To determine the prevalence of refractive errors in Jewish and Arab college students in Israel and associations with ethnicity and sex.
MethodsIn this retrospective cross-sectional study, first-year college students underwent non-cycloplegic autorefraction and answered a questionnaire to assess age, sex, and self-identified ethnicity. Spherical equivalent refractive error (SER) was calculated, and the prevalence of hyperopia (>+0.50 Diopter, D), emmetropia (>-0.50 to +0.50 D), myopia (≤-0.50D, low ≤-0.50 to >-3.0D, moderate <-3.0 to >-6.0D, high ≤-6.0D), and astigmatism (>0.50D) were determined. Groups were compared using Chi-square or Fisher test. Univariate and multivariate analyses were conducted to identify factors associated with refractive errors.
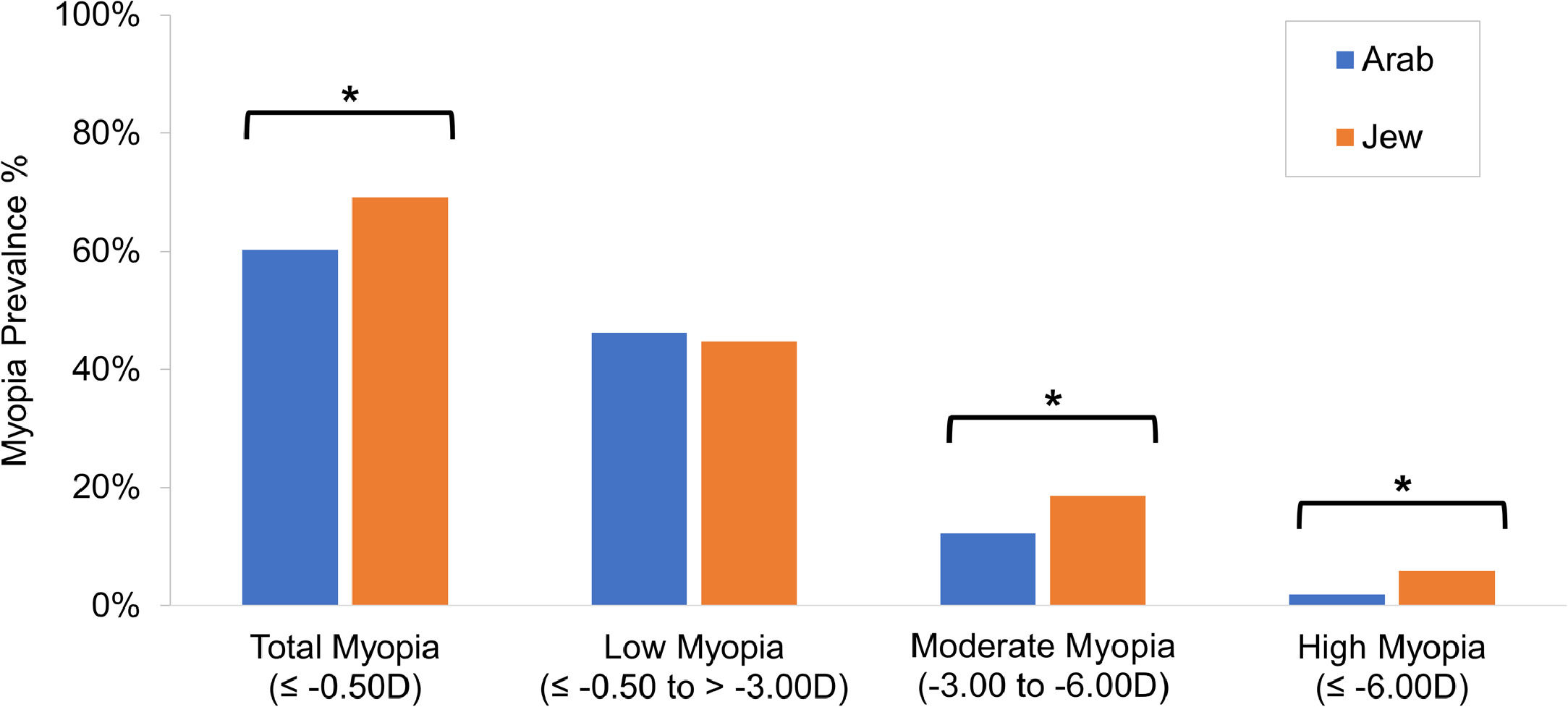
ResultsParticipants (n = 807) had a mean age of 22.1 ± 2.6 years (range: 17–30 years) and SER of -1.7 ± 2.2D (range: -13.3 to +5.7D). The prevalence and 95% confidence internal of myopia was 66.3% (63.0–69.6). Jewish students had a higher prevalence than Arab students for myopia (69.2% vs 60.3%), moderate (18.5% vs 12.2%) and high myopia (5.9% vs 1.9%) and astigmatism (51.4% vs 43.9%, p<0.05 for all), but not low myopia or hyperopia. Females had a higher prevalence of myopia than males (68.1% vs 58.7%, p<0.03). Jewish ethnicity was associated with myopia (OR=1.48, p = 0.01) and moderate myopia (OR=1.72, p = 0.01), and studying optometry was associated with moderate myopia (OR=1.63, p = 0.02). Sex and age were not associated with myopia.
ConclusionMyopia prevalence in Israeli college students is high, showing associations with Jewish, but not Arab, ethnicity, suggesting that ethnic factors may play a role in the refractive differences between Arabs and Jews.
Uncorrected refractive error is a major cause of mild to severe vision impairment, globally.1 Myopia is the most prevalent refractive error, with a growing prevalence in Israel, Eastern Asian countries, the United States, and other non-Asian countries.2–5 The prevalence of high myopia is also growing6 and there are predictions that by 2050, approximately 50% of the world population will be myopic.3
Myopia is associated with retinal detachment, macular degeneration, cataract, and glaucoma.7 Understanding the causative factors underlying the increasing prevalence of myopia may enable the development of treatments and reduce the potentially blinding complications and socio-economic impact associated with myopia.8 Refractive development is regulated by a complex interaction between genetic, environmental, and behavioral factors.9,10 Risk factors for myopia include parental myopia11,8 and high amounts of near work,12,13 while accumulating evidence suggests that outdoor time is protective against myopia.14–17
In Israel, level of education has been linked to myopia and is considered a proxy for near work.18–21 Studies in college students in other parts of the world support this notion, since college students have been shown to have a higher prevalence of myopia22,23 than the general population in the same geographic area.24,25 This may be due to behavioral factors; college student populations are characterized by high academic achievement during school years, which often correlates with prolonged near work and less leisure time outdoors.
Most studies on myopia in college students follow ethnically homogenous cohorts, which limits the generalization of the results. The term ethnicity refers to communality in cultural heritage, language, social practice, traditions, and geopolitical factors.26 Ethnicity includes health factors such as lifestyle, diet, and values.27 Although ethnic differences in the prevalence of myopia have been examined previously,28–30 the exact role that ethnicity plays in the development and progression of myopia remains elusive. Some studies have compared the prevalence of myopia across different geographic regions to assess ethnic differences.31 However, this approach generates questions around confounding variables since different countries and cultures bring with them differences in risk factors other than ethnicity. A comparison of two ethnicities in the same geographic region and with similar educational background could elucidate the etiology of myopia. A similar prevalence of myopia would suggest a contribution of educational background and a different prevalence of myopia a contribution of ethnicity.
Previous studies in Israel compared the prevalence of myopia in Jewish children from different backgrounds,19 in Jewish 17-year-old pre-army recruits,21,32–34 and in Arab and Jewish first and eight grade children.35,36 The results show that in Jewish pre-army recruits, women have a higher prevalence of myopia than men,32–34 and ultra-Orthodox men have a higher prevalence of myopia than secular men.21 Furthermore, Jewish eighth grade children have a higher prevalence of myopia than Arab eighth grade children.35,36 Thus far, there are no published studies regarding the prevalence of refractive errors in adults in Israel.
The purpose of the current study was to determine the prevalence of refractive errors in college students in Israel and to compare the prevalence in two ethnically distinct groups, Jews and Arabs who reside in the same geographic location and have similar educational background. This comparison will allow us to test the contribution of ethnicity to myopia and refractive error prevalence.
Material and methodsParticipantsThis cross-sectional retrospective study was approved by the Hadassah Academic College (HAC) Ethics Committee. Informed consent was obtained and the privacy rights of the subjects was observed. From 2011 to 2020 all first-year Department of Optometry students at HAC in Jerusalem, Israel, were invited to participate in a free vision screening program run by the Department of Optometry during orientation week. In 2011 and 2014, students from several other academic departments were invited, as well, and were categorized in analyses as non-optometry. The purpose of vision screening was to identify vision problems in first year students so as to correct them before they interfered with learning. The data from the screening program was used as part of several research studies,37,38 each having the received approval of the HAC Ethics Committee including informed consent. Students were recruited via the HAC email. Additionally, a researcher visited each intake's initial orientation meeting to invite them to vision screening and explain the importance of vision for learning. Students with a history of ocular surgery or known ocular pathology were not invited to participate in screening but were referred for a full ocular exam. Thus, their follow-up data were not available. There were very few students above age 30 years, and therefore, these participants were not included.
HAC is a public institution with government subsidized tuition located in Downtown Jerusalem. All students at HAC have similar academic background. Admission is open to all candidates who have full high school matriculation and a psychometric exam result with an appropriate score. Israeli public high schools offer a standardized curriculum in Hebrew or Arabic. Usually, Jewish teenagers study at schools in which the language of instruction is Hebrew and Arab teenagers at schools in which the language of instruction is Arabic. Most students at HAC attended an Israeli public school. Ultra-Orthodox Jews have a private school system for boys which does not offer full matriculation, thus they do not have the background required for admission to HAC. Therefore, this study included Arab and Jewish students with a similar high school background, and did not include ultra-Orthodox Jewish men.
Screening protocolThe screening tests included distance visual acuity, measured at 6.0 m using a Snellen chart. Non-cycloplegic refraction was measured using a Hartmann-Shack based auto-refractometer (Luneau, France, either the L80 or a newer version of the instrument, VX120). Both instruments use the same aberrometry based auto-refraction technique and differ only in that the VX120 has an additional Scheimpflug camera. The instruments were previously validated to subjective refraction and found to have good intersession and intrasession repeatability.38–42 The instruments were not significantly different than subjective refraction, with a mean difference for spherical equivalence of 0.06 ± 0.44 D and 0.14 ± 0.47 D, for the L8037 and VX120,36 respectively. The instruments were calibrated before each vision screening. These automatic devices require minimal examiner skill. Hence, a change in examiner is unlikely to be the source of any significant precision error,43 and high repeatability was found in studies where different examiners were used.38,42 Students completed a questionnaire regarding age, sex (male or female), and academic department. The questionnaire had a closed question asking which ethnicity they identified with more: Arab or Jew.
AnalysisParticipants were classified into refractive error groups based on non-cycloplegic auto-refraction. The International Myopia Institute (IMI) has the following classifications of myopia when accommodation is relaxed (using cycloplegia in non-presbyopic patients): myopia is defined as spherical equivalent (SER) ≤−0.50 D; low myopia SER ≤−0.50 to > −6.00 D; high myopia ≤−6.00 D.44 Since cycloplegic refraction is not usually part of a screening protocol, most previous studies in Israel21,32–34 and many around the world in university students23,45–47 also used non-cycloplegic refraction. The most recent study in Israel of older adolescents used non-cycloplegic refraction and the IMI definitions but with two differences: low myopia was categorized as SER ≤−0.50 to > −3.00 D and an additional category of moderate myopia was defined as SER ≤ −3.00 to > −6.00 D.21 Thus, to be consistent with the IMI and to compare with similar studies in Israel and abroad, refractive errors were defined as follows: Myopia as SER ≤−0.50 D, low myopia as SER ≤−0.50 D to > −3.00 D, moderate myopia as SER of −3.00 D to > −6.00 D, and high myopia as SER ≤−6.00 D.
Hyperopia was defined as SER >+0.50 D45 and astigmatism as a cylinder power greater than 0.50 D.45 High astigmatism was defined as a magnitude equal to or greater than 3.0 D.48
The main outcome of the study was the prevalence of myopia. Thus, the sample size was calculated using WinPepi software49 based on the ability to detect the prevalence of myopia, which was set at 45% in college students based on previous studies.22,45 Assuming a power of 0.92, a sample size of 149 was estimated, and assuming a power of 0.95, a sample size of 381 was estimated. Therefore, this study was sufficiently powered to detect myopia in the entire cohort and in each subgroup.
Prevalence and 95% confidence interval (CI) were calculated for each refractive error group. Prevalence of myopia (total, low, moderate, and high), hyperopia, and astigmatism were compared for sex (men vs women), self-identified ethnicity (Arabs vs Jews), and department (optometry vs non-optometry) using chi-squared test, Odds Ratio (OR) and 95% Confidence Intervals (CI). The data were not normally distributed (tested by Shapiro-Wilk Test), so the Mann-Whitney test was used for continuous variables (age, SER and astigmatism). Univariate and multivariate logistic regressions were applied to determine factors affecting different refractive errors (age, sex, ethnicity, and academic department). The results of the regression models were reported as odds ratios (ORs) with 95% CIs. The level of significance was set at 0.05. All analyses were conducted using SPSS, version 25.0 (IBM Corp). Since the refractive error is highly correlated between the right and left eye,50 only data from the right eye of each subject were used.
ResultsVision screening was offered to 1139 (637 optometry and 502 non-optometry) students and 822 participated, giving a response rate of 72% (78% and 65%, for optometry and non-optometry, respectively). Fifteen students did not meet the inclusion criteria due to age. Thus, 807 subjects were included in this study. Population demographics are presented in Table 1. The mean age of the study population was 22.1 ± 2.6 years (range 17–30 years); 652 (68.1%) were female and 155 were (31.9%) male. In terms of ethnicity 545 (69.2%) self-identified as Jewish and 262 (30.8%) self-identified as Arab. The majority of the students were in the Department of Optometry (498; 68.3%), and the remaining studied in other academic departments (309; 31.7%). The women were significantly younger than the men (p<0.0001), the Arab students were significantly younger than the Jewish students (p<0.0001), and the optometry students were significantly younger than students in other departments (p<0.0001). A significantly more myopic SER was found in women vs. men (p = 0.001), Jews vs. Arabs (p<0.0001), and optometry vs. non-optometry students (p = 0.006 and p = 0.002, respectively).
Participant demographic and refractive data.
Abbreviations: D, Diopter. *significant difference<0.05.
The prevalence of refractive errors by sex, ethnicity, and academic department is shown in Table 2. Emmetropia was found in 29.7% (240) of students (95% CI 28.2–31.2%), while the remaining students were found to have a refractive error. The most common refractive error was myopia (66.3%; 95% CI 63.1–69.6), followed by astigmatism (48.9%; 95% CI 46.5–51.4%) and hyperopia (4.0%; 95% CI 3.8%−4.2%). Of the participants with astigmatism, 92 had simple astigmatism with no significant spherical component, and nine had an astigmatic power greater than 3 D, which is classified as high astigmatism.48
Prevalence of refractive errors by sex, self-reported ethnicity, and academic department in Israeli college students.
| N | Myopia (≤−0.50D) | Low Myopia (≤−0.50 to >−3.00D) | Moderate myopia (−3.00D to >−6.00D) | High myopia (≤−6.00D) | Hyperopia (>+0.50D) | |
|---|---|---|---|---|---|---|
| Total N,% (95% CI) | 807 | 535 | 365 | 133 | 37 | 32 |
| 66.3% | 45.2% | 16.5% | 4.6% | 4.0% | ||
| (63.0–69.6%) | (43.0–47.5%) | (15.7–17.3%) | (4.4–4.8%) | (3.8–4.2%) | ||
| Sex | ||||||
| Male N% (95% CI) | 155 | 91 | 63 | 24 | 4 | 6 |
| 58.7% | 40.6% | 15.5% | 2.6% | 3.9% | ||
| (55.8–61.6%) | (38.6–42.7%) | (14.7–16.3%) | (2.5–2.7%) | (3.7–4.1%) | ||
| Female N,% (95% CI) | 652 | 444 | 302 | 105 | 33 | 26 |
| 68.1% | 46.3% | 16.7% | 5.1% | 4.0% | ||
| (64.7–71.5%) | (44.0–48.6%) | (15.9–17.6%) | (4.8–5.3%) | (3.8–4.2%) | ||
| PChi square | 0.03* | 0.20 | 0.71 | 0.28£ | 1.00 | |
| OR (95% CI) | 1.50 (1.05–2.15) | 1.26 (0.88–1.80) | 1.10 (0.68–1.77) | 2.01 (0.70–5.77) | 1.03 (0.42–2.55) | |
| Self-reported Ethnicity | ||||||
| Arab N,% (95% CI) | 262 | 158 | 121 | 32 | 5 | 13 |
| 60.3% | 46.2% | 12.2% | 1.9% | 5.0% | ||
| (57.3–63.3%) | (43.9–48.5%) | (11.6–12.8%) | (1.8–2.0%) | (4.7–5.2%) | ||
| Jew N,% (95% CI) | 545 | 377 | 244 | 101 | 32 | 19 |
| 69.2% | 44.8% | 18.5% | 5.9% | 3.5% | ||
| (65.7–72.6%) | (42.5–47.0%) | (17.6–19.5%) | (5.6–6.2%) | (3.3–3.7%) | ||
| PChi square | 0.01* | 0.71 | 0.02* | 0.01£* | 0.31 | |
| OR (95% CI) | 1.48 (1.09–2.01) | 0.95 (0.70–1.27) | 1.64 (1.07–2.51) | 3.21 (1.24–8.33) | 0.69 (0.34–1.42) | |
| Academic Department | ||||||
| Optometry N,% (CI 95%) | 498 | 340 | 218 | 93 | 29 | 23 |
| 68.3% | 43.8% | 18.7% | 5.8% | 4.6% | ||
| (64.9–71.7%) | (41.6–46.0%) | (17.7–19.6%) | (5.5–6.1%) | (4.4–4.8%) | ||
| Other N,% (95% CI) | 309 | 195 | 147 | 40 | 8 | 9 |
| 63.1% | 47.6% | 12.9% | 2.6% | 2.9% | ||
| (60.0–66.3%) | (45.2–50.0%) | (12.3–13.6%) | (2.5–2.7%) | (2.8–3.1%) | ||
| PChi square | 0.13 | 0.29 | 0.03* | 0.03* | 0.23 | |
| OR (95% CI) | 1.26 (0.93–1.70) | 0.86 (0.65–1.14) | 1.54 (1.03–2.31) | 2.33 (1.05–5.16) | 1.61 (0.74–3.54) |
Jews had significantly more of the following myopia categories and astigmatism than Arabs (Fig. 1): myopia (69.2% vs 60.3%, p = 0.02), moderate myopia (18.5% vs 12.2%, p = 0.03), high myopia (5.9% vs 1.9%, p = 0.01), and astigmatism (51.4% vs 43.9%, p = 0.05). No differences were observed between Jews and Arabs for low myopia (46.2% vs 44.8%, p = 0.71) and hyperopia (5.0% vs 3.5%, p = 0.31). Women had significantly more myopia than men (68.1% vs 58.7%, p = 0.03), but no difference was observed for all other refractive errors (p>0.2 for all comparisons).
To test whether students attracted to study optometry were more likely to have refractive errors than other students, the prevalence was calculated for each department category separately (Table 2). Optometry students had significantly more moderate and high myopia than all other students (18.7% vs 12.9%, p = 0.03 and 5.8% vs 2.6%, p = 0.03, respectively), although no differences were observed for myopia and low myopia, astigmatism, and hyperopia (p>0.13 for all comparisons).
Table 3 presents the results of univariate analysis on the relationship between refractive errors and independent predictors, including age, sex, ethnicity, and academic department. This analysis was not performed on high myopia and hyperopia since these groups had less than 30 subjects. None of the refractive errors were associated with age or sex. However, myopia and moderate myopia were associated with Jewish ethnicity. Only moderate myopia was associated with academic department. Using multivariate logistic regression analysis, the adjusted odds ratios were determined as a measure of association between refractive errors and the independent predictors, which had been found significantly different in the univariate analysis. The independent predictors which were found to be significantly associated with refractive errors were ethnicity for myopia ≤−0.50 (OR 1.48 (95% CI 1.09–2.01); p<0.01) and moderate myopia (OR 1.72 (1.12–2.65); p<0.01) and academic department for moderate myopia (OR 1.63 (95% CI 1.09–2.44); p = 0.02).
Univariate analysis of association of age, sex, self-reported ethnicity and academic department with refractive errors.
Abbreviations: ref, reference; OR, odds ratio, CI, confidence intervals. *significant difference<0.05.
While previous studies determined the prevalence of myopia in Jewish teenagers21,32–34 and children35 this is the first study to quantify the prevalence of refractive errors in adult college students in Israel. Results showed an overall prevalence of myopia (as defined as ≤−0.50D SER) to be 66%. Self-identified Jews had significantly more myopia as well as moderate and high myopia and astigmatism than self-identified Arabs. Additionally, women had significantly more myopia than men. Myopia and moderate myopia were associated with self-reported ethnicity in multivariate analysis. Thus, the results of the current study demonstrate that Jews are at a higher risk for myopia than Arabs. Similarly, in Israeli eighth grade students, a significantly higher prevalence of myopia was found in Jewish children (26.8%) in comparison to Arab children (11.8%).35 The sample size in the current study was not sufficient to determine the factors associated with high myopia in the multivariate model, so this remains an open question.
While age differed significantly between the groups, age was not associated with refractive error in the univariate analyses. This is not unexpected, as all the subjects were adults in the narrow age range from 18 to 30 years. Studies show that myopia incidence, prevalence, and progression are associated with age,5 but most of the change happens before age 18 years.51 Thus, due to the narrow range, age was not a factor in the current study.
The prevalence of myopia of 66% in Israeli college students found here is much higher than that found in previous studies of 17-year-old adolescent Israeli army recruits, which ranged from 28% to 37.8%.21,32,33 As in the current study, these previous studies used non-cycloplegic autorefraction and the same or similar definition of myopia, so the results can be compared. The different rates of myopia may be due college students having different educational backgrounds than the general population; while all Jewish Israeli citizens must report for recruitment to the army, only those who have a specific interest in higher education and full matriculation enroll in university. Only 70% of high school students in Israel complete full high school matriculation. The association between education and myopia has been shown at a number of levels.52 There is also evidence for causality: a Mendelian randomization study suggests that higher academic achievement causes myopia, and not that myopic children are more likely to excel in school.53
The difference in prevalence between college students in this study and the study of army recruits21 is not likely due to age. The college students were all adults with an average age of 22 and thus older than the army recruits who were on average 17 years-old. However, most axial elongation occurs before the age of 18, making the difference in axial growth between these age groups minute and without implications in terms of refractive error.51
The association between myopia and education in Israel is further supported by a study in army recruits that found a correlation between myopia and years of education32 and between myopia and educational system. Bez, et al21 found that the odds of having myopia for those who were studying in the ultra-Orthodox and Orthodox educational systems were higher than those studying in the secular educational system. The findings suggest that educational systems requiring extensive reading and other near-work activities are associated with increased prevalence and severity of myopia.
The different rates of myopia found in Arabs and Jews with a similar educational background in this study provide insight regarding the pathogenesis of myopia. The previously reported difference in the prevalence of myopia in Jewish and Arab eighth graders (26.8% vs 11.8%),35 is much greater than the differences in the current study (60.3% vs. 69.2%). The study in Israeli eighth graders included all children registered in school, despite their academic performance.35 In contrast, the current study included only a cohort of students with the high academic achievement required for college admission. This suggests that educational history, is a major contribution to myopia. However, if myopia were only a function of school related near work history, we would expect Arab and Jewish college students to have the same prevalence of myopia. The fact that there are differences suggests that ethnic factors also contribute to the pathogenesis of myopia. Jews and Israeli Arabs have been shown to be genetically distinct,54 and perhaps these genetic differences contribute to the disparate rates of myopia. However, genetic variability is only one of many biological mechanisms that can explain differences between ethnicities. For example, the ethnic differences observed in cardiometabolic health can be explained by life history, microbiome, behavior, social environment, education values, and beliefs.27 It is possible that some aspect of ethnicity explains the differences between self-categorized Jews and Arabs in this study as well.
The notion that shared academic history is strongly associated with myopia is supported by comparing the results with other studies of the prevalence of myopia in Arabs, which used protocols similar to the current study. The prevalence of myopia and high myopia found in Arab students in Israel is similar to that found in Arab students in Saudi Arabia.22 This suggests that an ethnic group with similar educational backgrounds will develop similar rates of myopia. In contrast, a study on refractive errors in an academically heterogenous cohort of adults in Jordan, using a similar definition of myopia (non-clycloplegic) as the current study,55 found a lower prevalence (54%) than the current study (60%), further supporting the role of education in the development of myopia.
Geographic location is not likely to explain the differences between Jews and Arabs in this study. Israel is a small country and Jews and Arabs live in distinct but adjacent neighborhoods in the same cities and in neighboring towns. Over 99% of Israelis live in urban settings.56 While urban vs. rural living has been thought to increase the risk of myopia, this would not explain the differences found in Arab and Jewish students in the current study.57,58
The significantly higher prevalence of myopia in women than in men found in the current study has also been reported previously in adolescent Israeli army recruits.32–34 Sex differences in the prevalence of myopia in whites and East Asians, emerge at about nine years of age and become more marked through adolescence, showing double the odds of myopia in girls compared with boys.58 These differences have been attributed to a stronger emphasis on education and near distance-related activities in girls compared with boys.59 This sex difference has been observed previously in some studies of college students,22,46,47 but not in others.23 This suggests that despite men and women in college having similar school background, near work and outdoor behavior differ between the sexes; girls and young women may spend more time performing near work and less time outdoors.
The prevalence of myopia in college and university students has been widely studied and is known to vary with geography. Studies in Asian countries found a prevalence of myopia as high as 96% in Taiwan60 and 92% in China.47 In the United States, law students had a prevalence of 66%23 and in Norway first year engineering students had a prevalence of 47%.61 In Iran, 43% of the students were myopic45 and in Saudi Arabia, 48% were myopic.22 Some of the variance may be due to different definitions of myopia. However, the studies in China, Saudi Arabia, Taiwan, and Iran used the same definition as in the current study (non-cycloplegia) yet exhibited different rates of myopia than the current study (66%). The differences may be due to cultural and behavioral, as well as genetic, differences.
The prevalence of astigmatism found in Israeli college students (49%) is higher than that found in college students in Iran (29%).45 A literature review and meta-analysis of the global prevalence of refractive errors2 found that about 15% of children and 40% of adults had astigmatism, but with large variations. In the Middle East, the prevalence of astigmatism was 24% in people above age 15.62 The reason for the high prevalence of astigmatism is unclear and warrants further research. This may be due to genetic or environmental differences.
The prevalence of hyperopia in this study (4%) is similar to that found in college students in Saudi Arabia (6.5%)22 and Iran (3.8%).45 However, studies in college students have a much lower prevalence of hyperopia than the general population the Middle East in people over age 15 (21%).62 The greater amount of near work and less time outdoors in highly educated people may cause a myopic shift, reducing the prevalence of hyperopia.
The current study does present some limitations. The cohort in this study does not reflect the general population in Israel, rather a highly educated subset of the population. Thus, the prevalence of myopia in the general population is likely to be different. However, the students admitted to the college had a very similar educational history. Therefore, we can make conclusions regarding Arabs vs. Jews and men vs. women.
Another limitation is that refractive errors were measured without cycloplegia, despite the classification of myopia by the International Myopia Institute as ≤−0.50 D spherical equivalent in the absence of accommodation.44 The motivation for not using cycloplegia was three-fold. First, this was a large cross-sectional prevalence study involving assessment of a large number of participants in a short time. It is beyond the scope for many researchers to perform cycloplegic refraction in this format. Second, all previous studies in Israel that included a similar age group (adolescents) also used non-cycloplegic refraction.21,32–34 Third, the only research on the prevalence of refractive errors in university students in the Middle East used non-cycloplegic refraction.22,45 Thus to compare our results with previous research we used non-cylcoplegic refraction. The use of non-cycloplegic refraction could have resulted in the overestimation of the prevalence of myopia and underestimation of the prevalence of hyperopia.63 However, this limitation is true for all the subjects that participated and thus would not affect comparison of Arab and Jewish students or men and women.
The definition of myopia used in this study was based on spherical equivalent, as suggested by the IMI guidelines.44 A critique of these guidelines is that it may include people with mixed astigmatism that have a hyperopic principle meridian. Thus, it has been suggested that myopia be classified as including spherical myopic errors as well as simple or compound myopic astigmatism, excluding mixed astigmatism.64 The current study did not use this classification system so as to compare to previous studies.
The results of this study may suffer from self-selection biases. It may be that students attracted to study optometry are more likely to have refractive errors than other students. Indeed, optometry students have a higher prevalence of moderate and high myopia than students in other departments in our study. However, Jewish and Arab students, and men and women, were equally represented in both optometry and non-optometry departments. Additionally, students with vision-related issues may have been more likely to participate in the screening process, especially if they were not optometry students. Indeed, compliance was higher (78%) for optometry students than for non-optometry students (65%). Since we did not collect data regarding visual complaints and/or visual acuity, this bias cannot be ruled out.
Data were not collected regarding subjects’ family history of myopia or exposure to risk factors. Future studies could implement methodology that would include questions about parental refractive status to assess the contribution of heredity to refractive error. High school grade point average and psychometric exam results would be of interest to evaluate the relationship between academic success and myopia. Additional questions regarding near work, use of electronic devices, physical activity, and time outdoors would be relevant to understand the role of behavioral factors to myopia.
ConclusionIn conclusion, this study demonstrates that Jewish university students in Israel have a higher prevalence of myopia than Arab university students, and women have a higher prevalence of myopia than men. Jewish ethnicity emerged as a risk factor in the multivariate model. Because Jewish and Arab college students share a common educational background, these findings suggest that ethnicity plays a role in refractive error development in Israeli young adults. However, the difference in the prevalence of myopia between Arab and Jewish college students is relatively small and suggests that educational history has a role in myopia.
We would like to thank the students and faculty of Hadassah Academic College Dept. of Optometry who ran the vision screening program. This work was supported by the Binational Science Foundation (Grant #2019053, 2020).