sixty-five participants from the control group completed the first exam achieving a mean score of 63.7% (SD 15.4) with no statistically significant difference between group mean scores (p = 0.21, independent samples t-test).
In the second exam (post-intervention) the OCTAID group mean score was 80.6% (SD 12.3). The control group mean score was 70.9% (SD 13.1) and the difference between the group mean scores was statistically significant (p < 0.001).
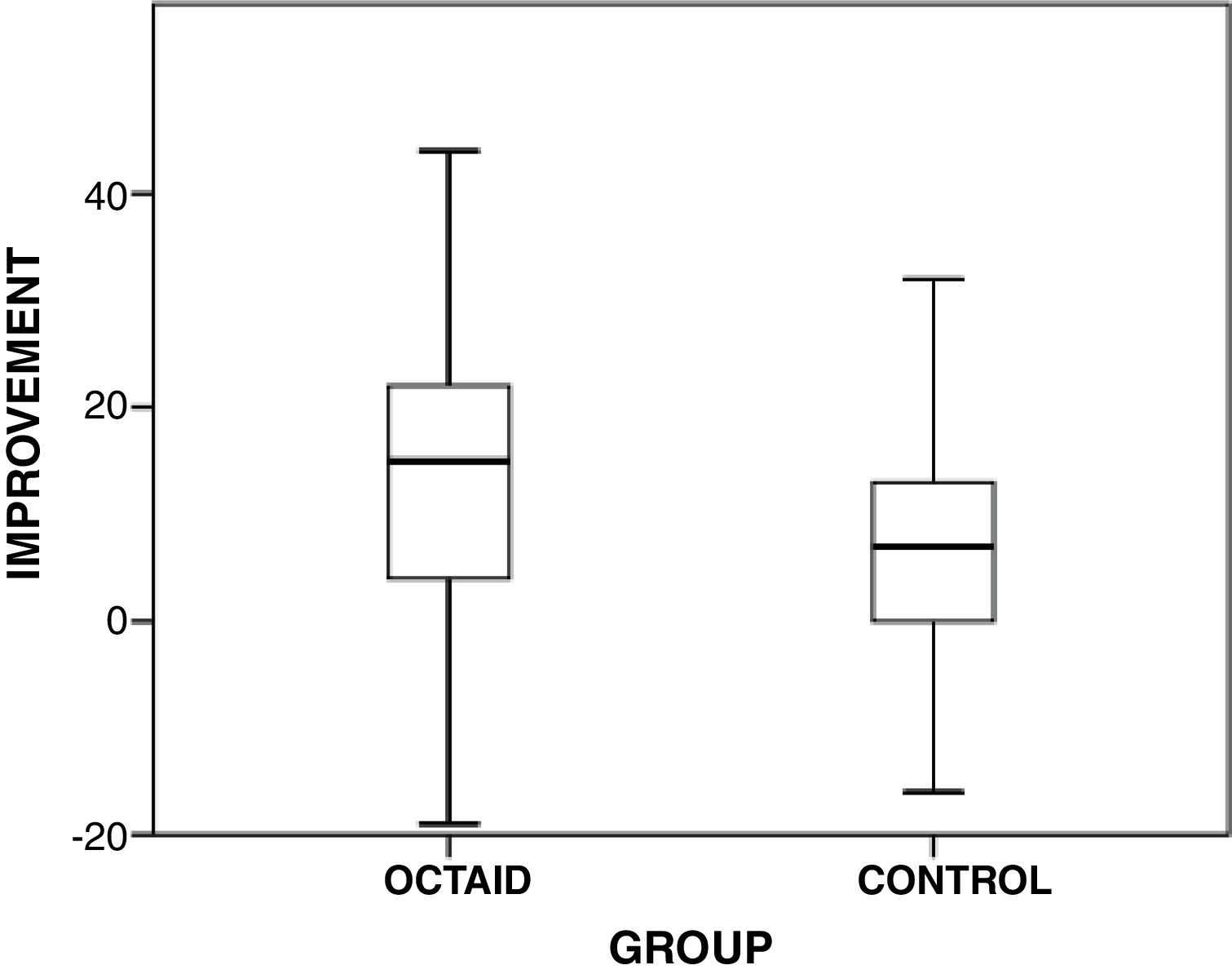
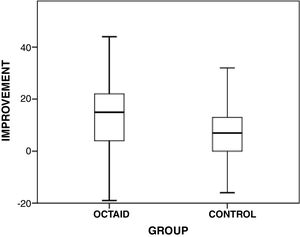
The primary outcome measure was the improvement in exam score (score in exam 2 minus the score in exam 1). The distribution of the improvement variable was tested by inspecting frequency distributions in both main groups (OCTAID and control) and carrying out the Shapiro–Wilks test, which confirmed distributions that did not differ significantly from a normal distribution (p > 0.25). The mean improvement in exam performance in the OCTAID group was 13.4% (SD 12.7). The mean improvement in exam performance in the control group was 7.2% (SD 11.8). Applying the independent samples t-test, the OCTAID group showed a significantly greater improvement in mean exam score compared with the control group (p = 0.005). The improvement in participants’ scores between exam 1 (before intervention) and exam 2 (after intervention) is illustrated in the box and whisker chart (Fig. 2).
Box and whisker chart showing score improvement (OCTAID v control).
The box represents the upper and lower quartiles so the box spans the interquartile range — the median is marked by the horizontal line inside the box. The whiskers are the two lines outside the box that extend to the highest and lowest observations, excluding outliers (there were no outliers in this data).
Participants’ OCT experience was classified as one of three levels: inexperienced or ‘novice’, intermediate and experienced. Participants in the intermediate subgroups were small in number (6 in the control group and 3 in the OCTAID group) therefore their exam scores were not subjected to detailed analysis.
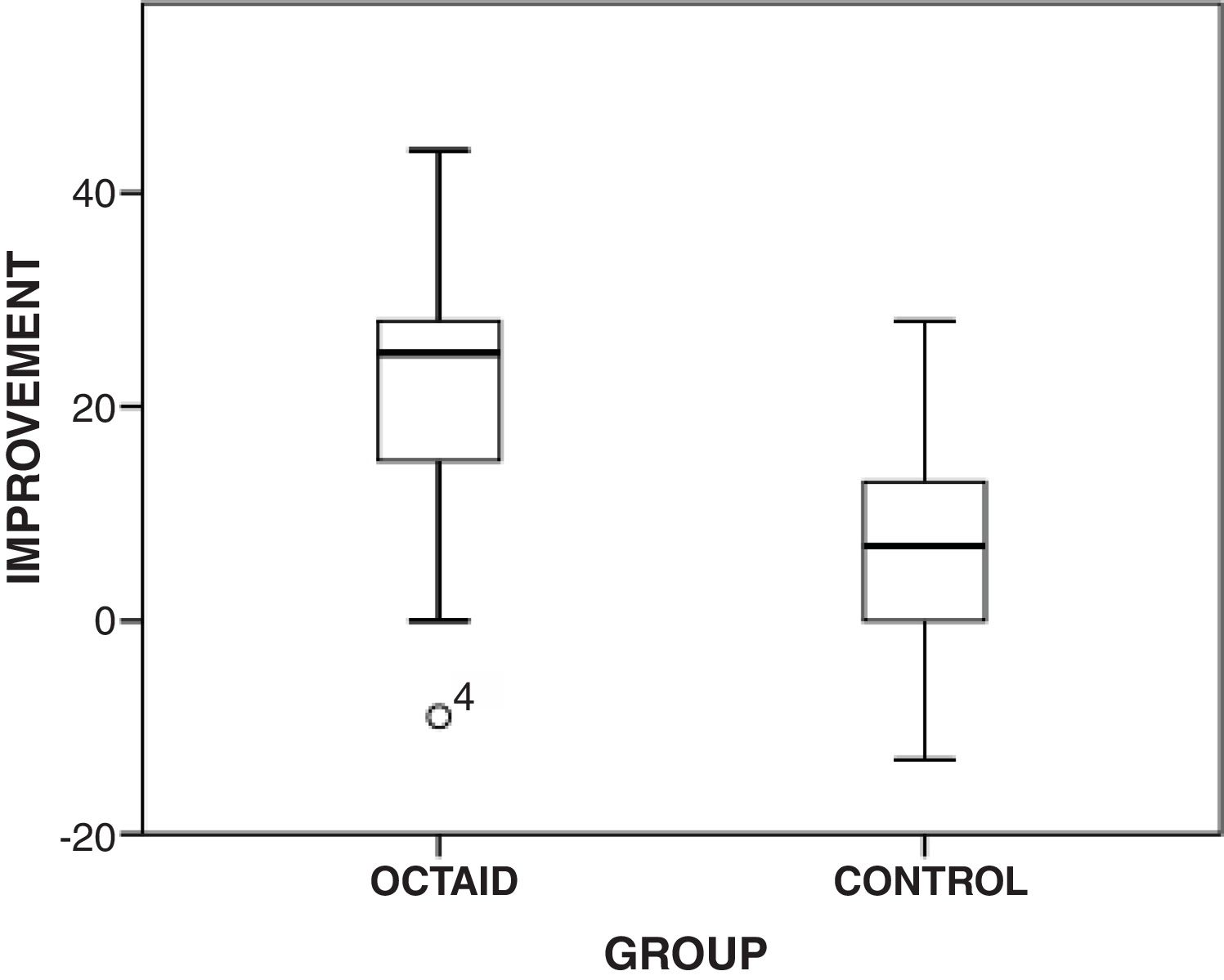
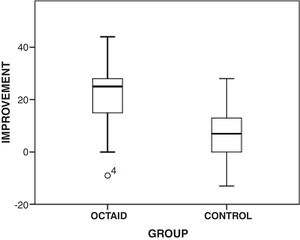
The ‘novice’ subgroups (n = 21 for the OCTAID group, n = 19 for the control group) performed similarly in the first assessment with a mean score of 57.7% (SD 13.9) for the OCTAID subgroup and 58.0% (SD 16.7) for the control subgroup with no significant difference between means (p = 0.95, t-test).
The mean exam 2 score for the OCTAID novice subgroup was 77.8% (SD 15.4) compared with 65.2% (SD 15.9) for the control novice subgroup. The OCTAID novice subgroup improved their mean exam score by 20.1% compared with a mean improvement of 7.2% in the control novice subgroup. The independent samples t-test demonstrated statistically significantly better outcomes in terms of mean score improvement in the OCTAID novice subgroup (p = 0.001). The primary outcome measure of exam score improvement for each group is summarised in the box and whisker chart (Fig. 3).
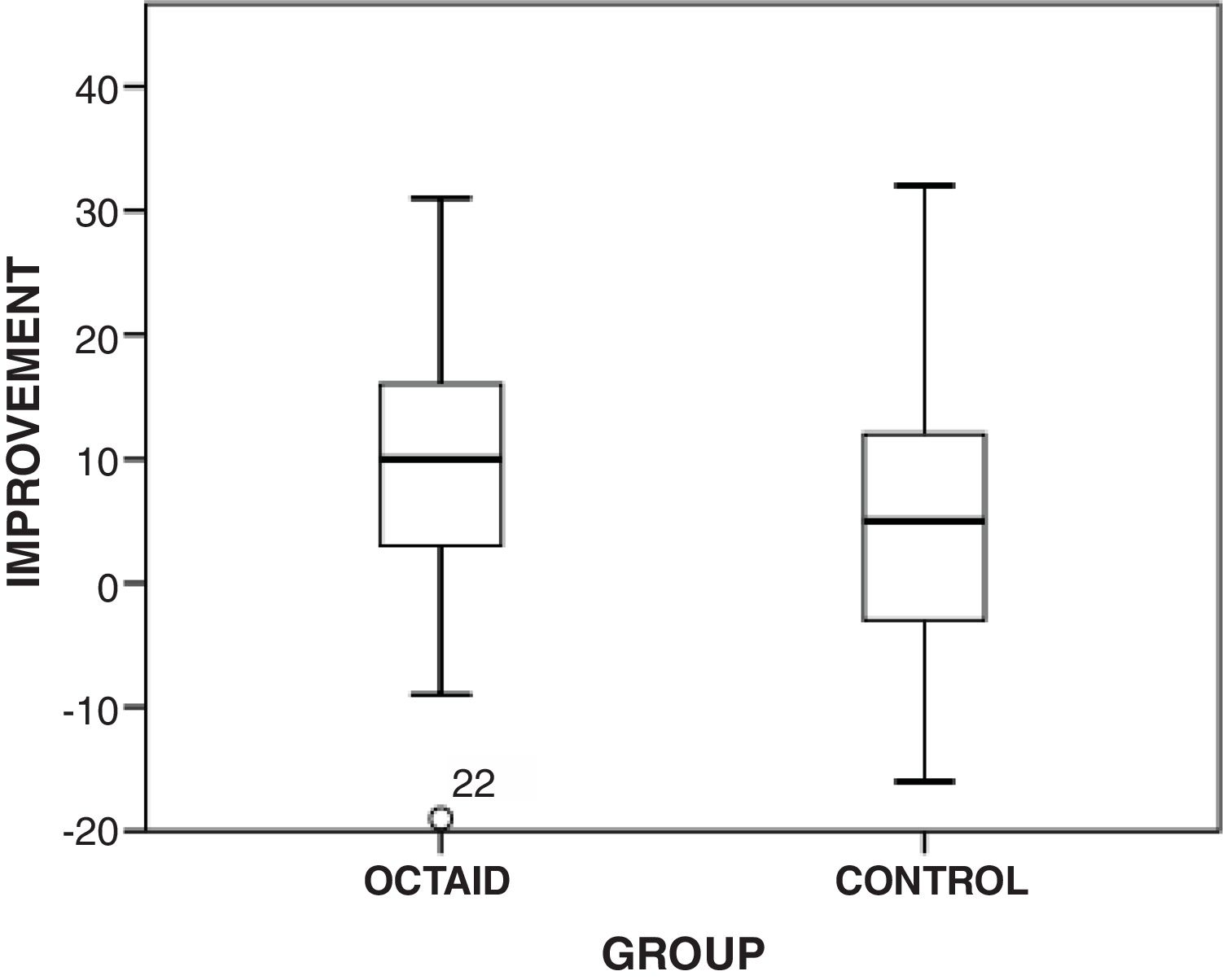
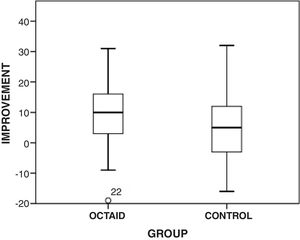
As expected, the experienced subgroups performed best in both exams with the OCTAID subgroup (n = 29) achieving a mean score of 73.5% (SD 11.0) in exam 1 compared with 68.7% (SD 13.3) in the control subgroup (n = 40) with no significant difference between mean scores (p = 0.12).
The mean exam 2 score for the OCTAID experienced subgroup was 82.6% (SD 9.9) vs 74.5% (SD 11.2) for the control experienced subgroup. Although the experienced OCTAID subgroup’s mean exam score improved by 9.1% compared with 5.8% in the control subgroup, there was no statistically significant difference in mean improvement (p = 0.25).
The primary outcome measure of score improvement is summarised in the box and whisker chart (Fig. 4).
Secondary outcome measuresSetting a pass markThe exams received accreditation (with a pass mark of 60%) from the UK regulatory body, (the General Optical Council, GOC) that governs optometric Continuing Education and Training (CET). Using this 60% pass mark, the difference in pass rate between the study and control groups was used as a secondary outcome measure.
There was no statistically significant difference between the OCTAID (Pass rate = 71.7%, 38/53) and control groups (Pass rate = 61.5%, 40/65) in the first exam (Fisher’s two-sided exact test, p = 0.33).
There was a statistically significant difference in pass rate between the OCTAID (Pass rate = 94.3%, 50/53) and control group (Pass rate = 75.4%, 49/65) in the second exam which followed the educational intervention (p = 0.006).
Chi square analysis of the pass rate showed no significant difference between the OCTAID (Pass rate = 47.6%, 10/21) and control (Pass rate = 47.4%, 9/19) novice subgroups in exam 1 (Fisher’s two-sided exact test, p = 1.00). However, a statistically significant difference was demonstrated between groups in their pass rate in exam 2, with the OCTAID novice subgroup (Pass rate = 90.5%, 19/21) outperforming the control novice subgroup (Pass rate = 47.4%, 9/19) (p = 0.005).
No significant difference between the OCTAID (Pass rate = 86.2%, 25/29) and control (Pass rate 77.5%, 31/40) experienced subgroups was demonstrated from the Chi square analysis of the pass rate in exam 1 (p = 0.54).
Similarly, Chi square analysis of the pass/fail results in exam 2 showed no significant difference between the two experienced subgroups in terms of pass rate (p = 0.39).
Monitoring use of the OCTAID websiteThe use of the OCTAID site was monitored throughout the study using Google Analytics software. The number of visitors to the site equalled the number in the OCTAID study group so it was reasonable to assume that these visitors to the site represented this group.
Measuring participants’ use of educational interventions and time taken to complete the exam tasksParticipants were asked (using short electronic questionnaires linked to the online study modules) how long it took them to complete each exam task and how long they spent studying the OCT educational tools provided for the study.
Participants from both the OCTAID and control groups were asked how much time they spent completing exam 1 and all 118 participants answered this question. Based on feedback from the participants in the pilot study, data were collapsed into two categories, namely <90 min (40 participants from the OCTAID group and 54 from the control group) and >90 min (13 participants from the OCTAID group and 11 from the control group)
There was no statistically significant difference between the OCTAID and control groups in terms of time spent completing exam 1 (Fisher’s exact two-sided, p = 0.36).
Participants were also asked how long they spent completing exam 2. Eighty participants provided a response to this question (40 from each group). Seventeen participants from the OCTAID group and 27 from the control group took less than 90 min to complete the second exam. Twenty-three participants from the OCTAID group and 13 from the control group took more than 90 min to complete the second exam.
In general, the OCTAID group spent longer completing the second exam task than the control group and this difference in proportions just reached statistical significance (p = 0.04).
Participants in both groups were asked how much time they had spent studying the OCT resources (OCTAID or control). Four ordinal time categories were created for participants to choose from in the questionnaire, which was completed immediately after the second exam module. These categories were: less than 2 h (25 from the OCTAID group and 37 from the control group), 2–4 h (8 from the OCTAID group and 3 from the control group), 4–6 h (5 from the OCTAID group and 0 from the control group), and more than 6 h (2 from the OCTAID group and 0 from the control group).
Participants in the OCTAID group spent more time reviewing OCTAID than the control group spent reviewing the control educational resource. This time difference in the two groups was statistically significant (p = 0.01).
DiscussionThis study indicates that use of OCTAID is associated with statistically significant improvements in vignette scores when compared with the group using conventional OCT resources. This improvement is greatest and statistically significant in a subgroup of less experienced OCT users but the improvement did not reach significance in a subgroup of more experienced OCT users.
It is difficult to determine which aspect of OCTAID’s design (e.g., its website delivery or its illustrated explanatory algorithm) resulted in improved vignette task performance. Accessing clinical information via the web may be more intuitive to some optometrists and less intuitive to others. However, there is a situational relevance to using an online training tool employing digital OCT images to improve skills at interpreting the digital images that OCT provides.
As acknowledged in another study with an exam setting based on OCT scans and clinical vignettes, results may not be fully representative of a participant’s diagnostic performance in a genuine clinical setting.21
This study was subject to some limitations. Double blinding (an experimental procedure in which neither the participants nor the researchers know which participants are in the experimental and control groups during the course of the experiment) was not possible and a more pragmatic approach was adopted. However, the integrity of the original process of randomisation was preserved. Also, the exam modules were not timed and it is possible that participants who spent more time in researching the answers to questions achieved a higher result. Whilst it could be argued that this may have been a factor in improving the exam score of the OCTAID group, participants from both groups were allowed to take as much time as they wished to complete the exam task. Participants using the OCTAID site may have felt more confident about finding answers to vignette questions (perhaps because of the ease of navigation of the OCTAID resource or a strongly held belief that the OCTAID site would provide an answer) and therefore may have spent more time exploring the OCTAID resource during the exam task. The OCTAID site may also have had novelty value and participants’ curiosity may have given them the incentive to explore the site for solutions to the vignette task.
However, these explanations are speculative and the reason why the OCTAID group spent more time studying the OCTAID intervention than the control group spent on the control intervention cannot be determined from the data in the randomised controlled trial.
When researching the answers to questions in the exam modules, participants in both the OCTAID and control groups were permitted to use whatever resources they would normally refer to when making a diagnostic or patient management decision based on an OCT scan in their everyday practice. In addition to this the OCTAID group were provided with a link to the OCTAID website and the control group were provided with a link to a conventional OCT resource. Whilst it could be argued that the control intervention provided a less comprehensive knowledge of OCT than the OCTAID site, the study was testing the efficacy of the OCTAID site compared with conventional OCT resources, of which the control intervention is a typical example. We could not however be certain that the OCTAID and control groups were accessing resources of equivalent content. It is also possible that some participants in the OCTAID group had access to the control intervention through their own online searches.
There is an established principle in medicine that diagnostic tests should only be performed where they are clinically indicated because the overuse and indiscriminate use of diagnostic tests in any field of medicine increases false positive referrals.22 Educational tools such as OCTAID do not adequately address this important issue although the improvement in diagnosis and management skills after OCTAID is an encouraging finding.
For a small number of participants (n = 6 in the OCTAID group and n = 15 in the control group), scores in the second exam were lower than in the first exam (by an average of 7.2% in the OCTAID group and 7.8% in the control group). One explanation for this could be that, although considerable efforts were made to design both exams to have the same level of difficulty, it is inevitable that some participants would find one exam less difficult than the other.
The OCTAID group as a whole performed better (in terms of exam score improvement) than the control group but took longer to complete the second exam task than the control group in what was an ‘open book’ exam. Further research on factors influencing diagnostic accuracy of optometrists using OCT imaging technology may help to confirm, complement or challenge our findings.
Extensive literature searches did not identify any similar studies for comparison and whilst it is hoped that this study has made a contribution to knowledge, it would be helpful if it could be shown how the data from this study might compare with other similar studies.
In recent times community optometrists have faced unprecedented challenges, not only in how they are providing care to patients but also in how to continue to educate the next generation of optometrists. The current COVID-19 pandemic is affecting optometric education and practice in ways that may disrupt the training of future eye care professionals. It seems likely that long waits for hospital eye service appointments will increase the use of community optometrists with OCTs for monitoring macular conditions. It is more important than ever to ensure that the optometry community has access to high-quality educational materials to ensure trainee preparedness for clinical challenges. Large-scale, global efforts to utilise technology in support of remote learning, distance education and online learning during the COVID-19 pandemic are emerging and evolving quickly. The efficacy demonstrated here for an online training tool, OCTAID, is an encouraging finding in these times when online training has clear advantages.
ConclusionsThe data presented in this study indicate benefits from a novel diagnostic tool, OCTAID, in improving the ability to interpret OCT central retinal scans for diagnosis and patient management
The potential exists for OCTAID to be used as an online training tool for optometrists and greater improvements in diagnostic accuracy may be achieved through the further development of the OCTAID site following feedback and the submission of archive images from multiple users.
It is planned to develop OCTAID to become a learner-centred model of OCT education, thus providing an opportunity for optometrists to take responsibility for their own learning within a unique professional community. Practitioners will be invited to contribute anonymised OCT images to keep OCTAID as a continuously updated resource and the goal is to keep the site freely available to eyecare practitioners. With standard online translation tools, language should be no barrier, facilitating a truly international community.
Conflicts of interestAccess to OCTAID is provided free of charge to practitioners. OCTAID was developed by the authors without sponsorship from any commercial interests.
We thank the participants who not only gave their time to participate but also gave valuable feedback.