To evaluate the agreement of dry, and cycloplegic autorefraction and wavefront-based refraction with subjective refraction.
Method83 subjects aged 19–57 years were included in this cross-sectional study. Refractive status was determined using four methods including subjective refraction, wavefront-based refraction, dry and cycloplegic autorefraction. Refractive data were recorded as sphere, cylinder and spherical equivalent (SE). Power vector components were used to compare the astigmatism obtained using the different methods of refraction.
ResultsThe more negative spherical, cylindrical and SE components were obtained using dry autorefraction, wavefront-based refraction and dry autorefraction, respectively. The less negative spherical, cylindrical and SE components were obtained using cycloplegic autorefraction, subjective refraction and cycloplegic autorefraction, respectively. Considering the spherical component, there was a statistically significant hyperopic shift (0.12 ± 0.29 D, p = 0.001) with cycloplegic autorefraction and a significant myopic shift (−0.17 ± 0.32 D, p < 0.001) with dry autorefraction compared to subjective refraction, while the difference between wavefront-based and subjective refraction was not significant statistically (p = 0.145). The calculated cylindrical component using subjective refraction showed statistically significant difference with dry auto-refraction (p < 0.001), cycloplegic auto-refraction (p = 0.041) and wavefront refraction (p < 0.001). The highest correlation with subjective refraction in sphere, cylinder and SE was observed for cycloplegic auto-refraction (rs = 0.967), dry auto-refraction (rs = 0.983) and cycloplegic auto-refraction (rs = 0.982), respectively.
ConclusionsAs subjective refraction is gold standard in our study, sphere in cycloplegic auto-refraction and astigmatism in dry auto-refraction showed better agreement and correlation.
Various techniques have been developed to assess the refractive status of the eye. Traditionally, subjective manifest refraction has been known as a gold standard for refraction and spectacle prescription, although it is a time-consuming procedure.1 Objective autorefracometers and, more recently, wavefront-based autorefractometers have achieved their clinical popularity because of their acceptable repeatability, accuracy, time-saving capability and ease of use.2–6 The introduction of automated refraction in the 1970s has created a promising revolution in eye examination.7 Autorefraction is considered as a clinically valuable starting point for subjective refraction.8–10 Over the past few years, the wavefront analysis systems was considered as a turning point for clinical optics because these systems provide a new way to examine the refractive errors in details, including lower and higher orders aberrations.11 The difference between classical refraction and wavefront sensing is analogous to the difference between keratometry and corneal topography. Subjective refraction and autorefraction both have a limited ability to separate between low and higher orders aberrations such as coma, trefoil and spherical aberration that can adversely affect the quality of retinal images and ultimately the visual quality.12 Wavefront sensing devices supply both types of aberrations, lower (spherical defocus and astigmatism) and higher orders aberrations.The wavefront-based refraction is based on fitting a reference (ideal) wavefront on the actual wavefront.13
The subjective refraction is considered as a standard procedure in assessing refractive errors to consider the need to modify the present correction. Sometimes, subjective refraction is not possible, as in young children or uncooperative subjects, and the findings of other techniques must be used. Therefore, the present study was designed to evaluate the agreement of the results obtained using wavefront-based refraction, dry and cycloplegic autorefraction and subjective refraction in adults.
MethodsThis cross-sectional study included 83 eyes of 83 subjects aged 19–57 years who met the inclusion criteria. All procedures of this study followed the principles of the Declaration of Helsinki, and an informed consent was obtained from each subject after explaining the goals of the study. The study protocol was approved by the Ethics Committee of Shiraz University of Medical Sciences. (Code No.: 16930) Exclusion criteria were corrected distance visual acuity of less than 20/25, history of corneal refractive surgery, previous eye trauma, corneal scar and corneal irregularity secondary to ectasia or dry eye, cataract and history of long-term contact lens wearing. Refractive status was determined for each subject using four methods, including subjective refraction, wavefront-based refraction, and dry and cycloplegic autorefraction. All techniques were performed by the same experienced and qualified optometrist to avoid any bias during a single visit. Subjective refraction was done using maximum plus acceptance for all subjects. This process was applied by determination of best vision sphere and cylinder (magnitude and axis) using the Jackson cross-cylinder technique.14 Owing to sphere power adjustment, variations in cylinder power were partly compensated; however, the entire compensations were subjectively controlled as well. For further measures, the cylinder highest power- that requested to be enhanced—was determined. After monocular subjective refraction, binocular balance was applied by alternate occlusion. The alternate occlusion method was performed using a handheld cover paddle. Both eyes were fogged with +1.00 D at the end of monocular subjective refraction and individuals were told to look at an isolated line of Snellen chart (6/9). Consequently, individual was asked to compare vision clarity between the right and left eyes while each eye was occluded for about half a second. If the individual confirmed a clearer vision in one eye, +0.25 D was added to the eye with clearer vision and alternate occlusion was repeated until equality was approached. The endpoint was the equal clarity in both eyes. Then, the ultimate spherical power was defined as the highest plus value or the lowest minus value that provided the best visual acuity. Three consecutive predicted phoropter refractions (PPR), were performed using the Zywave aberrometer (Bausch & Lomb, Rochester, NY). PPR is estimated using a second-order only Zernike model to fit the higher-order wavefront data for a nominal pupil diameter of 3.5 mm or in a specific exam pupil diameter. The Zywave aberrometer is a Hartmann-Shack wavefront sensor using wavelength of 785 nm. The accuracy of this device in measuring aberrations have been reported in a previous study.15 The measurements were immediately perfomed after a blink to minimize disruption of the tear film. Fogging of the accommodative target was turned off during measurements with this device. A 6-mm optical zone was chosen for wavefront analysis. Dry (noncycloplegic) autorefraction was done using an autorefractometer (KR-800; Topcon, Tokyo, Japan) by automatically averaging the three measurements taken at the central 3-mm of the entrance pupil. Cycloplegic effect was obtained using cyclopentolate hydrochloride 1%. Three drops of this agent were administered with a time interval of five minutes. Thirty minutes after the third drop, autorefraction was repeated under cycloplegic conditions. Refractive data were recorded as sphere, negative cylinder, and cylinder axis. The astigmatic difference between the four methods was determined using the vector components of refraction. For this purpose, the conventional refraction was transformed to Jackson crossed cylinder format to calculate M, J0, and J45 from the refractive data (S: sphere, C: cylinder, and α: cylinder axis) as the following:
To compute the astigmatic difference between subjective refraction and the other three methods, the difference in J0 and J45 was calculated separately. Finally, the final values obtained of power vector components were transformed into the conventional cylinder using the following formula for a better understanding of the outcomes:
All measurements were carried out between 4 pm and 8 pm. Cycloplegic autorefraction was always performed last. Selection of the other methods for each subject (subjective refraction, wavefront-based refraction and dry autorefraction) was done randomly.
Refractive data was collected from both the right and left eyes of each subject, however, it is extremely likely that separate eyes of an individual would not reflect distinct samples and that there would be a significant association between refractive error components of the right and left eye,16 and between higher orders aberrations of the right and left eye.17 Thus, the right eye refractive data were recorded for the analysis. Data were analyzed using the SPSS.21 software (SPSS Inc, Chicago, Illinois, USA). Normality of the data was assessed using the Kolmogorov–Smirnov test, which did not show a normal distribution for quantitative data. The non-parametric equivalent of repeated measures analysis of variance (Friedman test) was used to compare the mean sphere, cylinder and spherical equivalent (SE) obtained with the different methods and the Bonferroni adjustment applied for pairwise comparisons. Correlation of objective refraction measures with subjective refraction as the reference standard was assessed using the Pearson correlation test. Bland-Altman plots18 and intraclass correlation coefficients (ICC) were used to assess the agreement of subjective refraction with the other methods. ICC values of 0−0.2, 0.3−0.4, 0.5−0.6, 0.7−0.8 and more than 0.8 were considered indicators of poor, fair, moderate, strong and near perfect agreements, respectively.19 The limits of agreement (LoA) were determined as the mean difference±1.96SD of the mean differences. In all tests, p-values less than 0.05 were considered significant.
ResultsOf the 83 subjects studied, 27 (32.5%) were males and 56 (67.5%) females. The mean age was 28.27 ± 6.87 years, ranging from 19 to 57 years.
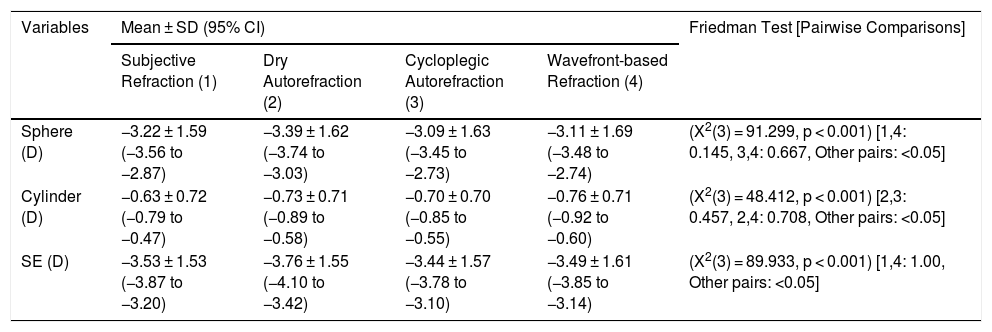
Table 1 summarizes the sphere, cylinder and spherical equivalent outcomes obtained using the different methods evaluated.
Mean and standard deviation of sphere, cylinder and spherical equivalent (SE) obtained using different refraction techniques. (n = 83 eyes).
| Variables | Mean ± SD (95% CI) | Friedman Test [Pairwise Comparisons] | |||
|---|---|---|---|---|---|
| Subjective Refraction (1) | Dry Autorefraction (2) | Cycloplegic Autorefraction (3) | Wavefront-based Refraction (4) | ||
| Sphere (D) | −3.22 ± 1.59 (−3.56 to −2.87) | −3.39 ± 1.62 (−3.74 to −3.03) | −3.09 ± 1.63 (−3.45 to −2.73) | −3.11 ± 1.69 (−3.48 to −2.74) | (X2(3) = 91.299, p < 0.001) [1,4: 0.145, 3,4: 0.667, Other pairs: <0.05] |
| Cylinder (D) | −0.63 ± 0.72 (−0.79 to −0.47) | −0.73 ± 0.71 (−0.89 to −0.58) | −0.70 ± 0.70 (−0.85 to −0.55) | −0.76 ± 0.71 (−0.92 to −0.60) | (X2(3) = 48.412, p < 0.001) [2,3: 0.457, 2,4: 0.708, Other pairs: <0.05] |
| SE (D) | −3.53 ± 1.53 (−3.87 to −3.20) | −3.76 ± 1.55 (−4.10 to −3.42) | −3.44 ± 1.57 (−3.78 to −3.10) | −3.49 ± 1.61 (−3.85 to −3.14) | (X2(3) = 89.933, p < 0.001) [1,4: 1.00, Other pairs: <0.05] |
The highest negative spherical, cylindrical and SE components were obtained using dry autorefraction, wavefront-based refraction and dry autorefraction, respectively. The lowest negative spherical, cylindrical and SE components were obtained using cycloplegic autorefraction, subjective refraction and cycloplegic autorefraction, respectively. Comparison of the repeated refractions using different techniques showed statistically significant difference for all components using Friedman’s test. The Dunn-Bonferroni post hoc test was used for the pairwise comparisons. The results are given in Table 1.
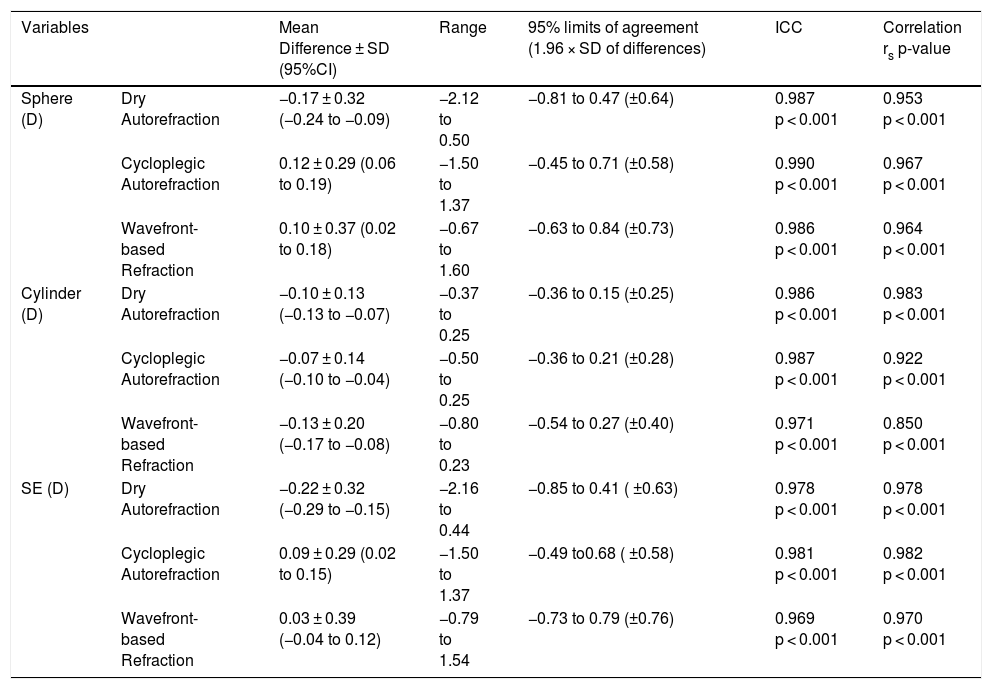
The mean difference and correlation of the refractive components obtained using different techniques in comparison with subjective refraction as the standard reference is shown in Table 2.
Mean difference, 95% limits of agreement and correlation of the refractive components with different methods compared to subjective refraction. (n = 83 eyes).
| Variables | Mean Difference ± SD (95%CI) | Range | 95% limits of agreement (1.96 × SD of differences) | ICC | Correlation rs p-value | |
|---|---|---|---|---|---|---|
| Sphere (D) | Dry Autorefraction | −0.17 ± 0.32 (−0.24 to −0.09) | −2.12 to 0.50 | −0.81 to 0.47 (±0.64) | 0.987 p < 0.001 | 0.953 p < 0.001 |
| Cycloplegic Autorefraction | 0.12 ± 0.29 (0.06 to 0.19) | −1.50 to 1.37 | −0.45 to 0.71 (±0.58) | 0.990 p < 0.001 | 0.967 p < 0.001 | |
| Wavefront-based Refraction | 0.10 ± 0.37 (0.02 to 0.18) | −0.67 to 1.60 | −0.63 to 0.84 (±0.73) | 0.986 p < 0.001 | 0.964 p < 0.001 | |
| Cylinder (D) | Dry Autorefraction | −0.10 ± 0.13 (−0.13 to −0.07) | −0.37 to 0.25 | −0.36 to 0.15 (±0.25) | 0.986 p < 0.001 | 0.983 p < 0.001 |
| Cycloplegic Autorefraction | −0.07 ± 0.14 (−0.10 to −0.04) | −0.50 to 0.25 | −0.36 to 0.21 (±0.28) | 0.987 p < 0.001 | 0.922 p < 0.001 | |
| Wavefront-based Refraction | −0.13 ± 0.20 (−0.17 to −0.08) | −0.80 to 0.23 | −0.54 to 0.27 (±0.40) | 0.971 p < 0.001 | 0.850 p < 0.001 | |
| SE (D) | Dry Autorefraction | −0.22 ± 0.32 (−0.29 to −0.15) | −2.16 to 0.44 | −0.85 to 0.41 ( ±0.63) | 0.978 p < 0.001 | 0.978 p < 0.001 |
| Cycloplegic Autorefraction | 0.09 ± 0.29 (0.02 to 0.15) | −1.50 to 1.37 | −0.49 to0.68 ( ±0.58) | 0.981 p < 0.001 | 0.982 p < 0.001 | |
| Wavefront-based Refraction | 0.03 ± 0.39 (−0.04 to 0.12) | −0.79 to 1.54 | −0.73 to 0.79 (±0.76) | 0.969 p < 0.001 | 0.970 p < 0.001 | |
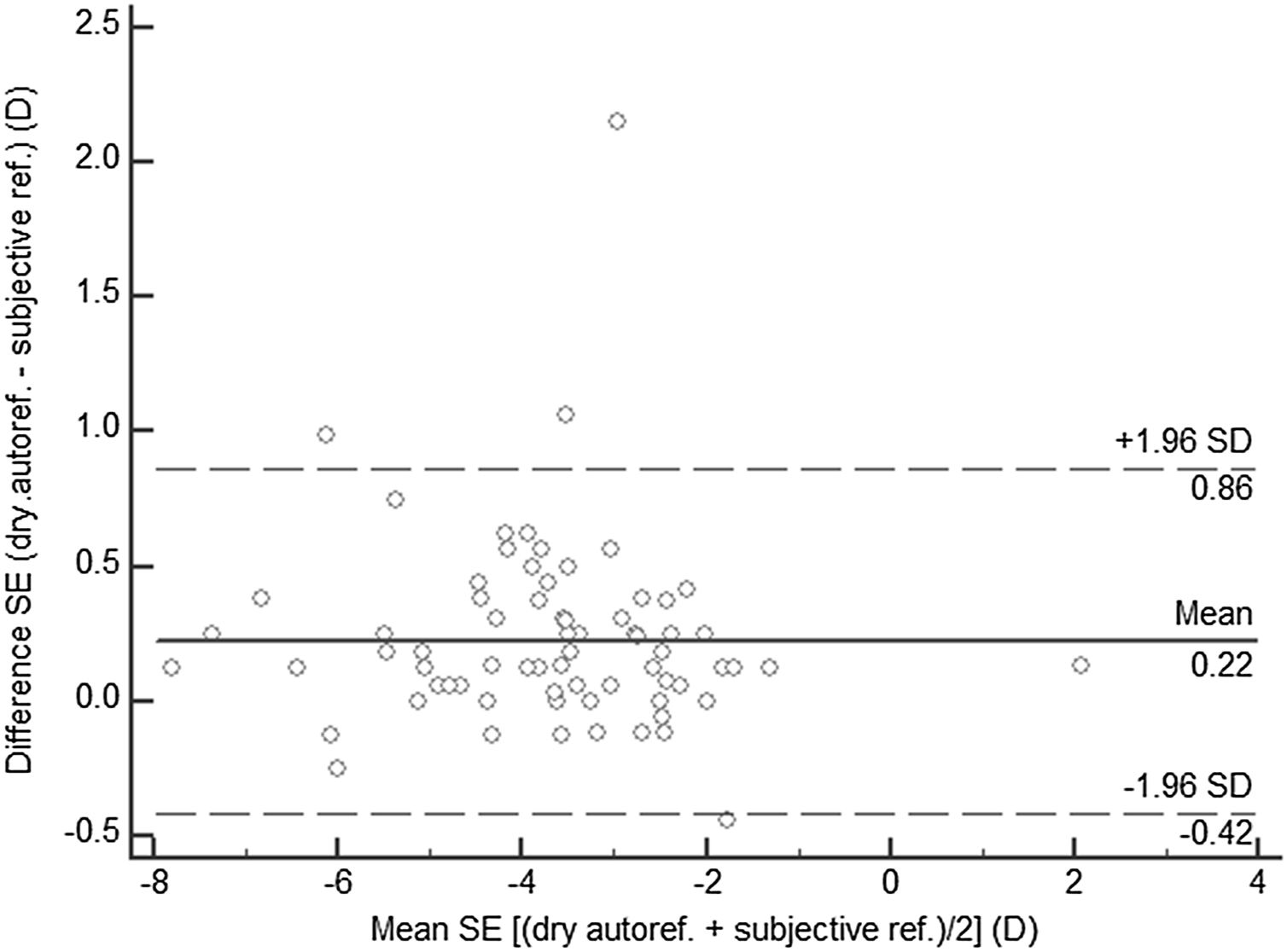
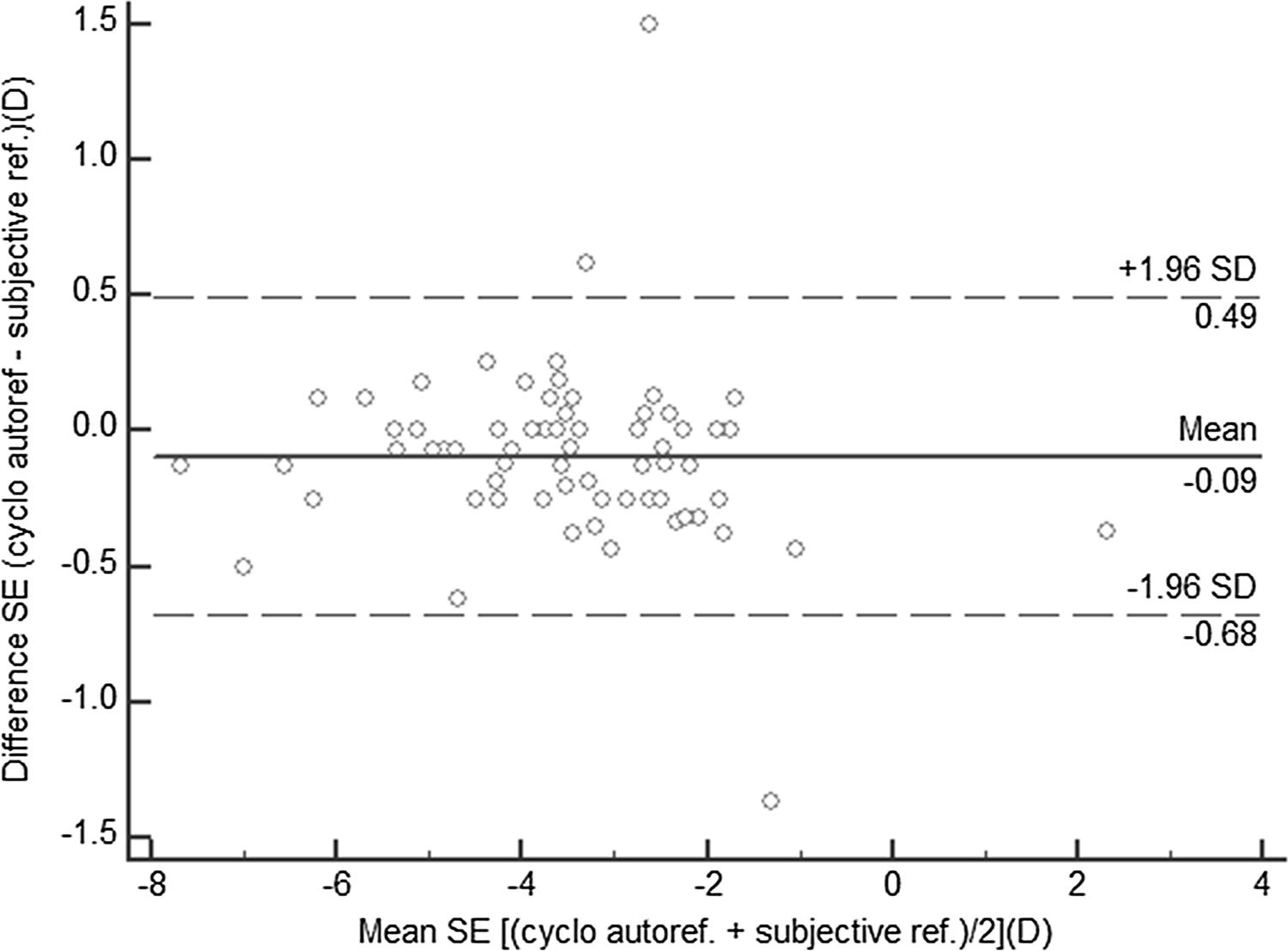
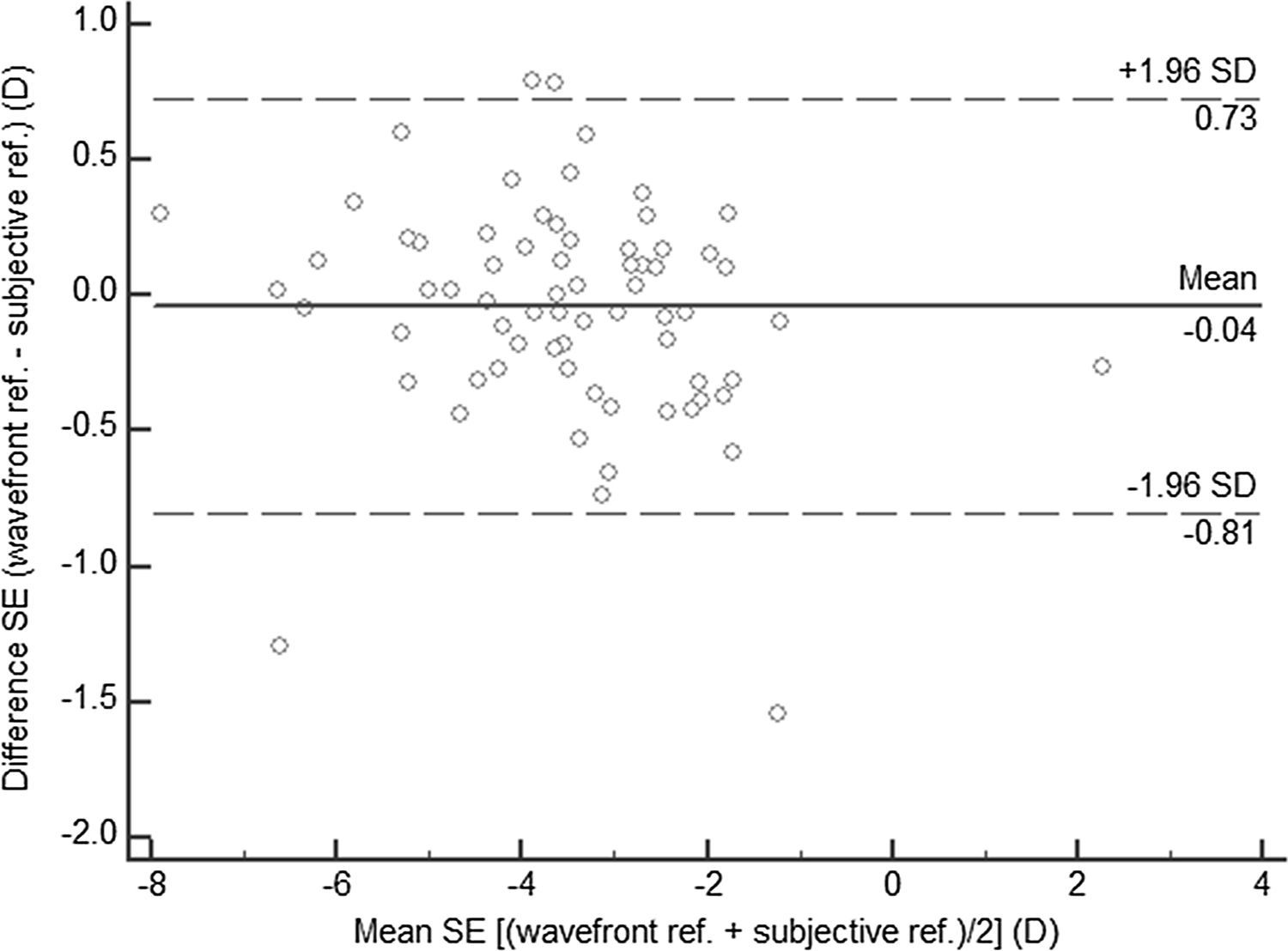
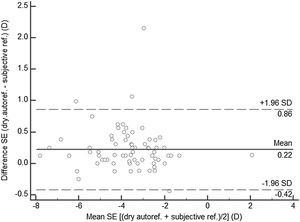
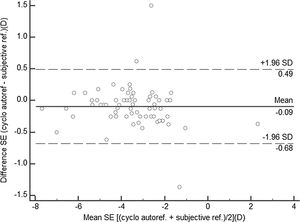
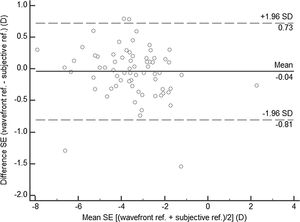
Considering the spherical component, there was a statistically significant hyperopic shift (0.12 ± 0.29 D, p = 0.001) with cycloplegic autorefraction compared to subjective refraction, and a significant myopic shift (−0.17 ± 0.32 D, p < 0.001) with dry autorefraction, while the difference between wavefront-based and subjective refraction was not significant statistically (p = 0.145). The calculated cylindrical component using subjective refraction showed statistically significant differences with dry autorefraction (p < 0.001), cycloplegic autorefraction (p = 0.041) and wavefront-based refraction (p < 0.001). As Table 2 shows, the lowest mean difference with subjective refraction in the obtained spherical and cylindrical components were found for wavefront-based refraction and cycloplegic autorefraction; however, the highest agreement was seen between cycloplegic and dry autorefraction, with narrower agreement bands (±0.58 and ±0.25 D) compared to the other methods. Considering the spherical equivalent, the lowest mean difference of SE (0.03 ± 0.39) and the highest agreement (±0.52) with subjective refraction were related to wavefront-based refraction and cycloplegic autorefraction, respectively. This good agreement was confirmed after obtaining higher values of ICC of cycloplegic refraction. Also, there was statistically significant correlation for all three refractive components (sphere, cylinder and SE) between all techniques with subjective refraction. The highest correlation with subjective refraction in sphere, cylinder and SE was observed for cycloplegic autorefraction (rs = 0.967), dry autorefraction (rs = 0.983) and cycloplegic autorefraction (rs = 0.982), respectively. According to the high and statistically significant correlation between the refractive components obtained using various techniques with subjective refraction, the Bland-Altman (1986) plot is a suitable method for analysis and comparison in situations in which different techniques measure an identical parameter. In these plots, the mean difference for SE between the two techniques is shown as a function of the mean SE of the two techniques. In each plot, the mean difference between each method with subjective refraction was marked with a horizontal solid line and the 95% limits of agreement with horizontal dashed lines. (Fig. 1, 2 and 3–3)
Agreement rate of SE obtained with subjective refraction and dry autorefraction (n = 83 eyes). The mean difference is shown by the solid horizontal line, while the 95% limits of agreement, zero mean difference and the regression line are indicated by dashed horizontal and oblique lines, respectively.
Agreement rate of SE obtained with subjective refraction and cycloplegic autorefraction (n = 83 eyes). The mean difference is shown by the solid horizontal line, while the 95% limits of agreement, zero mean difference and the regression line are indicated by dashed horizontal and oblique lines, respectively.
Agreement rate of SE obtained with subjective refraction and wavefront-based refraction (n = 83 eyes). The mean difference is shown by the solid horizontal line, while the 95% limits of agreement, zero mean difference and the regression line are indicated by dashed horizontal and oblique lines, respectively.
In all plots, more than 95% of the differences between the SE determined with each technique and subjective refraction were placed in the range ±2SD of the mean difference in SE with the two methods. The lowest agreement band or the highest agreement with subjective refraction was seen for cycloplegic autorefraction. Also, the highest percentage of zero mean difference (15.7%) was found when subjective refraction and cycloplegic autorefraction were compared.
DiscussionThe present study shows that sphere in cycloplegic autorefraction and astigmatism in dry autorefraction is in better agreement and correlation with the results of subjective refraction. The highest agreement with subjective refraction in SE was seen for cycloplegic autorefraction. Nearly 81.9% of the obtained SE with cycloplegic autorefraction, 67.5% of the results using dry autorefraction and53.1% of the results with wavefront-based refraction were within ±0.25 diopters of subjective refraction values. Compared with sphere of subjective refraction, there was a statistically significant hyperopic shift of about 0.12 D of sphere with cycloplegic autorefraction and a significant myopic shift of about 0.17 D with the value obtained with dry autorefraction in most of patients, while the difference between wavefront-based refraction and subjective refraction was not statistically significant. According to cycloplegic refraction, some patients showed a myopic shift. There are several explanations for this phenomenon: Incomplete cycloplegia and the increased accommodative effort may be considered as a causative factor; however, we tried to minimize this error by providing sufficient time for cycloplegia, drug administration by the examiner and determining refractive error by the same optometrist with residual accommodation ≤0.5 D and the same instrument. Moreover, spherical aberration may be responsible for the myopic shift of refractive error. Some studies reported that spherical aberration increased significantly following cycloplegia.20,21 Gao et al. mentioned a significant reduction in the crystalline lens thickness following cycloplegia and backward lens shift which increased spherical aberration.22 Therefore, with a mydriatic pupil, the crystalline lens’ periphery is engaged in retinal image creation, which rises a positive spherical aberration and moves the image focus towards an anterior plane.23
In agreement with the current study, it was reported that dry or non-cycloplegic autorefraction may lead to over-minus or under-plus refractive outputs.24 Giessler et al. showed aberrometers tend to underestimate myopia,25 which is contrary to the previously reported instrumental myopia induced by most of aberrometers.4,26 Thibos et al. suggested that aberrometry may eventually become the new standard for optimal correction of refractive error,27 although aberrometry can provide a tremendous amount and detailed data on total aberration and each component of the Zernike polynomial decomposition of the wavefront error.
For the comparison of objective refraction methods, some influencing factors have to be considered. First, the spherical and cylindrical lenses chosen by the patient may compensate for not only the spherocylindrical (lower order) aberrations, but also part of their higher orders aberrations.28,29 It is known that coma can be compensated for, in part, by a cylindrical lens and spherical aberration by a spherical lens in a particular pupil size. Higher order aberrations may influence manifest refraction, and can be compensated for by using different spherical and cylindrical combinations when measuring subjective refraction,27,30 while wavefront measurements split clearly between true spherical/cylindrical components and other higher orders aberrations. According to the types of higher order aberrations, spherical or cylindrical components may differ from the subjective refraction. Second, the pupil sizes during measurements is another possible factor explaining our outcomes.31 A 3-mm smaller region of the pupil was used during the autorefraction while a 6-mm optical zone was usually chosen when using the wavefront-based refraction. Third, accommodation during measurement (instrumental myopia) could play a role when not dilated. There are other studies which found more myopic refraction using different aberrometers, and the instrumental myopia was proposed as one possible explanation for such findings.5,15,32 Fourth, in evaluating the refractive data, the aberrometers’ repeatability should be considered. In investigations on human as well as model eyes, some studies have shown acceptable repeatability of aberrometric measures,12,33–37 while others demonstrate short-term variations in aberrations secondary to variations in accommodation,38–40 small fixational eye movements40 or even fluctuations in the tear film.39,40 Fifth, wavelength is another parameter which can contribute to a potential artifact in the measurement of aberrometry.35,41 The infrared (IR) light used in wavefront sensors reflects from deeper structures than the apertures of the photoreceptors.42 Martin et al.43 revealed in a study using visible monochromatic light (633 nm) that objective refraction compared to the subjective results were more hyperopic. Sixth, age was repsorted as a possible influencing factor according to the age-related reduction in the the foveal pit depth,44 which results in less impact from the anterior vitreoretinal interface. All these fluctuations together with any illness process, can change the relative place reflecting the light used to select the target refraction in the aberrometric measurement procedure. The present research only included one subject of age above 50 years; therefore, the influence of this factor can be assumed to be very limited.
Comparing with the subjective refraction as a reference, the astigmatism measured by dry autorefraction was more precise than the values obtained with the other methods, although wavefront-based refraction and cycloplegic autorefraction showed good correlation with subjective refraction. Astigmatism components have been generally found to be very similar among wavefront-based and subjective refractions.27,32,45–48 In astigmatism, the correlation between wavefront-based and subjective refraction was not as high as the correlation obtained among the other with the two methods. Pesudovs et al. also reported that wavefront-based refraction were not as precise as standard autorefractions in estimation of astigmatism, although not clinically significantly worse.49
Sphere from cycloplegic autorefraction and astigmatism from dry autorefraction are useful objective clinical data that can used as starting points for subjective refraction for most patients. A point that should be clarified is that refraction and prescription imply distinctive concepts. Prescription refers to a thinking process involving various aspects, including previous prescription, the probability of a new prescription being endured and patient needs.50,51 Therefore, it is concluded that refraction alone fails to be a good alternative for prescription, irrespective of which type of refractions are concerned.
One limitation in the current study was the assessment of the refractive status by an examiner, which may be a source of bias in measurement. It is recommended to repeat the same study in subjects with a previous history of corneal refractive surgery or in cases with irregular corneas.
ConclusionCycloplegic autorefraction in sphere and noncycloplegic autorefraction in astigmatism give a better estimate of subjective manifest refraction. Considering the subjective refraction as the gold standard in correcting refractive errors or modifying the present correction, these findings are very important in situations where subjective refraction is impossible, for example in infants, uncooperative and uncommunicative patients. Both autorefraction and aberrometry results, in general, showed a high level of agreement with subjective refraction.
Conflicts of interestThe authors have no conflicts of interest to declare.