To determine the causes of visual impairment and the use of low vision devices in patients attending the low vision clinic in Trinidad and Tobago.
MethodsA retrospective study of the 222 patients attending the low vision clinic at the University of the West Indies, St Augustine Campus was conducted. The presenting visual acuity, causes of low vision and blindness, and prescribed low vision devices were recorded and analysed to determine the major causes of visual impairment and improvement in visual acuity with low vision aids.
ResultsOut of the total 222 participants, 66.66% (n = 148) had low vision while the rest (33.33%, n = 74) were legally blind. Glaucoma was the major cause of low vision (31.08%) and blindness (28.38%) followed by diabetic retinopathy (20.94%, low vision and 20.27%, blindness). A total of 193 low vision devices were prescribed, 79.79% (n = 154) near devices and 20.20% (n = 39) distance devices. The low vision devices were effective in improving both near visual acuity (120 participants reading 1M or 2M) and distance visual acuity (VA better than 3/60).
ConclusionThe major causes of vision impairment in Trinidad and Tobago were glaucoma and diabetic retinopathy and low vision devices are effective in improving visual acuity. A comprehensive approach to dealing with the causes of low vision and low vision services are required to mitigate the burden of visual impairment in the country.
Low vision is defined as visual acuity worse than 6/18 to 3/60 in the better eye or severely restricted visual field (<10° from the central fixation) even after medical and optical treatment. Visual acuity of less than 3/60 is considered as the criteria for legal blindness. Globally, it has been estimated that 253 m suffer from visual impairment including 36 m blind in 2015.1 The major causes of visual impairment are reported to be cataract (52 m), followed by age-related macular degeneration (8.4 m), glaucoma (4 m), and diabetic retinopathy (2.6 m).2
Trinidad and Tobago is the twin island state in the Caribbean with a population of 1.3 m composed of 35.4% East Indians, 34.2% African and 22.8% mixed ethnicities.3 The country is classified as a high-income country with per capita GDP of USD 16,127.4 Trinidad and Tobago spends 5.5% of its GDP in health, however, the healthcare provision faces serious challenges.5,6
While many studies have assessed the causes of visual impairment from various regions of the World, there are only a few studies from the Caribbean region. The Barbados eye study reported prevalence of blindness and low vision of 1.7% and 5.7% respectively in adults above 40 years of age with the major causes being cataract (32%) and glaucoma (28%).7 A recently conducted National Eye Study of Trinidad and Tobago (NESTT) reported blindness prevalence of 0.73% and moderate to severe visual impairment (MVI) of 5.34% in adults above 40 years of age.8,9 The major causes of blindness were reported to be glaucoma (28.6%) and cataract (25.7%), followed by diabetic retinopathy (11.4%). The major causes of moderate to severe visual impairment were uncorrected refractive error (44.0%) and cataract (30.1%).8,9
While the population based studies provide important data on various causes of visual impairment, it does not consider visual impairment after the best medical/optical correction. The information about the causes of low vision could be important to develop appropriate strategies to reduce the prevalence of visual impairment, especially those due to preventable and curable causes. The major causes of low vision vary across different population around the world. The major causes of low vision are reported to be albinism (31.9%) in Jordan,10 retinitis pigmentosa (16.6%) in Nigeria,11 optic atrophy (28.9%) in Saudi Arabia,12 and congenital cataract (14.38%) in China.13 Different studies also show the importance of low vision services with improvement in visual function through low vision rehabilitation using optical and non-optical interventions.14,15
In Trinidad and Tobago, low vision rehabilitation has only been recently introduced. The University of the West Indies (UWI) optometry unit runs the only comprehensive low vision clinic in the country. In addition, the clinic also dispenses free low vision aids with support from the Trinidad and Tobago Blind Welfare Association (TTBWA). The clinic acts as a referral center for patients with low vision from all over the country. The evaluation of causes of low vision and improvement with low vision aids in patients attending the UWI optometry low vision clinic could hence provide important information on causes of low vision in the country.
MethodsA retrospective analysis of all clinical records of patient attending the low vision clinic at the University of the West Indies Optometry Unit, St Augustine, Trinidad from November 2010 to July 2018 was carried out. Patients with the best corrected visual acuity of equal to or worse than 6/18 to perception of light (PL) or visual field less than 10° who had complete clinical record were included.
The details about demographic distribution, presenting visual acuity and clinical findings were recorded. In addition, the information on low vision trials and low vision devices prescribed were also collected. To determine the cause of low vision, the conditions affecting both eyes in all individuals were listed. In the cases where the primary cause of visual impairment could not be ascertained, the presenting pathology was recorded as the cause of low vision. The secondary cause that could contribute to visual impairment was also recorded. The determination of primary and secondary causes were based on the clinical judgement on the severity/stage of different conditions. The pathology at a more advanced/severe stage was recorded as the primary cause. The information on low vision trial was collected including devices dispensed and visual improvement through those devices. All data were tabulated in an excel sheet and analysed using SPSS software (IBM) to determine common causes of low vision and improvement in visual acuity with low vision aids. The study followed the Declaration of Helsinki and the procedure was approved by the Ethics Committee of the University of the West Indies, St. Augustine campus.
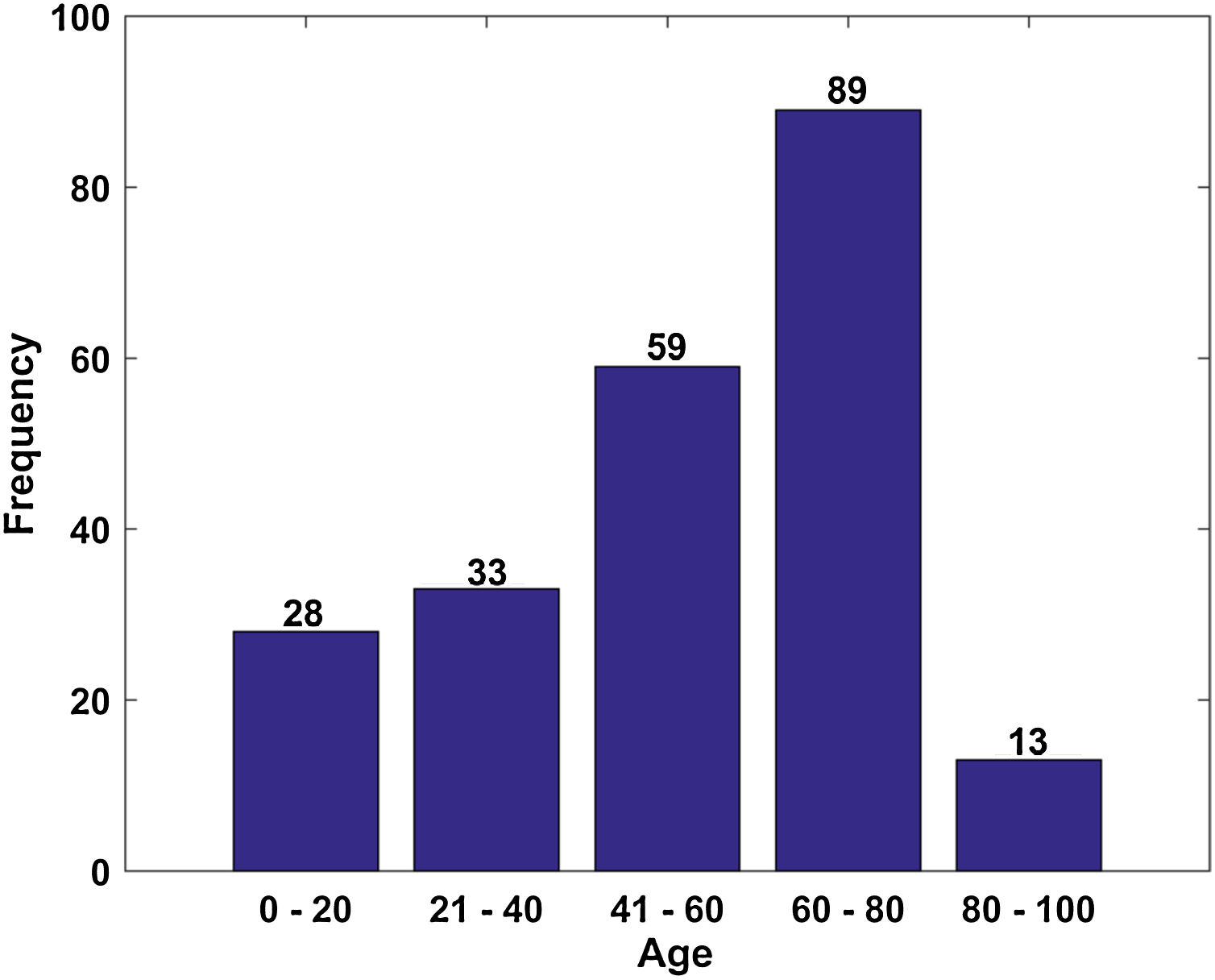
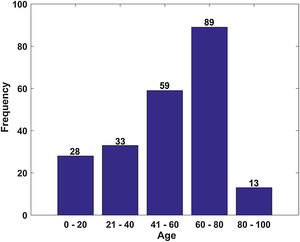
ResultsA total of 264 clinical records of patients attending UWI optometry low vision clinic were obtained. Out of these, 42 were excluded from the study as 23 did not have full clinical information while 19 were excluded as these showed participants improved their visual acuity to better than 6/18 after refractive correction. Among the remaining 222 participants, 124 were male and 98 were females (M:F ratio = 1.26). The mean age of patients was 52.99 (± 22.25) years with the majority of the patients between 60–80 years of age (Fig. 1).
Out of the 222 participants, 177 (79.73%) were referred from other organization/practitioners. Most of the participants (87) were referred from the Trinidad and Tobago Blind Welfare Association (TTBWA) followed by the referrals from optometrists (33) and ophthalmologists (30) working in private practices. 66 participants were already using some form of low vision aids, the most common low vision aid was near magnifiers (63) while two patients were using monocular telescopes and one was using magnifying spectacles (TV spectacles). A total of 131 (59%) participants had one or multiple associated systemic disorders. Among these 99 participants had diabetes and 74 suffered from hypertension.
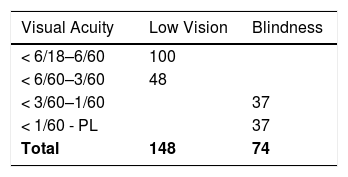
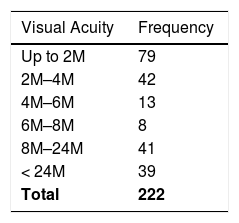
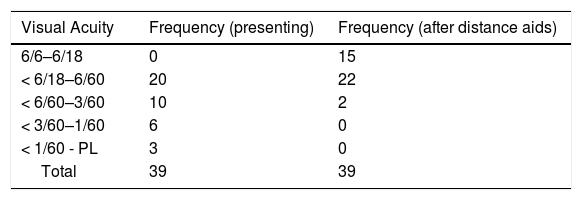
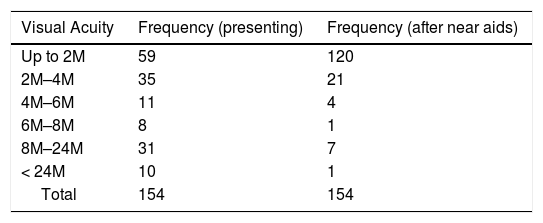
Presenting visual acuityOut of 222 patients attending the low vision clinic, 148 had low vision while 74 were legally blind (Table 1). Most patients (n = 100) with low vision had mild visual impairment (6/18–6/60). For near vision, 79 participants had acuity better than 2M while 80 participants had worse than 8M (Table 2).
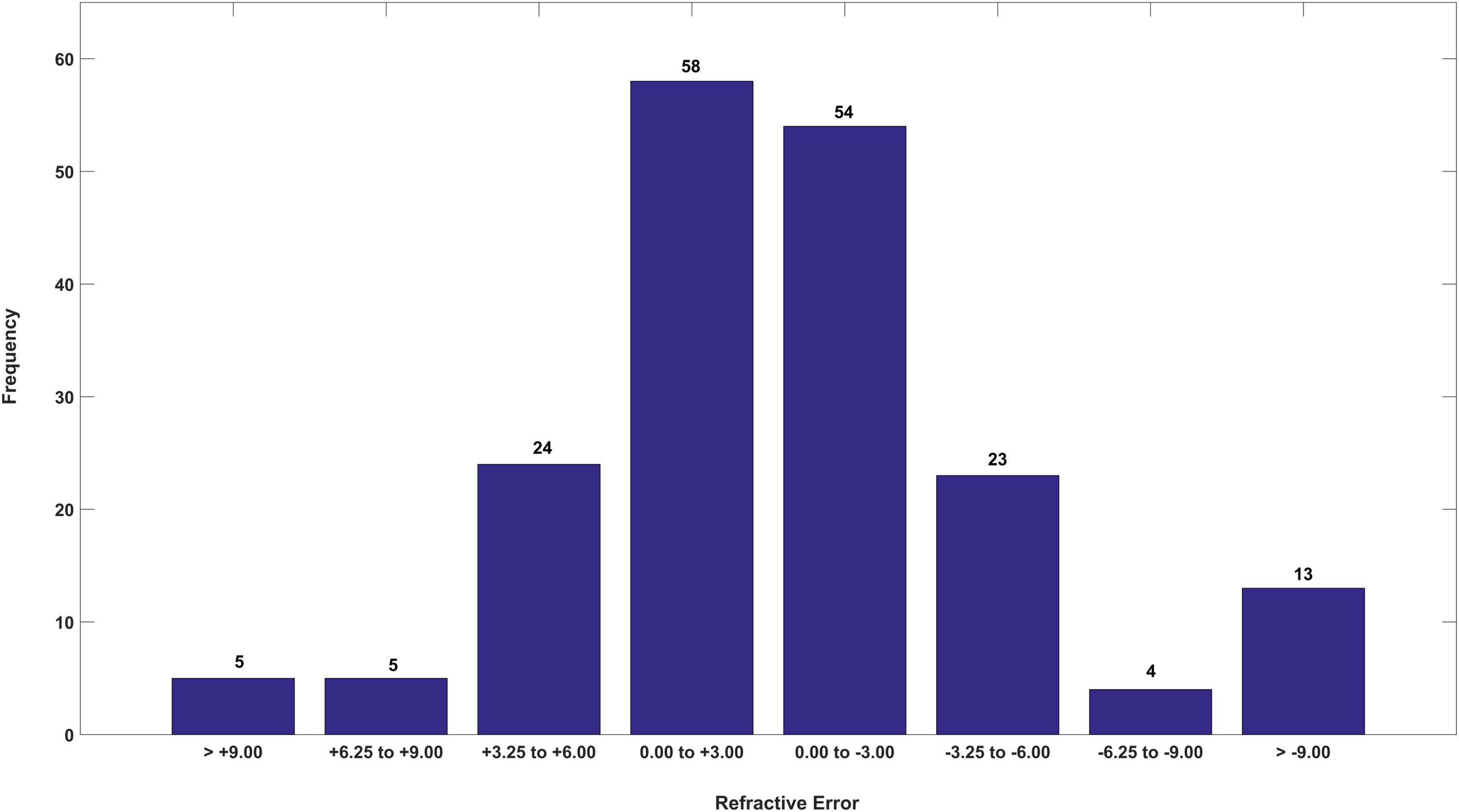
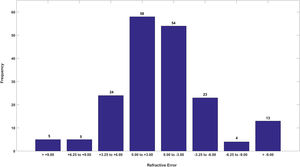
Out of a total of 222 patients, 186 patients had refractive error. Most of those with refractive errors were between ±3.00Ds (n = 112) with 18 patients having errors >±9.00Ds (Fig. 2).
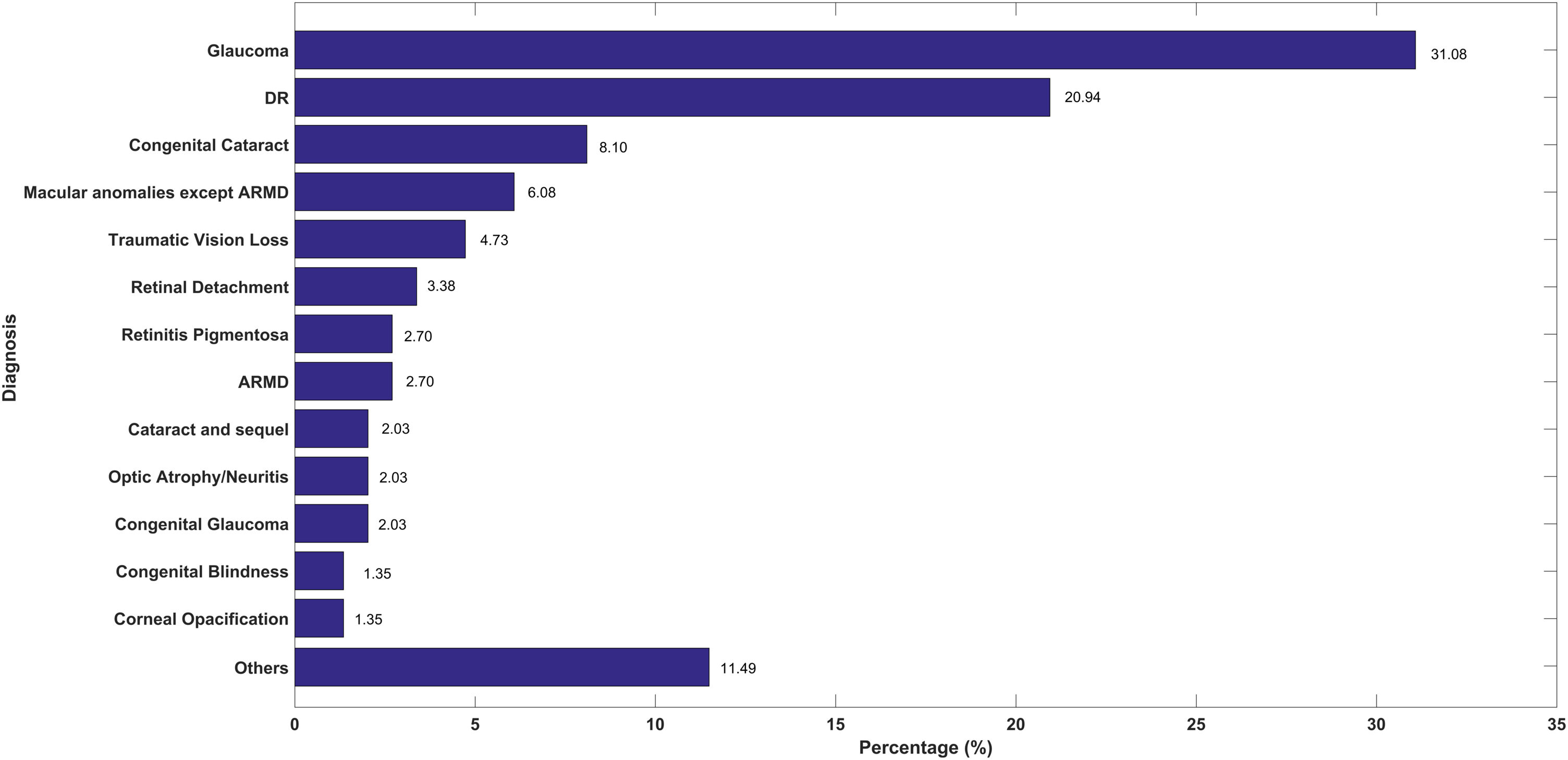
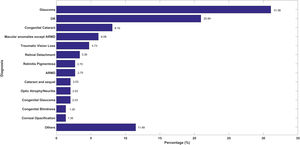
Causes of low visionThe most common primary causes of low vision were glaucoma (n = 46, 31.08%) and diabetic retinopathy (n = 31, 20.94%) followed by congenital cataract (n = 12, 8.10%) and traumatic vision loss (n = 7, 4.73%)—Fig. 3. The traumatic vision loss included various causes such as cataract, retinal detachment, and corneal opacities following history of traumatic episode.
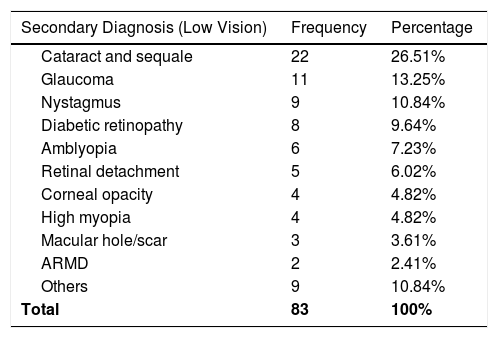
The secondary/associated causes were observed in 83 participants with low vision. The most common secondary cause was cataract and its sequale (n = 22, 26.50%), cataract (n = 21) and sequale (n = 1). This was followed by glaucoma (n = 11, 13.25%), and congenital nystagmus (n = 9, 10.84%)—Table 3.
Secondary causes of low vision.
| Secondary Diagnosis (Low Vision) | Frequency | Percentage |
|---|---|---|
| Cataract and sequale | 22 | 26.51% |
| Glaucoma | 11 | 13.25% |
| Nystagmus | 9 | 10.84% |
| Diabetic retinopathy | 8 | 9.64% |
| Amblyopia | 6 | 7.23% |
| Retinal detachment | 5 | 6.02% |
| Corneal opacity | 4 | 4.82% |
| High myopia | 4 | 4.82% |
| Macular hole/scar | 3 | 3.61% |
| ARMD | 2 | 2.41% |
| Others | 9 | 10.84% |
| Total | 83 | 100% |
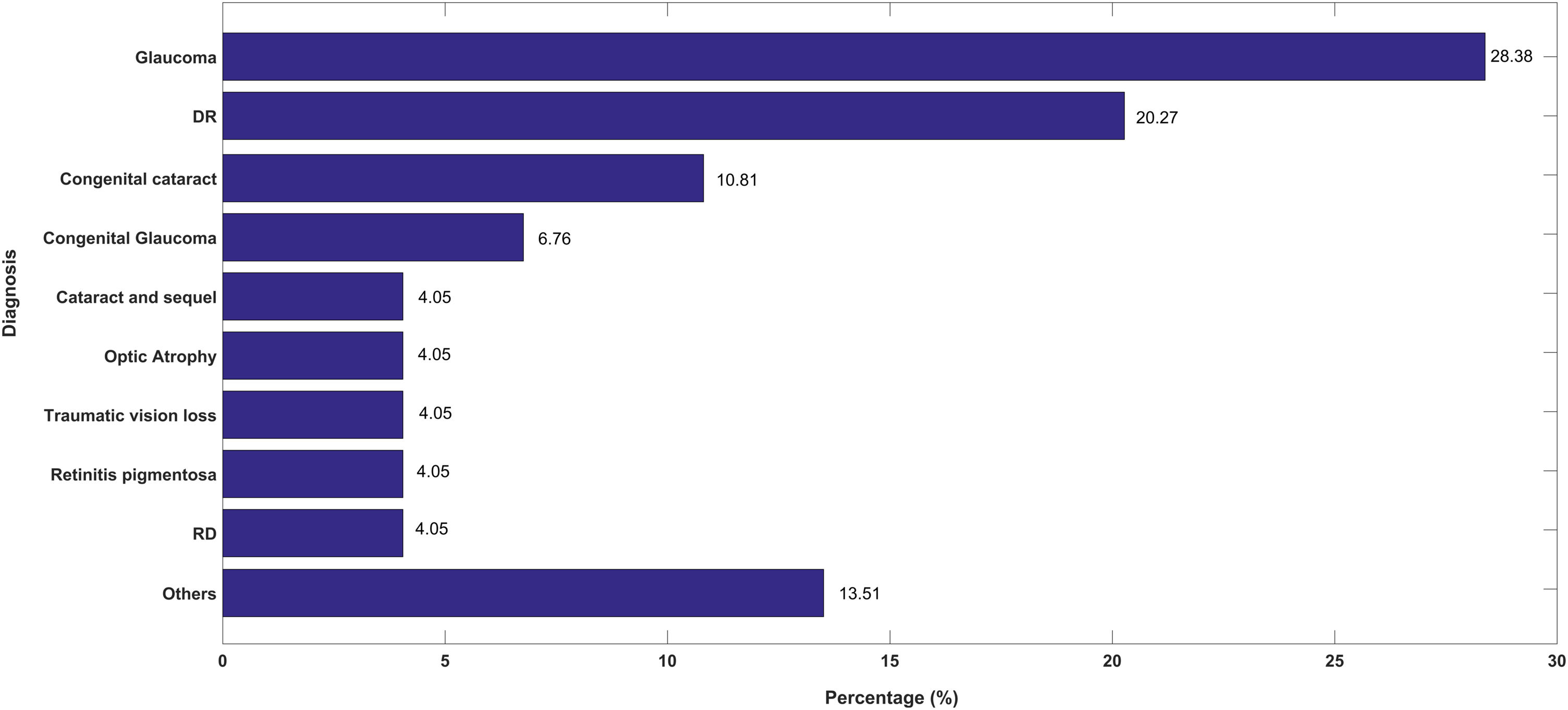
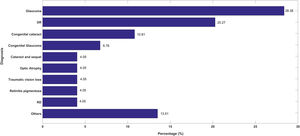
The major cause of legal blindness (VA < 3/60) were glaucoma (n = 21, 28.38%) and diabetic retinopathy (n = 15, 20.27%) followed by congenital cataract (n = 8, 10.81%) and congenital glaucoma (n = 5, 6.76%)—Fig. 4. Secondary associated cause of blindness was also identified in 37 participants with cataract and its sequale being the most common cause (n = 15) followed by retinal detachment (n = 6) and amblyopia (n = 4).
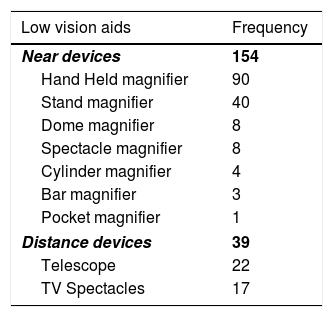
Low vision aidsA total of 154 near low vision aids were dispensed (Table 4). The majority of these were hand-held (n = 90, 58.44%) and stand (n = 40, 25.97%) magnifiers. Out of these 154 near low vision aids, 37 were illuminated magnifiers.
Using these near devices, 120 participants had near visual acuity between 1M and 2M (75 could read 1M) Table 5. A total of 39 distance devices were also dispensed, these included telescopes and TV spectacles. All 39 participants improved with the distance low vision aids with 9 participants previously in blindness category improving to visual acuity better than 3/60 and 15 participants improving to visual acuity normal range (6/6–6/18). (Table 6)
This is the first study to evaluate the causes of low vision in Trinidad and Tobago. The major causes of low vision, as well as blindness in the study were glaucoma and diabetic retinopathy. The finding is similar to the recently conducted population based study which showed glaucoma as the main cause of blindness (31.7%).8,9 The high prevalence of glaucoma has been reported before in the Caribbean population in Barbados,7 St. Lucia,16 and Suriname.17 The high prevalence of blindness and low vision due to glaucoma could be due to the genetic susceptibility of the population as South Asian and African populations are reported to be at higher risk of glaucoma.18,19 The high prevalence of glaucomatous visual impairment could also be due to the insufficient eye care infrastructure to tackle the condition. A recent study reported poor infrastructure for glaucoma diagnosis and management in public hospitals in Trinidad and Tobago.5 Glaucoma features prominently as the major cause of visual impairment worldwide.2,18,20 However, a study reported a reduction in glaucoma blindness in high income countries which is attributed to improved diagnosis and management of the condition.20 The improvement in diagnosis and management of glaucoma in Trinidad and Tobago could reduce the prevalence of visual impairment due to the condition.
Diabetic retinopathy (DR) was the second most common cause of visual impairment (20.94%) as well as blindness (20.27%). The NESTT study also reported DR as the third major cause of blindness (11.4%) in Trinidad and Tobago.8,9 High rates of diabetes were previously observed mainly in American and European populations with DR reported as the leading cause of blindness in the working age adults in the western world.21 In more recent times, there has been worldwide increase in the prevalence of diabetes (projected at 7.7% by 2030 worldwide) and associated ocular complications such as DR.22 The prevalence of diabetes has also been in a steady rise in Trinidad and Tobago from 3.45% in 196823 to 13% in 2013.24 Diabetes featured as the most common systemic disorder (44.59% of total 222 participants) in the sample population. The South Asian and African/Afro-Carribean populations that comprises the population of Trinidad and Tobago are reported to be at higher risk of diabetic retinopathy.25 There also seems to be an issue of poor compliance with regards to compliance/monitoring of DM treatment in Trinidad and Tobago, with a study showing only 44.7% of diagnosed diabetics had their blood glucose level under control.26 The high prevalence of visual impairment due to glaucoma and DR could also be due to the increase in the old aged population in the country, 9.8% above 65 years in 2011,27 as increasing age is a risk factor for both conditions.28–30 These multiple factors could have resulted in high prevalence of blindness and visual impairment due to glaucoma and diabetic retinopathy.
The congenital conditions (cataract and glaucoma) were also a significant cause of both blindness (10.13%) and low vision (17.57%). While congenital conditions feature as the major cause of visual impairment worldwide,13 the high prevalence of congenital disorders could also be due to the lack of provision of neonatal eye examination to detect conditions such as congenital cataract and glaucoma in Trinidad and Tobago.5
Another interesting finding from the current study is the low occurrence of low vision (2.70%) and blindness (none) due to age related macular degeneration (ARMD). The NESTT study also reports relatively low prevalence (2.8%) of visual impairment due to ARMD. ARMD is the most common cause of both low vision and blindness in the developed countries31,32 and the third most common cause of visual impairment and blindness worldwide.2 ARMD is also frequently reported as the major cause of low vision.33 However, a recent meta-analysis reported lower prevalence of ARMD in Asian (7.4%) and African (7.5%) populations compared to European populations (12.3% ), with no difference between Asian and African populations.34 Considering the ethnic distribution of the Trinidadian population composed of East Indian and African descent, the low prevalence of ARMD seem expected.
Cataract (26.51%) was the most common secondary condition of low vision followed by glaucoma (13.25%). The high number of cataract as the secondary condition could be due to the association with systemic conditions such as diabetes which was seen in around 45% of the study sample. Cataract surgery in diabetic patients is also associated with significant complications,35 which could discourage the surgery being performed. Moreover, there could be a reluctance to conduct cataract surgery in patients with other existing associated causes of visual impairment when the overall surgical output is low. The WHO Vision 2020 indicators suggest that the cataract output to tackle the visual impairment due to the condition should be around 3000 per 1 million population however there is low cataract surgical output (1489 cataract surgery per million population in 2013–14) from public hospitals in Trinidad and Tobago (Table 6).5
Low vision devicesA total of 193 low vision devices were dispensed with the majority (154) being near vision devices. The near visual acuity improved to 1M for 120 participants (out of 154 near prescriptions) with variable working distances. A review reported that low vision devices are effective in improving near visual acuity and such improvements are sustained over time.36 The distance low vision aids were also effective with significant improvement in vision both for participants with blindness and low vision. Various studies have shown clinical improvement in the visual performance with low vision aids, such interventions have been shown to improve the quality of life of the patients.36,37 In the current study, the investigation of change in the quality of life after low vision devices could have informed about the real life effectiveness of the prescribed devices in addition to the clinical improvement of the visual acuities. There is also growing emphasis on the multidisciplinary approach for rehabilitation of individuals with visual impairment with the inclusion of other professionals such as social workers, orientation and mobility specialists, and occupational therapists in addition to eye care professionals.38 Studies have reported that additional low vision rehabilitation such as in home training on the use of low vision devices, environmental modifications, mobility training have variable success on low vision rehabilitation.15,39,40 While these are important considerations, the multidisciplinary approach and additional visual rehabilitation of low vision patients in Trinidad and Tobago could be challenging due to the limited resources and manpower available to provide such services in the near future.
The major causes of low vision and blindness in this study are glaucoma and diabetic retinopathy. There is a need for a more comprehensive approach to dealing with the preventable causes of visual impairment as well as the provision of low vision services that are tailored to the requirement of the population.
Conflicts of interestThe authors have no conflicts of interest to declare.