Artificial Intelligence, Data Science and E-health in Vision Research and Clinical Activity
More infoThe application of artificial intelligence (AI) in diagnosing and managing ocular disease has gained popularity as research highlights the utilization of AI to improve personalized medicine and healthcare outcomes. The objective of this study is to describe current optometric perspectives of AI in eye care.
MethodsMembers of the American Academy of Optometry were sent an electronic invitation to complete a 17-item survey. Survey items assessed perceived advantages and concerns regarding AI using a 5-point Likert scale ranging from “strongly agree” to “strongly disagree.”
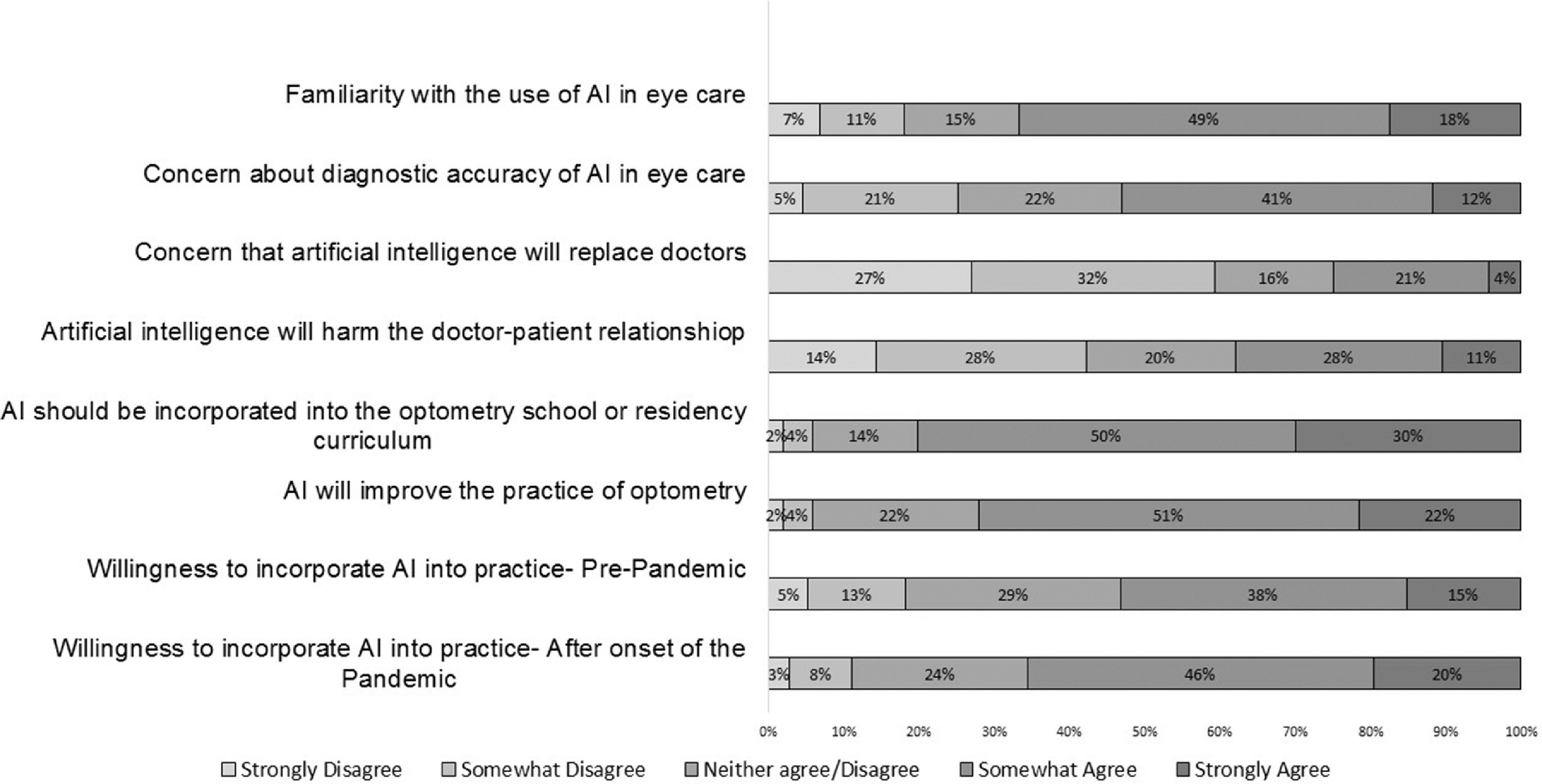
ResultsA total of 400 optometrists completed the survey. The mean number of years since optometry school completion was 25 ± 15.1. Most respondents reported familiarity with AI (66.8%). Though half of optometrists had concerns about the diagnostic accuracy of AI (53.0%), most believed it would improve the practice of optometry (72.0%). Optometrists reported their willingness to incorporate AI into practice increased from 53.3% before the COVID-19 pandemic to 65.5% after onset of the pandemic (p<0.001).
ConclusionIn this study, optometrists are optimistic about the use of AI in eye care, and willingness to incorporate AI in clinical practice also increased after the onset of the COVID-19 pandemic.
Artificial intelligence (AI) is defined as the theory and development of computer systems able to perform tasks that normally require human intelligence, such as visual perception, speech recognition, or decision-making.1 It utilizes software to stimulate cognitive function such as learning and problem solving. Over the last decade, uses of AI have accelerated at an immeasurable pace, with applications involving speech recognition and image interpretation becoming common technologies. In healthcare, AI offers a unique opportunity to assist in many capacities, such as disease screening, management, and patient triage. Studies of AI systems in eye care have shown favorable results.2-4 AI algorithms have been described for image analysis in retinal diseases including diabetic retinopathy, age-related macular degeneration, retinopathy of prematurity, retinal vascular occlusions, and retinal detachment; they have also been described for use in glaucoma, keratoconus, cataract, refractive error, intraocular lens power calculations, and when planning strabismus surgeries.5,6 Most notably, there is a promising role for the use of AI as a screening tool; U.S. Food and Drug Administration approval was obtained for the IDx-DR AI and EyeArt AI systems for diabetic retinopathy screening and the i-ROP Deep Learning system for evaluation of retinopathy of prematurity, which all aid in detecting referral-warranted disease.7-9
In order to understand the potential role and acceptance of AI in optometric practice, it is first necessary to understand provider perceptions towards AI. Previous studies on health care provider and trainee perceptions of AI have reported a willingness to incorporate AI into clinical practice.10-13 However, no study has evaluated optometrist's perceptions of AI to the best of our knowledge. The objective of this study was to describe current optometric perspectives on the application of artificial intelligence in eye care.
Materials and methodsThis study was approved by the University of Illinois at Chicago Institutional Review Board and followed the tenets of the Declaration of Helsinki. Members of the American Academy of Optometry (AAO) were invited by email to participate in a one-time 17-item survey administered via Qualtrics hosted by the University of Illinois at Chicago between September 30, 2020 and November 30, 2020 (Qualtrics, Provo, UT). One reminder email was sent and the survey was designed to allow a single submission per electronic device. No remuneration was provided. The survey was sent to 5092 members of AAO. Optometrists were included if they consented to the survey study.
The survey consisted of three sections: 1) Demographics: including gender, year of graduation from optometry school, completion of residency and residency type, and primary mode of practice. 2) Survey: items to assess perceived advantages and concerns related to AI using a 5-point Likert scale ranging from “strongly agree” to “strongly disagree.” Optometrists were also asked “Prior to the COVID-19 pandemic, I would have been willing to incorporate artificial intelligence into my practice” as well as “In response to the COVID-19 pandemic, I would be willing to incorporate artificial intelligence into my practice”. 3) Free text: additional items were included to further clarify perceptions surrounding AI in eye care. The complete survey is available in Appendix A.
Years since completion of optometry school were categorized by decade: prior to 1990, 1990-1999, 2000-2009, and 2010-2019. Categorical and continuous responses to questions were summarized using descriptive statistics including percentages and means (± standard deviation, SD). A Chi-square goodness of fit test was used to test for equal distribution of proportions for univariate categorical variables. Chi-square test of independence or Fisher's exact test, depending on cell sizes, were used to compare bivariate associations between categorical questions. A two-proportion z-test and a 95% confidence interval for the difference in proportion of those willing to incorporate AI pre and post pandemic was included. A p-value<0.05 was considered significant. All analyses were conducted using R (R Core Team (2019). R: A language and environment for statistical computing. R Foundation for Statistical Computing, Vienna, Austria. URL https://www.R-project.org/.)
ResultsA total of 400 optometrists completed the survey, with an estimated response rate of 7.8% based on an estimated 5092 AAO members. The respondents mean (±SD) number of years since optometry school completion was 25 ± 15.1, and over half were male (54.5%). The majority of respondents completed a residency (55.8%), most commonly ocular disease (34.6%) or primary care (17.6%). The most common mode of practice was private (33.0%) or optometry school (20.0%). Table 1 further describes characteristics of optometrists who completed the survey. Those who more recently completed optometry school were more often women (chi-square test of independence, p<0.01) and more often completed a residency (chi-square test of independence, p<0.01). Table 2 shows the relationship among different characteristics.
Demographics of optometrists in this study.
Relationships among different participant characteristics.
| Completed Residency | ||||
|---|---|---|---|---|
| No | Yes | P-value1 | ||
| Graduation Year | 1990 or earlier | 113 (71.52) | 45 (28.48) | <0.01 |
| 1991-2000 | 29 (40.28) | 43 (59.72) | ||
| 2001-2010 | 22 (24.44) | 68 (75.56) | ||
| 2011-2019 | 13 (16.25) | 67 (83.75) | ||
| Gender | Female | 49 (26.92) | 133 (73.08) | <0.01 |
| Male | 128 (58.72) | 90 (41.28) | ||
| Practice Type | Non-private | 107 (39.93) | 161 (60.07) | 0.02 |
| Private | 70 (53.03) | 62 (46.97) | ||
| Gender | ||||
| Female | Male | |||
| Graduation Year | 1990 or earlier | 33 (20.89) | 125 (79.11) | <0.01 |
| 1991-2000 | 38 (52.78) | 34 (47.22) | ||
| 2001-2010 | 55 (61.11) | 35 (38.89) | ||
| 2011-2019 | 56 (70) | 24 (30) | ||
| Practice Type | Non-private | 137 (51.12) | 131 (48.88) | <0.01 |
| Private | 45 (34.09) | 87 (65.91) | ||
| Practice Type | ||||
| Non-private | Private | |||
| Graduation Year | 1990 or earlier | 94 (59.49) | 64 (40.51) | 0.06 |
| 1991-2000 | 49 (68.06) | 23 (31.94) | ||
| 2001-2010 | 65 (72.22) | 25 (27.78) | ||
| 2011-2019 | 60 (75) |
| ||
The majority of optometrists reported they were familiar with AI (66.8%), and familiarity did not differ based on years in practice (chi-square test of independence, p=0.57) nor residency training (chi-square test of independence, p=0.12). An overwhelming majority, 80.3%, of respondents agreed that AI should be incorporated into the optometry school or residency curriculum. Some optometrists felt that there was concern for AI to replace providers (25.1%), and 38% felt that AI would alter the doctor-patient relationship. Though half of optometrists had concerns about the diagnostic accuracy of AI (53.0%), most believed it would improve the practice of optometry (72.0%). Figure 1 shows the distribution of responses to the survey.
Willingness to Incorporate AI into clinical practice after the onset of the COVID-19 pandemicWhen asked how willing they would have been to incorporate AI into their practice prior to the COVID-19 pandemic, about half (53.3%) of respondents reported willingness to incorporate AI into their practice. When asked in response to the COVID-19 pandemic, how willing they were to incorporate AI into their practice more (65.5%) indicated willingness to incorporate AI into their practice. Using a two proportion z-test, this increase in willingness was significant (95% CI: (+0.05 to +0.19), P<0.01). Of 75 individuals who indicated a change in their wiliness to incorporate AI before and after the onset of the pandemic, 62 (82.7%) changed from neutral or disagree to somewhat or strongly agree. Whether or not a participant had completed a residency or whether they worked in an academic setting (optometry school or academic medical center) versus private practice did not have any association with if their willingness to incorporate AI before and after the onset of the pandemic stayed the same, changed from willing to neutral or disagree, or changed from neutral or disagree to willing (Fisher's exact test, P=0.09 and P=0.17, respectively; Table 3). There was an association between when the participant graduated from optometry school and how their opinion on willingness to incorporate AI before and after the onset of the pandemic changed (Fisher's exact test, P=0.04; Table 3).
Relationship between willingness to incorporate AI pre and during pandemic and participant characteristics.
| Willing to incorporate AI Before and After Onset of the Pandemic | ||||
|---|---|---|---|---|
| Variable | Stayed the same | Neutral/Disagree→Agree | Agree → Neutral/Disagree | P-value1 |
| Completion of optometric residency | ||||
| Yes | 152 (85.88) | 20 (11.3) | 5 (2.82) | 0.09 |
| No | 173 (77.58) | 42 (18.83) | 8 (3.59) | |
| Year of graduation | ||||
| 1990 or earlier | 134 (84.81) | 19 (12.03) | 5 (3.16) | 0.04 |
| 1991-2000 | 59 (81.94) | 8 (11.11) | 5 (6.94) | |
| 2001-2010 | 75 (83.33) | 14 (15.56) | 1 (1.11) | |
| 2011 or later | 57 (71.25) | 21 (26.25) | 2 (2.5) | |
| Type of Practice | ||||
| Private practice | 217 (80.97) | 45 (16.79) | 6 (2.24) | 0.17 |
| Not private practice | 108 (81.82) | 17 (12.88) | 7 (5.3) | |
When selecting what role optometrists believed AI should play in the future of eye care, they indicated: disease screening (86.8%), monitoring disease progression (69.0%), triage and scheduling (61.8%), diagnosis (35.3%), making eye disease management decisions (27.0%) or determining refractive error (27.0%). Additional information on characteristics of respondents who felt AI will replace them and characteristics of respondents who had concerns about accuracy of AI are available in supplementary material, Tables 4 and 5.
Respondents were invited to provide free responses on their perceptions of how AI can improve health care delivery in optometry and what challenges they anticipate with the use of artificial intelligence in optometry. Perceived advantages of AI included improved accuracy (of diagnosis, refraction, and triage), better efficiency, and assistance in monitoring of disease progression. Additionally, respondents commented on the use of AI to improve normative databases, assist in expanding care to the underserved, and ease the burden of documentation on the provider. Potential challenges included assuring practical training before integrating AI into practice, overreliance on the technology, cost, altered patient-provider relationship, and adaptability of the profession as a whole.
DiscussionKey findings from this study are: 1) Although about half of optometrists in this study had concerns about the diagnostic accuracy of AI, the majority agree that AI will improve the practice of optometry; 2) An overwhelming majority of respondents believe that AI should be incorporated into the optometry school or residency curriculum; and 3) Willingness to incorporate AI into practice increased after the onset of the COVID-19 pandemic. Optometrists with varying levels of experience were well represented and there were trends of more female and more residency trained graduates as expected, as over 70% of 2020 graduates were female,14 and the number of residency positions have increased over recent years.15
Half of participants reported concerns about the diagnostic accuracy of AI. It is possible that a lack of familiarity reported by one-third of respondents could play a role in this concern. Previous studies have demonstrated the diagnostic accuracy of AI algorithms compared to eye care providers, including ophthalmologists and optometrists. In a study in which retinal fundus photographs were used for the diagnosis of age-related macular degeneration (AMD), the accuracy of algorithms ranged between 88% and 92%, nearly as high as for expert ophthalmologists.16 Another deep-learning study assessed the need for urgent referral using optical coherence tomography (OCT) imaging and compared the referral by an algorithm to four retina specialists and four optometrists. In 997 patients with a range of 50 retinal pathologies, the algorithm did not miss a single referral case and had an error rate of 3.5%, which was better than all eight experts. Moreover, the clinicians only agreed on 65% of referral decisions.17 Diagnostic accuracy of outcomes in AI algorithms is greatly dependent on the quality of inputs.18 Although many AI platforms are being explored for potential use in the detection, surveillance, and treatment of ocular disease, they are not yet readily available in optometric practices. However, many are in the experimental phase and further evaluation is required to assess if these algorithms are appropriate for clinical practice.
The majority (72%) of optometrists who participated in this survey agree with the statement that AI will improve the practice of optometry. This is consistent with a previous study of ophthalmologists, in which 75% reported agreement that AI would improve their practice.10 Similarly, in a survey of medical students by Pintos dos Santos, 73% of medical students believed AI will play an integral role in healthcare.19 A quarter of optometrists in this study indicated concern that AI will replace doctors. This concern is greater than the study by Pintos dos Santos et al, which reported 3% of physicians believed that the physician would be replaced by AI in the foreseeable future.19 Previous studies have shown AI can complement the role of providers by increasing efficiency in patient care.20 Nevertheless, other studies have discussed caution in patient care, noting that AI dismisses subjective aspects of a disease when looking purely at an algorithm or objective test results.21 When used as a tool within practice rather than a replacement of providers, AI may provide the doctor with supplemental information to more effectively manage eye diseases while affording the doctor more time to provide personalized care, allowing for shared decision-making and improved communication.
Given that an overwhelming majority of respondents believe that AI should be incorporated into the optometry school or residency curriculum, the above examples highlight the importance of educating providers on strengths and limitations of AI before implementation into clinical practice. This may improve familiarity and trust in the accuracy of AI, which were sentiments noted in the current study. The topic of AI in eye care is just recently gaining traction in optometry, with the first American Academy of Optometry meeting lectures and abstracts on the topic presented in 2019.22 Perhaps increased participation in AI during optometry school and residency and more continuing education opportunities will result in a more positive opinion of the technology. Since no research on the topic currently exists in the literature, future studies should look at AI in optometry school and residency curricula since the onset of the pandemic. Curricula implemented in residency and optometry school as well as in continuing education for practicing optometrists should address understanding primary literature in AI, identifying the limitations of AI, and learning about potential applications for clinical practice. Suggested concepts for medical education on the topic of AI include fundamental concepts of AI and machine learning, appropriate clinical use, interdisciplinary care, ethics, quality and safety.23,24
Limitations of AI include issues with generalizability and overcoming regulatory and medicolegal issues.20,25 As previously mentioned, a significant number of images are required for each training set, and the performance of the AI algorithm is dependent on both the number of images and how representative the data are.6 Medicolegal risk is likely dependent on the difference amid assistive AI as opposed to autonomous AI systems, and more work is needed in order to regulate the use of AI systems. These limitations are important for inclusion into AI curricula aimed at practicing and trainee optometrists. Future studies should include questions related to medicolegal concerns of optometrists.
Reported willingness to incorporate AI into clinical practice increased after the onset of the COVID-19 pandemic, from 53.3% to 65.5%. Of those whose willingness to incorporate AI changed, over a quarter of optometrists graduating after 2011 showed the greatest shift toward willingness to adopt AI after the onset of the pandemic. Our healthcare system has been transformed by the COVID-19 pandemic, requiring changes in clinical workflows and adaption of new technologies in order to continue to provide quality care. Clinically, the pandemic has prioritized the rapid adaptation of telehealth and AI. A survey of ophthalmologists prior to the onset of the COVID-19 pandemic showed that most participants agreed telehealth was an important application in eye care, though many felt modalities needed further validation.26 During the peaks of the pandemic, telemedicine bridged the gap between patients and providers allowing for ongoing management. A survey of clinicians by the All India Ophthalmological Society reported almost all, 98.6% of clinicians, had interest in adding telehealth into their practice during the COVID-19 pandemic.27 Perhaps, in our study, experiencing such a drastic change in the healthcare system landscape early in an optometrists’ career prompted young graduates to be more willing to adapt to change. Future qualitative studies will help in understanding why opinions shifted in this group. As AI options continue to expand and become more common, researchers and clinicians will likely be more accepting of their integration into clinical practice, and areas for future development include the integration of AI into telemedicine platforms and the practice of telehealth. Overall, a change in optometrists’ attitudes toward accepting AI could be encouraged in a few different ways. Examples include exposure to more peer reviewed research, continuing education by leaders at local, state, and national society meetings, incorporation of AI in optometry school or residency curricula, and clinician hands-on experience. Focus should be on the accuracy of AI platforms, adapting to new clinical workflows, and the use of AI as a tool in clinical decision making.
Several study participants mentioned that AI will assist in expanding care to the underserved. Health disparities within eye care are well documented. Glaucoma, diabetic retinopathy, and overall visual impairment is more prevalent in Blacks and Hispanics than non-Hispanic Whites.28 These findings are due to non-biologic factors such as income, lack of local providers, neighborhood conditions, and the clustering of low socioeconomic status groups.29 AI interventions have been deployed in low and middle income countries to assist in diagnosis, morbidity and mortality risk assessment, disease outbreak prediction and surveillance, and health policy and planning.30 However, researchers warn that work is needed to prevent racial bias into these algorithms6 while assuring that systems are addressing needs in the underserved.
There were a number of limitations to this study that need to be considered. 1) This was a single survey study and the results may not be generalizable across the profession. This pilot study targeted members of the AAO and over half of survey respondents completed a residency. Though increasing, only 21% of optometry school graduates went on to complete a residency in 2019.15 Additionally, more than half of study participants have been in practice for over 20 years, with limited data existing for new graduates; however, given that no research exists on the perspectives of AI in optometry, we find this data to be a first step in addressing AI perspectives in optometrists. It is possible that newer trainees may become more open to new technology and the incorporation of AI, and a study specifically looking at optometry student and resident perceptions could help us better understand this population. 2) Though efforts were made to avoid participants taking this survey more than once, it is possible that multiple surveys could have been submitted by a single participant from multiple devices. 3) A total of 400 optometrists completed the survey. At the time of survey distribution, AAO reported 5092 members; however, not all members are optometrists and we were unable to confirm the total number of members who are optometrists. 4) Typical survey limitations include selection or response bias. This study was completely voluntary and it is possible that optometrist's interested in AI may have chosen to participate in this study based on the topic, increasing positive findings; however, respondents did share concerns about the use of AI in eye care, indicating participation of optometrists who are apprehensive to the technology. Future studies should look at potential areas of AI expansion in the field including screening and using AI to address health disparities, development of both optometry school and continuing education curricula and opportunities to collaborate with ophthalmologists and other eye care providers for screening and treatment.
ConclusionIn conclusion, the majority of optometrists participating in this study believe AI will improve the practice of optometry and should be incorporated into optometry school or residency curricula. Willingness to incorporate AI in clinical practice also increased after the onset of the COVID-19 pandemic. Although some optometrists report concern about the diagnostic accuracy of AI, this could potentially be addressed with increased education. Efforts should be made within educational institutions and optometric organizations to provide education about the implementation of AI as a tool for eye care professionals, to improve clinical decision making and outcomes for patients, while allowing providers to maintain the doctor-patient relationship.
This work was supported by funding by National Institutes of Health/National Eye Institute K12 EY021475 (Scanzera) and P30 EY001792; and an unrestricted grant to the Department of Ophthalmology and Visual Sciences from Research to Prevent Blindness. The views expressed in this manuscript are those of the authors and do not necessarily represent the views of the funding sources.