To compare the visual performance of prototype contact lenses which extend depth-of-focus (EDOF) by deliberate manipulation of multiple higher-order spherical aberration terms and a commercially-available center-near lens (AIR OPTIX Aqua Multifocal, AOMF).
MethodsThis was a prospective, cross-over, randomized, single-masked (participant), short-term clinical trial where 52 participants (age 45–70 years) were stratified as low, medium or high presbyopes and wore EDOF and AOMF on different days. Objective measures comprised high and low contrast visual acuity (HCVA/LCVA, logMAR), and contrast sensitivity (log units) at 6m; HCVA at 70cm, 50cm and 40cm and stereopsis (seconds of arc) at 40cm. HCVA at 70cm, 50cm and 40cm were measured as “comfortable acuity” rather than conventional resolution acuity. Subjective measures comprised clarity-of-vision and ghosting at distance, intermediate and near, overall vision satisfaction and ocular comfort (1–10 numeric rating scale) and lens purchase (yes/no response). Statistical analysis included repeated measures ANOVA, paired t-tests and McNemar's test.
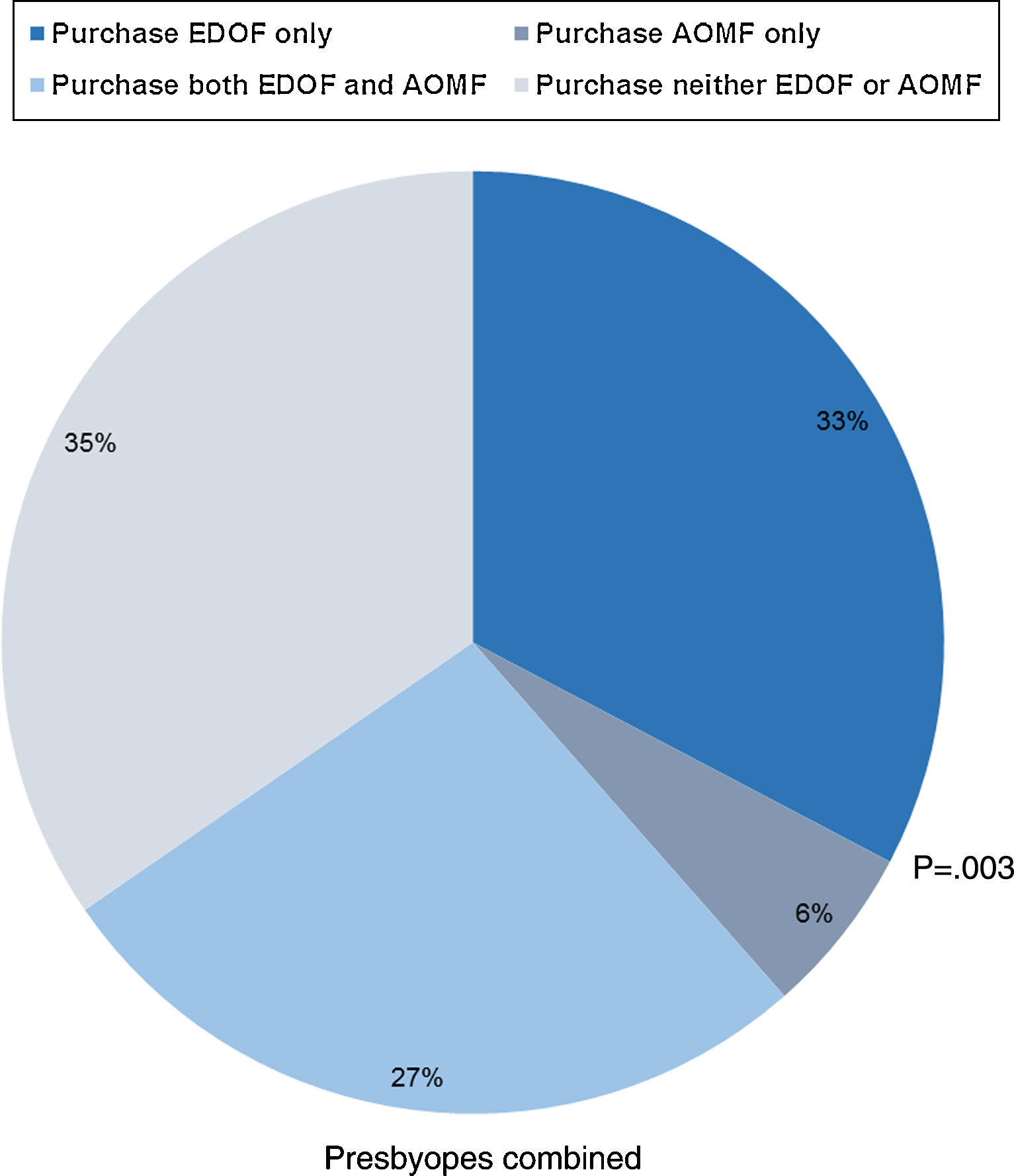
ResultsSignificant differences between lens types were independent of strata (p≥0.119). EDOF was significantly better than AOMF for HCVA at 40cm (0.42±0.18 vs. 0.48±0.22, p=0.024), stereopsis (98±88 vs. 141±114, p<0.001), clarity-of-vision at intermediate (8.5±1.6 vs. 7.7±1.9, p=0.006) and near (7.3±2.5 vs. 6.2±2.5, p=0.005), lack-of-ghosting (p=0.012), overall vision satisfaction (7.5±1.7 vs. 6.4±2.2, p<0.001) and ocular comfort (9.0±1.0 vs. 8.3±1.7, p=0.002). Significantly more participants chose to only-purchase EDOF (33% vs. 6%, p=0.003).). There were no significant differences between lens types for any objective measure at 6m or clarity-of-vision at distance (p≥0.356).
ConclusionsEDOF provides better intermediate and near vision performance in presbyopes than AOMF with no difference for distance vision during short-term wear.
Comparar el rendimiento visual de prototipos de lentes de contacto con las de profundidad de campo extendida (EDOF), mediante la manipulación deliberada de múltiples aberraciones esféricas de alto orden y las lentes de visión simultanea centro-cerca comercialmente disponibles (AIR OPTIX Aqua Multifocal, AOMF).
MétodosEnsayo clínico prospectivo, transversal, aleatorizado, con máscara única (participante), y a corto plazo, en el que se estratificó la presbicia de 52 participantes (de edades comprendidas entre 45 y 70 años) como baja, media o alta; dichos participantes utilizaron lentes EDOF y AOMF en días diferentes. Las mediciones objetivas incluyeron la agudeza visual de alto y bajo contraste (HCVA/LCVA, logMAR), y la sensibilidad al contraste (unidades log) a 6m, HCVA a 70cm, 50cm y 40cm, y estereopsis (segundos de arco) a 40cm. La HCVA a 70cm, 50cm y 40cm se midió como “agudeza de confort” en lugar de la agudeza de resolución convencional. Las mediciones subjetivas incluyeron la claridad de visión y la visión fantasma (ghosting) a distancia, la satisfacción con la visión general intermedia y lejana, el confort ocular (escala de clasificación numérica de 1a 10) y la adquisición de lentes de contacto (respuesta sí/no). El análisis estadístico incluyó la prueba ANOVA con medidas repetidas, la prueba de t pareada, y la prueba de McNemar.
ResultadosLa significación de las diferencias entre los tipos de lentes fue independiente de los estratos (p≥0,119). Los resultados de EDOF fueron considerablemente mejores que los de AOMF en cuanto a HCVA a 40cm (0,42±0,18 frente a 0,48±0,22, p=0,024), estereopsis (98±88 frente a 141±114, p<0,001), claridad de visión intermedia (8,5±16 frente a 7,7±1,9, p=0,006) y próxima (7,3±2,5 frente a 6,2±2,5, p=0,005), ausencia de visión fantasma (p=0,012), satisfacción con la visión general (7,5±1,7 frente a 6,4±2,2, p<0,001) y confort ocular (9,0±1,0 frente a 8,3±1,7, p=0,002). Un número considerable de participantes optó por adquirir únicamente EDOF (33% frente al 6%, p=0,003). No se produjeron diferencias significativas entre los dos tipos de lentes en relación a las mediciones objetivas a 6m, ni a la claridad de visión lejana (p ≥ 0,356).
ConclusionesLas lentes EDOF proporcionaron un mejor rendimiento de la visión intermedia y próxima en pacientes con presbicia que las lentes AOMF, sin que se produjeran diferencias en cuanto a visión lejana con el uso a corto plazo.
The most commonly prescribed multifocal contact lenses (CLs) are soft, simultaneous-image.1 Center-near CLs appear to be the contemporary design of choice as each of the four largest worldwide CL manufacturers (Alcon, TX, USA; Johnson and Johnson, FL, USA; Bausch and Lomb, NY, USA; CooperVision, CA, USA) currently have at least one center-near design in at least two add powers in their inventory. Indeed, the only manufacturer with a true center-distance design recommends a center-distance/center-near combination when reading add is beyond +1.50D.2
Recent improvements in center-near multifocal designs seem to have positively impacted the presbyopic CL market, aided by an aging population.3 Comparing the years 2005–2009 to 2010–2014 shows an increase in both the proportion of presbyopes prescribed CLs (16%4 vs. 22%5–9) and multifocal CL prescribing rates (29%4 vs. 45%5–9).
Center-near lenses have a central maximum positive power and negative primary spherical aberration C(4,0), resulting in a monotonic refractive power profile10 which achieves distance correction in the periphery of the optical zone of the lens.10,11 Unlike non-monotonic zonal-refractive multifocals,10 center-near CLs are pupil-dependent.11 However, simultaneously focused and defocused retinal images can lead to decreased quality of vision,1,12,13 decreased contrast sensitivity13,14 and ghosting.13,15 Despite these limitations, good visual outcomes have been reported with some center-near designs12,16–21 with some studies reporting similar12,19 or better12,16 outcomes compared to a zonal-refractive multifocal. However, these limitations also indicate improvements in multifocal designs are needed to service the current and future presbyopic CL market.
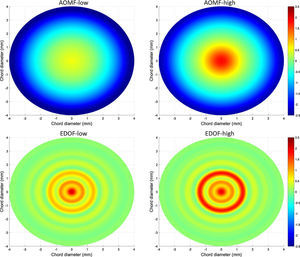
In a previous short-term study, our research group described a novel, cast-molded prototype CL (extended depth of focus [EDOF], Brien Holden Vision Institute, Sydney, Australia) which increases depth of focus by deliberate manipulation of the magnitude and sign of multiple higher-order spherical aberration terms.22 This contrasts with the power profile of either center-distance or center-near aspheric multifocals, which are monotonic in nature, where the power distribution either gradually changes from distance to near power or vice versa.10 EDOF also contrasts with concentric-ring bifocals, which are non-monotonic but their profiles are periodic in nature—there are distinct zones for distance and near correction which are separated equally over the optic zone diameter.10 Unlike these designs, EDOF prototypes are designed using multiple higher-order spherical aberration terms which result in a non-monotonic, non-aspheric, aperiodic, non-diffractive, refractive power profile across the optic zone diameter.22 Compared to a commercially-available, non-monotonic, zonal-refractive multifocal lens, EDOF lenses provided significantly improved intermediate and near vision in presbyopes without compromising distance vision.22
The purpose of the current study was to further assess the clinical utility of these EDOF lenses by comparing their short-term objective and subjective visual performance in presbyopes against a commercially-available, center-near multifocal lens with a monotonic power profile.
MethodThe study design and study procedures have been previously detailed22 and are briefly described here.
Study designThis was a prospective, cross-over, randomized, single-masked (participant), short-term clinical trial conducted at the Clinical Research Trials Centre (CRTC) of the Brien Holden Vision Institute in Sydney, Australia. The trial was approved by a local Human Research Ethics Committee, was conducted in accordance with the principles of the Declaration of Helsinki and registered on the Australian New Zealand Clinical Trials Registry (ACTRN#12613001380785).
ParticipantsSigned informed consent was obtained from participants prior to commencing any study procedures. Participants were required to be healthy with less than 1.00D of astigmatism and correctable to a minimum 6/12 distance high-contrast visual acuity (HCVA) while wearing spherical hydrogel CLs (power range −6.00 to +3.00D). In addition, participants were required to be presbyopic, requiring a minimum +0.75D addition over distance subjective refraction to read 0.1logMAR print on a high contrast black text on white background MNREAD Acuity Chart Card (Precision Vision, IL, USA) at 40cm under photopic conditions (300–350lx).
Baseline proceduresAll baseline procedures were performed under photopic conditions and comprised distance subjective refraction, near addition power measurement, eye dominance identification and acclimatization to the ghosting rating scale used during the trial.
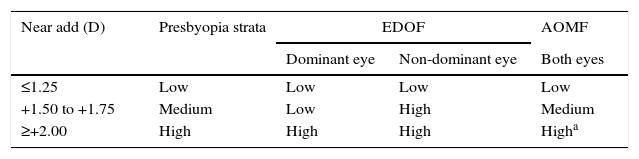
Subjective distance refraction was performed using standard optometric techniques. For the purpose of this trial, participants requiring a negative spherical-equivalent subjective distance refraction were classified as myopes while all other participants were classified as hyperopes. The near add was the minimum plus power required over subjective distance refraction to comfortably read the 0.1logMAR paragraph on a high contrast black text on white background MNREAD acuity card at 40cm. The measured add power was used to stratify participants as low, medium and high presbyopes as shown in Table 1
Presbyopic strata and near power used for each lens type. The near add calculated at baseline was used to stratify participants as low, medium and presbyopes and to determine near power for both lens types.
| Near add (D) | Presbyopia strata | EDOF | AOMF | |
|---|---|---|---|---|
| Dominant eye | Non-dominant eye | Both eyes | ||
| ≤1.25 | Low | Low | Low | Low |
| +1.50 to +1.75 | Medium | Low | High | Medium |
| ≥+2.00 | High | High | High | Higha |
EDOF, extended depth of focus; AOMF, AIR OPTIX aqua Multifocal.
Sensory dominance was the preferred determinant for eye dominance in this study as the eye with least blur tolerance is identified.23 Sensory dominance was assessed on all participants using the alternate blur method24 (single +1.50D trial lens alternated in front of the participant's eyes with the eye reporting greatest subjective blur deemed the dominant eye), and if the dominant eye was identified, no more eye dominance testing was performed. If sensory eye dominance could not be identified, sighting eye dominance was determined using the sighting method24 (“hole-in-the-hand technique”).
The ghosting scale used in this trial has been previously described.22 Briefly, the scale consisted of 10 progressively ghosted letter ‘R's15 (1=no ghosting, 10=severe ghosting) with a letter size of 6/19. Participants were acclimatized to the scale by viewing it at 6m while wearing their subjective distance refraction in a trial frame.
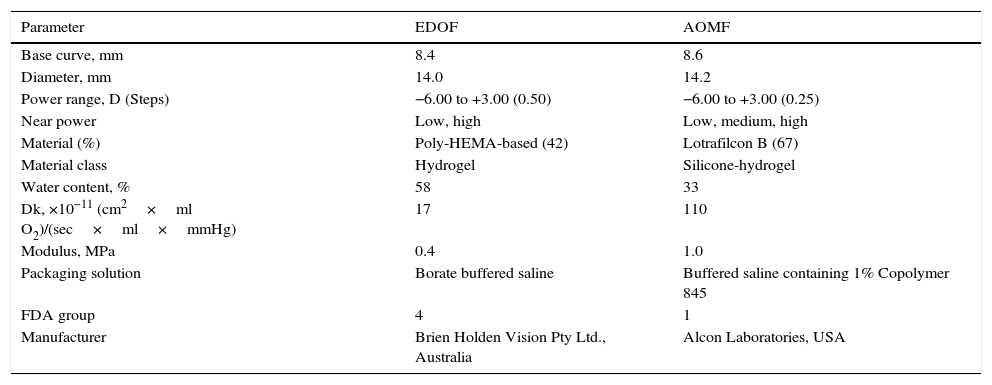
Contact lensesTest CLs in this trial were EDOF and control CLs were AIR OPTIX® Aqua Multifocal (AOMF: lotrafilcon B, Alcon, TX, USA). The parameters, power range used in this trial and physical properties of both CLs are given in Table 2.
Parameters and physical properties of contact lenses used in this trial.
| Parameter | EDOF | AOMF |
|---|---|---|
| Base curve, mm | 8.4 | 8.6 |
| Diameter, mm | 14.0 | 14.2 |
| Power range, D (Steps) | −6.00 to +3.00 (0.50) | −6.00 to +3.00 (0.25) |
| Near power | Low, high | Low, medium, high |
| Material (%) | Poly-HEMA-based (42) | Lotrafilcon B (67) |
| Material class | Hydrogel | Silicone-hydrogel |
| Water content, % | 58 | 33 |
| Dk, ×10−11 (cm2×ml O2)/(sec×ml×mmHg) | 17 | 110 |
| Modulus, MPa | 0.4 | 1.0 |
| Packaging solution | Borate buffered saline | Buffered saline containing 1% Copolymer 845 |
| FDA group | 4 | 1 |
| Manufacturer | Brien Holden Vision Pty Ltd., Australia | Alcon Laboratories, USA |
EDOF, extended depth of focus; AOMF, AIR OPTIX aqua Multifocal; Dk, oxygen permeability.
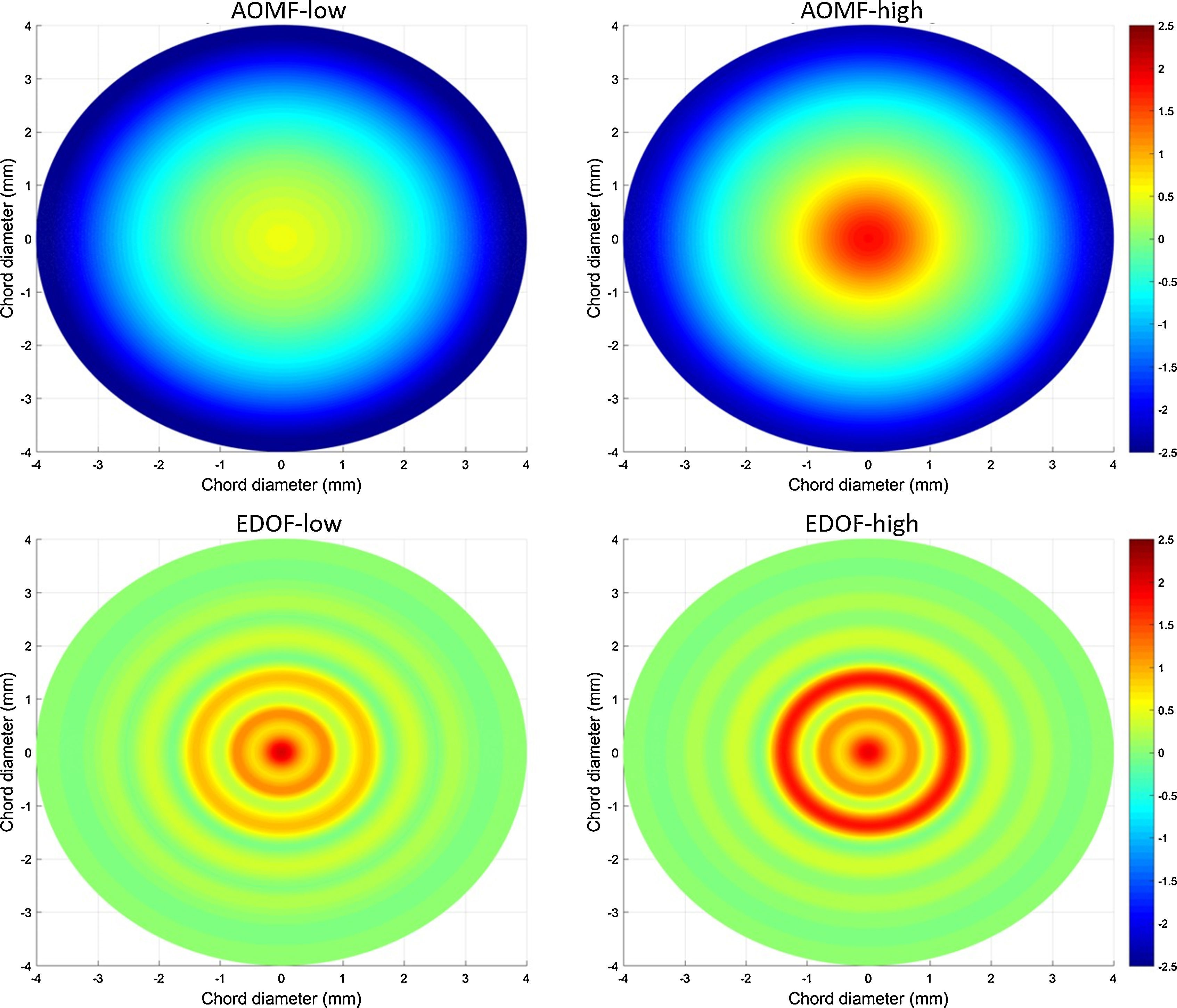
The power profiles of plano distance power for EDOF (low and high power) and AOMF (low and high add) are shown in Fig. 1. These power profiles were measured using the NIMO TR1504 (Lambda-X, Belgium) The profiles show EDOF has a non-monotonic power profile with smooth transition between multiple zones and AOMF has a monotonic power profile with smooth transition from center of the lens to edge of the optic zone.
The initial CL assessed was randomly allocated and participants were restricted to one CL assessment per day. The distance power used for both EDOF and AOMF was based on the spherical equivalent distance refraction. EDOF was only available in 0.50D steps, and so the closest least minus power was used when the spherical equivalent power was unavailable. AOMF was available in 0.25 steps, and so the spherical equivalent power was used for all participants.
The near power chosen for both CLs was based on the participant's near addition measured at baseline. The method used for determining the required near power for EDOF has been previously described22 while manufacturer's recommendations were followed for AOMF lenses.25 The near power chosen for participants are given in Table 1
CLs were inserted by one of several unmasked investigators and participants were masked to CL identity. During a 10min settling time, participants were encouraged to observe distant objects, read printed material or view their phones.
A spherical over-refraction at 6m was performed under photopic conditions. For both test and control CLs, a trial frame and lenses were used to monocularly calculate the maximum plus to best distance HCVA. An additional +0.75D was added binocularly to this result then reduced binocularly in 0.25 steps until the participant could just read the 6/6 line binocularly. Extra plus was given if subjective improvement was demonstrated at near provided binocular distance HCVA was no worse than 6/7.5 and the participant preferred subjective improvement at near compared to slight distance blur. The difference in HCVA between eyes was kept to within one line.
Due to the inequality in power availability between lens types, the over-refraction in a trial frame was worn by participants for all subsequent objective and subjective measurements to optically equalize lens types. A trial frame was not worn if the over-refraction was plano for both eyes.
Objective measurementsObjective measurements were performed binocularly at distance (6m), intermediate (70cm) and near (50cm and 40cm) under photopic conditions. Results were entered directly into a database by the investigator.
Distance measurements at 6m comprised HCVA, low contrast visual acuity (LCVA) and contrast sensitivity (CS). A Test Chart 2000 Pro (Thompson Software Solutions, Hertfordshire, UK) was used for all distance measurements, with contrast set to 100% and 10% for HCVA and LCVA, respectively and CS measured with a Pelli–Robson like chart at 18cycles/degree.
A reading-based assessment was used to measure HCVA at intermediate and near. A high contrast black on white MNREAD Card was held at 70cm, 50cm and 40cm and participants were asked the smallest paragraph they could comfortably read rather than the smallest paragraph they could read. These HCVA results yielded are therefore measurements of “comfortable visual acuity” rather than conventional resolution acuity.22 Measurements taken at 50cm and 70cm were adjusted to equivalent logMAR values prior to analysis.
Near stereopsis was measured at 40cm with the Stereo Fly Test Circles (Stereo Optical, IL, USA).
Subjective measurementsSubjective measurements were assessed binocularly for distance (6m), intermediate (around 70cm) and near (40–50cm) under photopic conditions and results were entered directly into a database by the participant. The investigator only intervened to indicate targets for ratings or clarify rating descriptors.
Subjective ratings were assessed on a 1–10 numeric rating scale (NRS) in 1-point steps as previously described.22 Briefly, the NRS assessed clarity-of-vision (1=blurred, 10=clear) and ghosting (1=none, 10=severe) at distance, intermediate and near.
For clarity-of-vision and ghosting ratings at distance, participants viewed the 6/6 line and 6/19, respectively, of a Test Chart 2000 Pro set to 100% contrast. For clarity-of-vision ratings at intermediate and near, participants viewed the 0.6logMAR paragraph and 0.3logMAR paragraph, respectively, of a high contrast black on white MNREAD Card. For ghosting ratings at intermediate and near, participants viewed the 1.0logMAR paragraph and 0.9logMAR paragraph, respectively, of a high contrast black on white MNREAD Card.
Overall vision satisfaction (1=not satisfied and 10=satisfied) was based on the overall vision experience for all distances. Ocular comfort (1=uncomfortable and 10=comfortable) was measured after all vision assessments were complete.
Participants were asked if they would purchase the CL they were wearing based on their vision experience only (lens purchase). Answers were given as a forced choice yes/no response.
Lens fittingOnce all objective and subjective measurements were complete, lenses were observed on eye with slit-lamp biomicroscopy and assessed for centration (mm, horizontal and vertical), primary lens movement (mm), primary lens lag (mm) and tightness (%).
Statistical analysisA minimum of 20 participants per stratum was required to demonstrate a statistically significant paired difference between lens types in subjective ratings±standard deviation (SD) of 1±1.5 units with 80% power at the 5% level of significance. This sample also had 80% power to detect a paired difference in visual acuity of 0.1±0.15logMAR between lens types. The resultant sample sizes of 19 in the medium and 10 in the high add strata were inadequate for statistical analysis, and were therefore combined into one stratum (medium-high).
Data were summarized as means±SD for variables measured on an interval scale and as percentages for categorical variables. The ghosting rating scale has been reversed in the analyses (referred to as ‘lack-of-ghosting’ in results) to maintain consistency with other scales. Prior to statistical analysis, stereopsis measurements were log transformed because of the positively-skewed distribution and visual acuity measurements were converted to logMAR.
Repeated measures analysis of variance (ANOVA) was used to determine the overall effect of lens type and its interaction with strata and testing distances for HCVA, clarity-of-vision, and lack-of-ghosting. The model included strata as between-participant factor while lens type and various testing distances were factored as within-participant factor. If the interactions of lens type with strata and/or various distances was significant at the 10% level, paired t-tests were used to compare between lens types at each sub level of the interacting factor.
McNemar's chi-square test for paired categorical data was used to analyze lens purchase and the proportion of participants who rated clarity-of-vision≥8 units for all three testing distances and overall vision satisfaction≥8 units with each lens type.
Chi square test was used to analyze the proportion of participants requiring a trial frame and linear mixed model was used to analyze over-refraction power and lens fitting.
The analysis was performed using SPSS 21 (IBM, USA), and the level of significance was set at 5%.
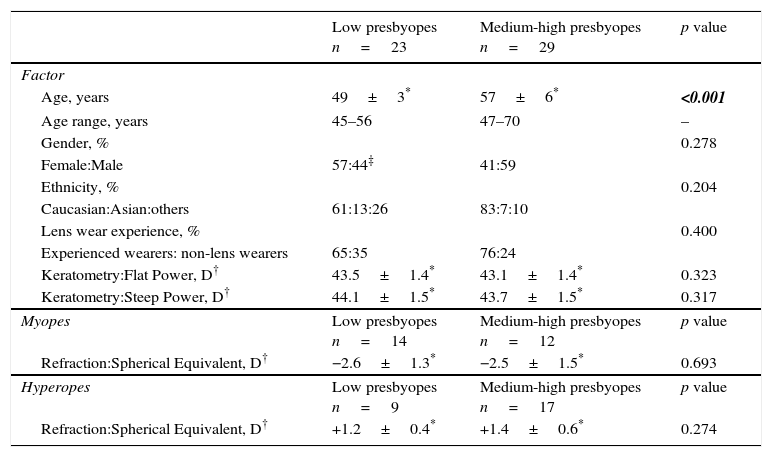
ResultsStudy population characteristicsThe total dataset comprised 52 participants: 48% were female, mean age±SD was 53±6 years, age range was 45–70 years and 71% were experienced contact lens wearers. Demographic details for each strata are given in Table 3. There was a significant difference between strata for age (p<0.001) but not for gender, ethnicity, lens wear experience, keratometry or spherical-equivalent refraction (p≥0.204).
Demographic factors for low and medium-high presbyopes.
| Low presbyopes n=23 | Medium-high presbyopes n=29 | p value | |
|---|---|---|---|
| Factor | |||
| Age, years | 49±3* | 57±6* | <0.001 |
| Age range, years | 45–56 | 47–70 | – |
| Gender, % | 0.278 | ||
| Female:Male | 57:44‡ | 41:59 | |
| Ethnicity, % | 0.204 | ||
| Caucasian:Asian:others | 61:13:26 | 83:7:10 | |
| Lens wear experience, % | 0.400 | ||
| Experienced wearers: non-lens wearers | 65:35 | 76:24 | |
| Keratometry:Flat Power, D† | 43.5±1.4* | 43.1±1.4* | 0.323 |
| Keratometry:Steep Power, D† | 44.1±1.5* | 43.7±1.5* | 0.317 |
| Myopes | Low presbyopes n=14 | Medium-high presbyopes n=12 | p value |
| Refraction:Spherical Equivalent, D† | −2.6±1.3* | −2.5±1.5* | 0.693 |
| Hyperopes | Low presbyopes n=9 | Medium-high presbyopes n=17 | p value |
| Refraction:Spherical Equivalent, D† | +1.2±0.4* | +1.4±0.6* | 0.274 |
Significantly more participants wore a trial frame when EDOF lenses were assessed (71% vs. 42%, p=0.003). There was a significant difference in over-refraction between EDOF and AOMF lenses (−0.09±0.29D vs. +0.02±0.22D, p<0.001).
Objective measurementsRepeated measures ANOVA for HCVA showed non-significant interaction between lens type and strata (p=0.676) while interaction between lens type and testing distances was significant at the 10% level (p=0.053). Due to this interaction, paired t-tests at each testing distance using the entire sample (i.e. presbyopes combined) only were performed.
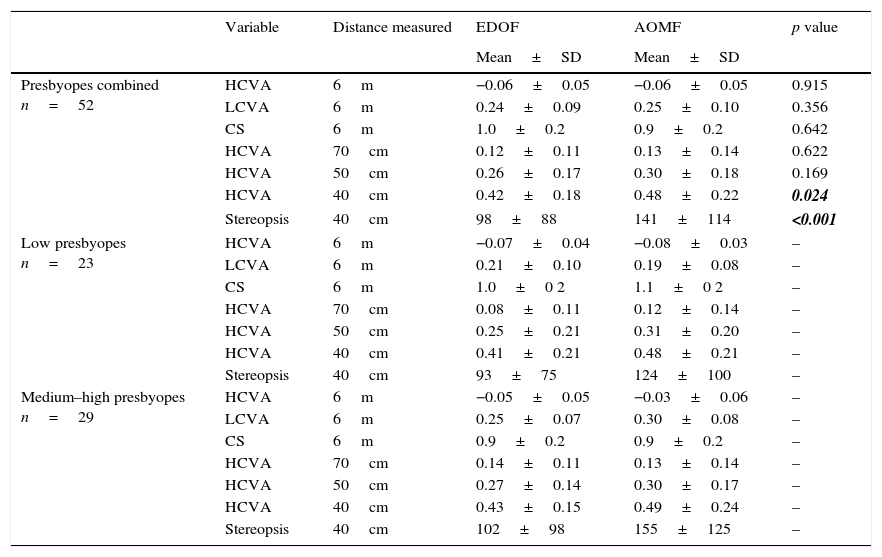
Objective results for presbyopes combined, low presbyopes and medium-high presbyopes are given in Table 4. HCVA and stereopsis at 40cm were significantly better with EDOF (p=0.024 and p<0.001 respectively). There were no significant differences between CL for HCVA at 6m, 70cm and 50cm, LCVA at 6m or CS at 6m (p≥0.169).
Objective measurements while wearing EDOF and AOMF lenses. HCVA at 70cm, 50cm and 40cm are measures of “comfortable acuity” rather than conventional resolution acuity. Descriptive data only is provided for low and medium-high presbyopes as there was no significant interaction between lens type and participant strata (p=0.676). p-values in bold and italicized indicate significant differences between lens types.
| Variable | Distance measured | EDOF | AOMF | p value | |
|---|---|---|---|---|---|
| Mean±SD | Mean±SD | ||||
| Presbyopes combined n=52 | HCVA | 6m | −0.06±0.05 | −0.06±0.05 | 0.915 |
| LCVA | 6m | 0.24±0.09 | 0.25±0.10 | 0.356 | |
| CS | 6m | 1.0±0.2 | 0.9±0.2 | 0.642 | |
| HCVA | 70cm | 0.12±0.11 | 0.13±0.14 | 0.622 | |
| HCVA | 50cm | 0.26±0.17 | 0.30±0.18 | 0.169 | |
| HCVA | 40cm | 0.42±0.18 | 0.48±0.22 | 0.024 | |
| Stereopsis | 40cm | 98±88 | 141±114 | <0.001 | |
| Low presbyopes n=23 | HCVA | 6m | −0.07±0.04 | −0.08±0.03 | – |
| LCVA | 6m | 0.21±0.10 | 0.19±0.08 | – | |
| CS | 6m | 1.0±0 2 | 1.1±0 2 | – | |
| HCVA | 70cm | 0.08±0.11 | 0.12±0.14 | – | |
| HCVA | 50cm | 0.25±0.21 | 0.31±0.20 | – | |
| HCVA | 40cm | 0.41±0.21 | 0.48±0.21 | – | |
| Stereopsis | 40cm | 93±75 | 124±100 | – | |
| Medium–high presbyopes n=29 | HCVA | 6m | −0.05±0.05 | −0.03±0.06 | – |
| LCVA | 6m | 0.25±0.07 | 0.30±0.08 | – | |
| CS | 6m | 0.9±0.2 | 0.9±0.2 | – | |
| HCVA | 70cm | 0.14±0.11 | 0.13±0.14 | – | |
| HCVA | 50cm | 0.27±0.14 | 0.30±0.17 | – | |
| HCVA | 40cm | 0.43±0.15 | 0.49±0.24 | – | |
| Stereopsis | 40cm | 102±98 | 155±125 | – |
HCVA, high-contrast visual acuity; LC, low-contrast visual acuity; CS, contrast sensitivity; EDOF, extended depth of focus; AOMF, AIR OPTIX aqua Multifocal. Units of measurement: HC VA=logMAR, LC VA=logMAR, CS=log units (18 cycles/degree), stereopsis=seconds of arc.
Repeated measure ANOVA for clarity-of-vision ratings showed non-significant interaction between lens type and strata (p=0.119) and significant interaction between lens types and testing distances (p=0.004). Due to this interaction, paired t-tests at each testing distance using the entire sample only were performed.
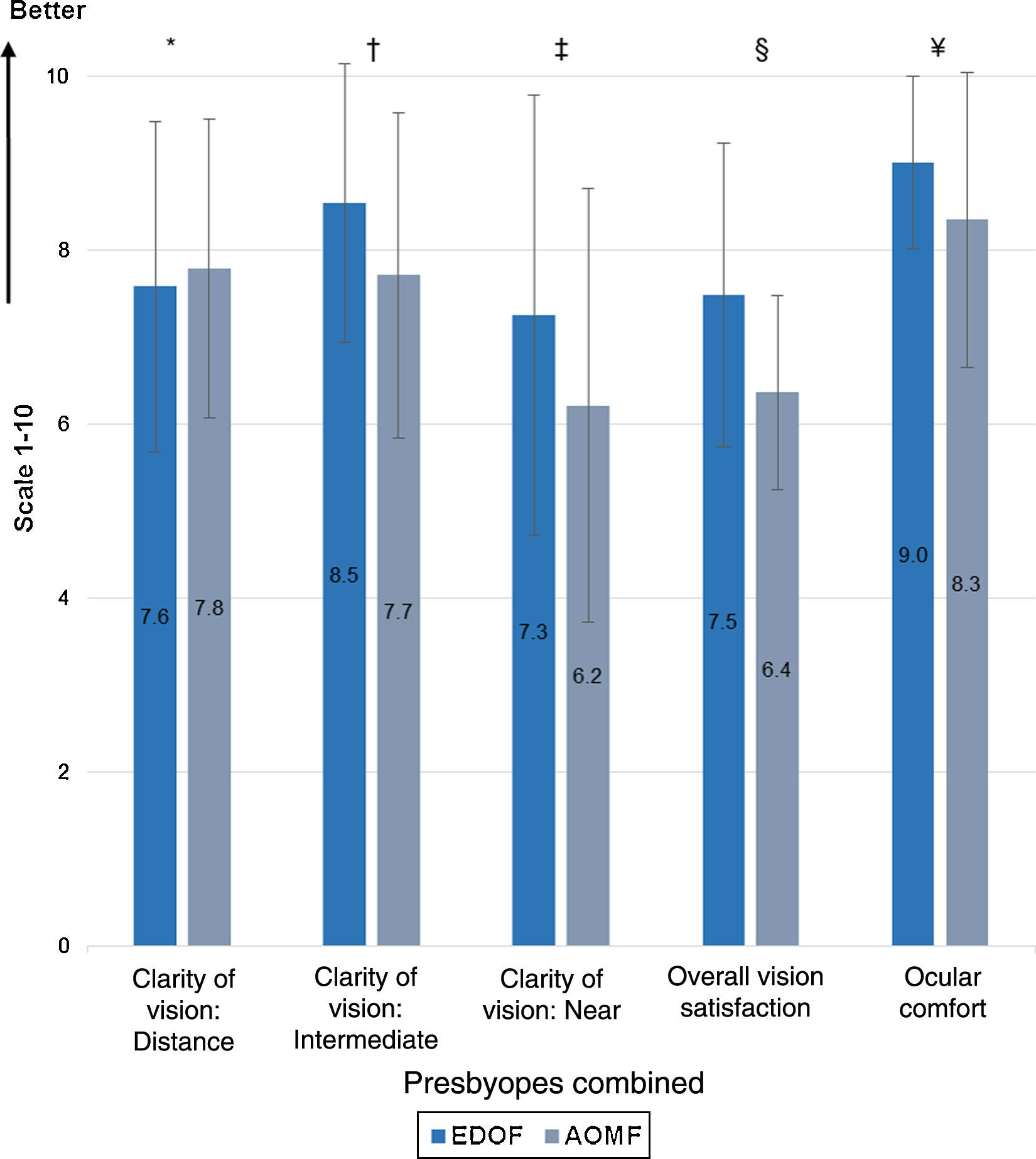
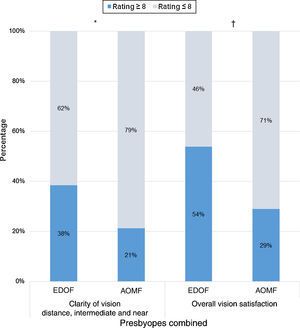
Clarity-of-vision at intermediate and near were rated significantly higher with EDOF (Fig. 2, p=0.006, p=0.005 respectively). There were no significant difference between lens types for clarity-of-vision at distance (Fig. 2, p=0.471).
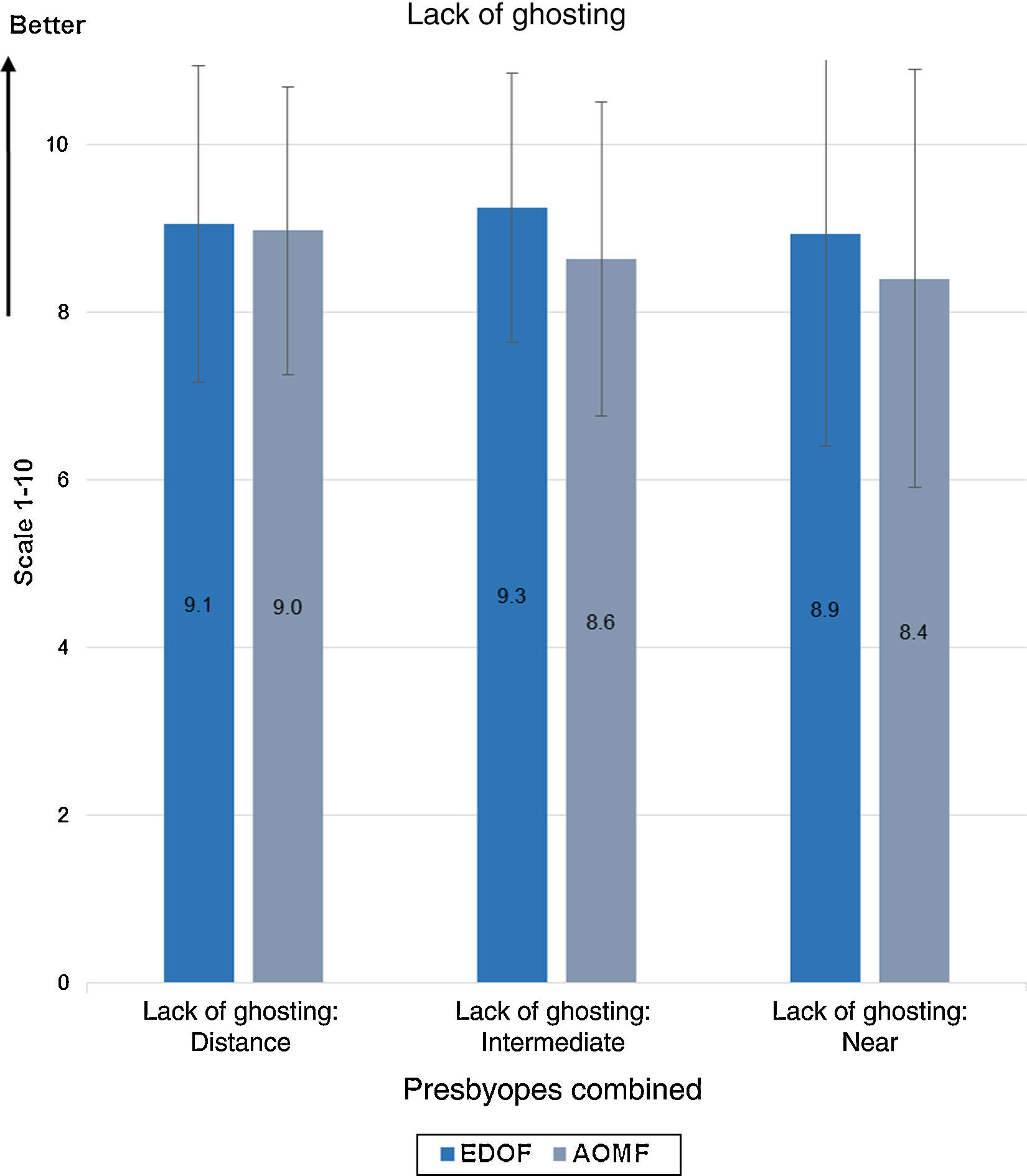
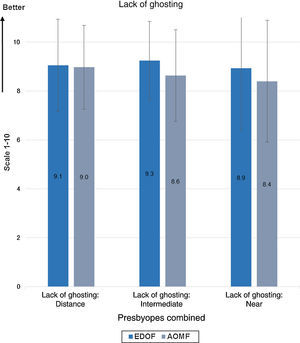
Repeated measures ANOVA for lack-of-ghosting ratings showed EDOF was rated significantly better (i.e. less ghosting, p=0.012), but there was no significant interaction between lens type and strata (p=0.276) or testing distance (p=0.126). Results are given in Fig. 3.
Lack-of-ghosting ratings while wearing EDOF and AOMF lenses for presbyopes combined at distance, intermediate and near. There was a significant difference between lens types for lack-of-ghosting (p=0.012) but no significant interaction between lens type and testing distance (p=0.126). Error bars=1 SD.
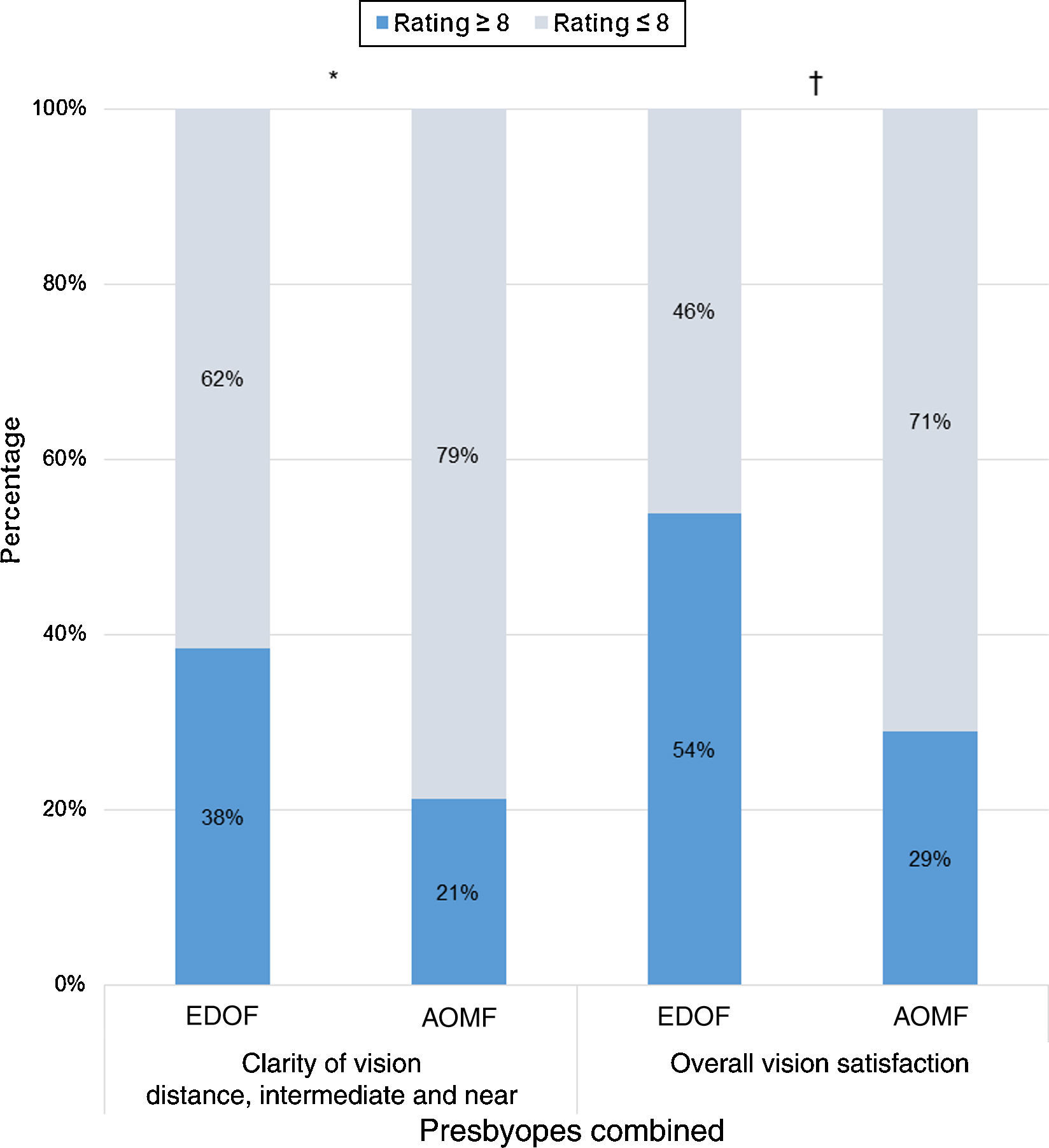
The proportion of participants who rated clarity of vision≥8 units for all three testing distances and overall vision satisfaction≥8 units was significantly higher when EDOF was worn (Fig. 4, p=0.022 and p=0.002 respectively).
Overall vision satisfaction and ocular comfort were rated significantly higher with EDOF (Fig. 2, p<0.001 and p=0.002 respectively).
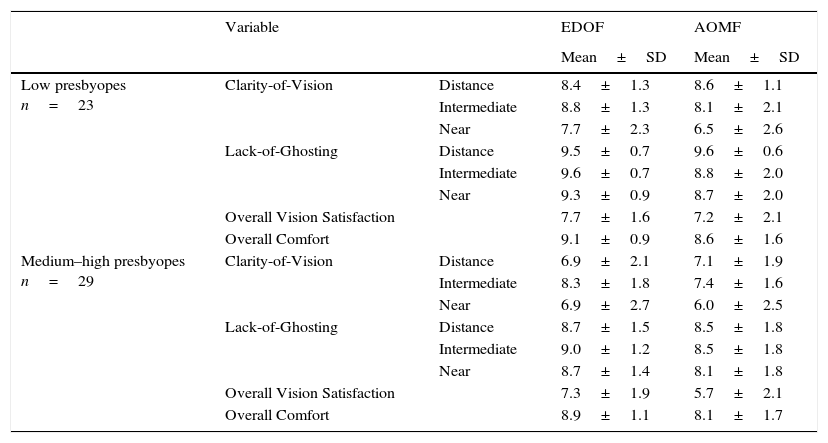
Subjective ratings (descriptive data only) for low presbyopes and medium-high presbyopes are given in Table 5.
Subjective ratings while wearing EDOF and AOMF lenses for low and medium-high presbyopes. Descriptive data only provided as there was no significant interaction between lens type and participant strata for clarity-of-vision (p=0.119) or lack-of-ghosting (p=0.276). Higher ratings represent a better outcome.
| Variable | EDOF | AOMF | ||
|---|---|---|---|---|
| Mean±SD | Mean±SD | |||
| Low presbyopes n=23 | Clarity-of-Vision | Distance | 8.4±1.3 | 8.6±1.1 |
| Intermediate | 8.8±1.3 | 8.1±2.1 | ||
| Near | 7.7±2.3 | 6.5±2.6 | ||
| Lack-of-Ghosting | Distance | 9.5±0.7 | 9.6±0.6 | |
| Intermediate | 9.6±0.7 | 8.8±2.0 | ||
| Near | 9.3±0.9 | 8.7±2.0 | ||
| Overall Vision Satisfaction | 7.7±1.6 | 7.2±2.1 | ||
| Overall Comfort | 9.1±0.9 | 8.6±1.6 | ||
| Medium–high presbyopes n=29 | Clarity-of-Vision | Distance | 6.9±2.1 | 7.1±1.9 |
| Intermediate | 8.3±1.8 | 7.4±1.6 | ||
| Near | 6.9±2.7 | 6.0±2.5 | ||
| Lack-of-Ghosting | Distance | 8.7±1.5 | 8.5±1.8 | |
| Intermediate | 9.0±1.2 | 8.5±1.8 | ||
| Near | 8.7±1.4 | 8.1±1.8 | ||
| Overall Vision Satisfaction | 7.3±1.9 | 5.7±2.1 | ||
| Overall Comfort | 8.9±1.1 | 8.1±1.7 |
EDOF, extended depth of focus; AOMF, AIR OPTIX aqua Multifocal.
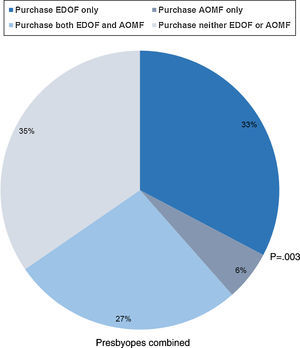
Lens purchase results for presbyopes combined are given in Fig. 5. Significantly more participants indicated they would only purchase EDOF compared to only purchase AOMF (p=0.003). A higher proportion of participants indicated they would purchase EDOF compared to AOMF (60% vs. 33%), 27% would purchase both lens types and 35% would purchase neither lens type.
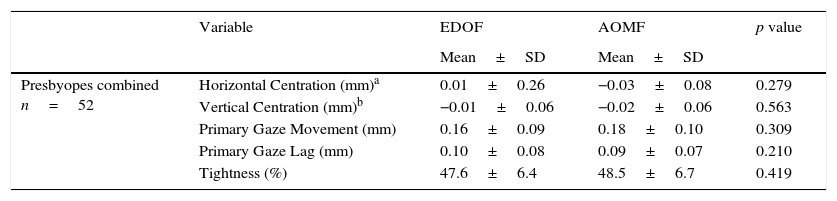
Lens fittingLens fitting results are given in Table 6. There were no significant difference between lens types for centration, primary gaze movement, primary gaze lag or tightness (p≥0.210).
Lens fitting parameters for EDOF and AOMF lenses for all presbyopes combined.
| Variable | EDOF | AOMF | p value | |
|---|---|---|---|---|
| Mean±SD | Mean±SD | |||
| Presbyopes combined n=52 | Horizontal Centration (mm)a | 0.01±0.26 | −0.03±0.08 | 0.279 |
| Vertical Centration (mm)b | −0.01±0.06 | −0.02±0.06 | 0.563 | |
| Primary Gaze Movement (mm) | 0.16±0.09 | 0.18±0.10 | 0.309 | |
| Primary Gaze Lag (mm) | 0.10±0.08 | 0.09±0.07 | 0.210 | |
| Tightness (%) | 47.6±6.4 | 48.5±6.7 | 0.419 |
EDOF, extended depth of focus; AOMF, AIR OPTIX aqua Multifocal.
A previous short-term study by our research group reported EDOF lenses demonstrate better intermediate and near visual performance with no significant difference at distance compared to a commercially-available, non-monotonic, zonal-refractive multifocal.22 The present study indicates similar findings with EDOF lenses showing better intermediate and near vision performance and similar distance vision when compared to a center-near design multifocal (AOMF). Similar to our previous study,22 possible confounders to multifocal performance including pupil size,10 illumination levels10 and lens fitting15,26 were minimized by the cross-over design, controlled illumination levels and no significance difference between lens types for any lens fitting parameters. The non-significant interaction for HCVA, clarity-of-vision and lack-of-ghosting between lens types and strata suggests inferences with the total sample size are also applicable to the low and medium-high presbyopia strata.
The objective results with AOMF concur with other studies assessing center-near lenses for HCVA,12,16–21 LCVA,18,21 and CS12,16,17,19 at 6m and stereopsis at 40cm.17,18,20 However, many of these studies also reported better results with AOMF for HCVA at 40cm.12,17–21 Our previous study also reported worse HCVA at 40cm with the commercially-available control lens compared to other studies using the same lens,22 and appears to result from the comfort-based, reading assessment (“comfortable visual acuity” rather than conventional resolution acuity) chosen to measure near acuity. Comfortable visual acuity measurements tends to push acuities toward 0.50logMAR,22 which is the paragraph size where maximum reading speed is achieved.27 Regardless, the current and previous study22 suggests comfortable visual acuities can discriminate between lenses for HCVA at 40cm, albeit at the expense of inter-study comparison. The current study also confirms reading-based HCVA can be improved by around 0.2logMAR (two paragraphs) with a reading distance of 50cm compared to 40cm, irrespective of CLs worn.22
Objective and subjective measures showed similar findings at distance and near: EDOF and AOMF were comparable for distance vision performance while EDOF was significantly better for near vision performance (HCVA and stereopsis at 40cm, and clarity-of-vision at near). The significantly better near stereopsis with EDOF may have been influenced by the significantly better HCVA,28 and may also indicate less binocular disruption17 compared to AOMF.
At intermediate, the objective measure (HCVA at 70cm) showed no significant difference while the subjective measure (clarity-of-vision at intermediate) was significantly better with EDOF. However, subjective measures are more sensitive indicators of multifocal vision performance29 suggesting EDOF was also significantly better than AOMF for intermediate vision performance.
These clinical findings concur with theoretical Fourier optics simulations, which indicates that manipulation of multiple modes of spherical aberration terms offers significantly greater extension in depth-of-focus than when just using single mode of spherical aberration term.30
Subjective measures of clarity-of-vision at intermediate and near and overall vision satisfaction were not only significantly better with EDOF, but the mean differences in ratings (0.8–1.1 units) suggest they were also clinically significant.31 The proportion of participants who rated clarity of vision≥8 units for all three testing distances and overall vision satisfaction≥8 units was also significantly higher with EDOF compared to AOMF. EDOF lenses were also rated as having less overall ghosting than AOMF.
Three of the reported limitations of center-near design multifocals include decreased quality of vision,1,12,13 contrast sensitivity,13,14 and increased ghosting.13,15 The results of this study suggest EDOF show reduction in two of these limitations compared to a center-near lens.
Lens purchase was also significantly better with EDOF lenses. However, lens purchase can be strongly influenced by ocular comfort,32–34 and so the results may have been confounded by the significantly better ocular comfort reported with EDOF. The most likely cause of comfort disparity in this study is material modulus (poly-HEMA-based 0.4MPa vs. lotrafilcon B 1.0MPa). High modulus materials require an adaptation period to improve comfort35 but participants in the current study only wore CLs for about 1h before rating comfort. Participants also wore CLs for 1h before rating comfort in our previous study,22 but the control lens had a lower modulus (senofilcon A, 0.72MPa35) than lotrafilcon B and there was no significant difference between lens types for comfort.22 Despite this non-significance, lens purchase was still significantly better with EDOF and was likely due to visual factors as indicated by the significantly better clarity-of-vision at intermediate and near and overall vision satisfaction,22 as was found in the present study. The effect of comfort was also mitigated by participants being instructed specifically to base lens purchase on their visual experience only. It therefore seems probable that visual factors rather than comfort were the main determinants of lens purchase in this study.
There were some limitations with this study. Even though over-refraction was necessary, a trial frame and trial lenses can adversely affect subjective visual performance and over-refraction power can influence results.22 However, subjective results with EDOF were either better than or not-significantly different to AOMF, despite significantly more participants requiring a trial frame with lens with EDOF. The significantly more minus over-refraction with EDOF and magnitude of difference (0.011D) in over-refraction between lens types were expected given the differences in lens power increments available and criteria for choosing lens power,22 indicating over-refraction achieved its intended purpose of optically equalizing lens types so that lens design differences alone were compared. Therefore, use of a trial frame and over-refraction do not appear to have been detrimental to the results of this study.
Investigators were not masked to lens identity, and so objective measurements could be perceived as biased. However, subjective measurements are unaffected as participants were masked to lens identity and subjective measurements were directly entered into a database by participants independently of the investigator. Since subjective measures are more sensitive than objective measures for assessing multifocal lens performance29 the non-masking of investigators does not appear to have affected the overall findings of this study.
The sample size of 19 and 10 in the medium and high add strata, respectively were inadequate to allow for statistical analysis of subjective measurements and so were combined into one medium-high stratum. Repeated measures ANOVA found no significant interaction between the low and medium-high strata, but a significant difference might have been found between the low, medium and high strata with a sample size of 20 in each strata. Though the medium and high strata did not have the minimum sample of 20 participants, the distribution of low, medium and high add strata (44%, 37% and 19% respectively) is probably closer to the CL wearing population than an equal proportion between the three strata. Moreover, it was observed that within each medium and high strata, EDOF performed better than AOMF by ≥1 unit for overall vision satisfaction and ≥0.5 units for clarity-of-vision at intermediate and near. This would indicate visual experiences within these two strata were not dissimilar.
This was a short term study, and so may not be predictive of longer-term performance.29 All measurements were performed under photopic conditions, and good visual performance has been reported with center-near lenses under mesopic conditions.12,16
Longer-term studies, with a full range of lens powers conducted under a range of visual and lighting conditions should address most of the limitations of this study.
ConclusionThis study demonstrates the prototype lenses, designed by deliberate manipulation of multiple higher-order spherical aberration terms, result in better intermediate and near vision performance in presbyopes with no difference in distance vision compared to a commercially-available center-near multifocal during short-term wear. Longer term studies are required to fully evaluate the clinical utility of EDOF lenses.
FundingThis project is entirely funded by the Brien Holden Vision Institute.
Conflicts of interestThe Institute has proprietary interests in the intellectual property governing EDOF lenses (Patent application number WO2014059465 A1). The Institute receives royalties from the sale of AOMF contact lenses.
The authors would like to acknowledge the clinical team (Ms. J. Diec, Ms. E. Robertson and Ms. R. Crompton) and the database management team (Dr. T. Naduvilath and Ms. K. Laarakkers) for their invaluable support to run the study at the CRTC, Brien Holden Vision Institute, Sydney, Australia. Authors would like to extend their thanks to Dr. J. Flanagan for reviewing the manuscript. The authors would also like to acknowledge the late Prof. Brien Holden, whose inspirational leadership and foresight made this project possible.