This pilot study aimed to investigate the maximum extension of foveal fixation in the horizontal direction among young adults in both emmetropes and myopes.
Methods35 participants (28 emmetropes and 7 myopes) were included. Participants with restricted extra-ocular mobility, end gaze nystagmus, and/or any other ocular pathology were excluded. Visual acuity (VA) was used as a surrogate measure of foveal fixation. VA was determined using a staircase procedure with 8 reversals. The average of the last 5 reversals was taken as the thresholds. VA acuity was measured at different gaze eccentricities along nasal and temporal visual field meridian. The eccentricity at which VA drops significantly was taken as the maximum extent of foveal fixation. A bilinear fit regression model was used to investigate the drop in the VA in both nasal and the temporal direction.
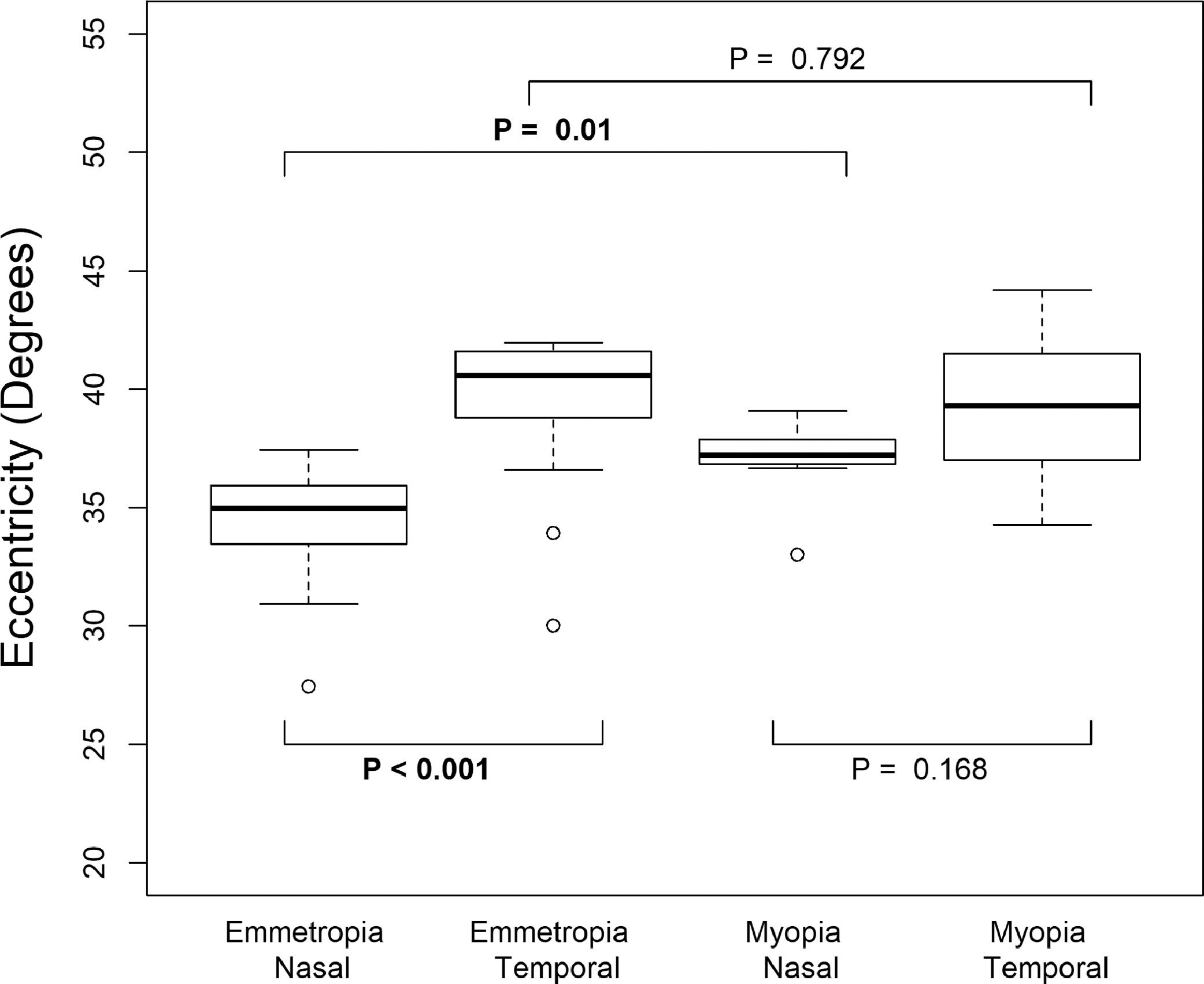
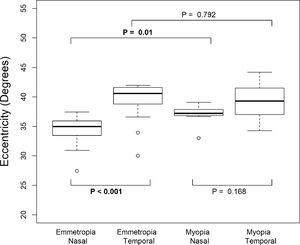
ResultsEmmetropes can foveate up to 35 ± 2° in nasal and 40 ± 3° in temporal direction and myopes can foveate up to 38° in both nasal and temporal directions. Paired student t-test showed a significant difference in foveal fixation between nasal and temporal direction for emmetropes (P<0.001) but not in myopes (P = 0.168). An unpaired student t-test showed a significant difference in foveal fixation for nasal direction between myopes and emmetropes (P = 0.01). However, no statistically significant difference was found in foveal fixation for temporal direction between myopes and emmetropes (P = 0.792).
ConclusionThe eye rotation does not necessarily match with the extent of foveal fixation at extreme eye rotation. Eyes can fixate only up to 35° nasally and 40° temporally maintaing their maximum visual acuity.
Sharp central vision (also known as foveal vision) in the human eye is achieved by maintaining the image in the central portion of the eye called the fovea where photoreceptors are densely packed. The fovea is a specialized retinal region with highly developed visual resolution and provides maximum visual acuity. Even at 1° away from the fovea, visual acuity was reported to drop off dramatically up to 60%1 which is equivalent to 2 lines drop in logMAR acuity.
When the objects appear in the peripheral visual field, a head turn, eye turn or a combination of both is necessary to maintain a sharp central vision. Monocular eye movements (ductions) are achieved with the help of six extraocular muscles. A normal healthy individual aged between 20–40 can rotate their eye up to 47° nasally and 46° temporally2 and the maximum ability to rotate the eye tend to decrease with increasing age.3
Although many studies have reported the extent of eye rotation,2–7 there is very limited literature on what extent eyes can foveate an object (henceforth referred to as foveation) by keeping the head stationary in a primary and fixed position. Shechtman et al.8 measured the extent of foveation with the head fixed in primary position have shown the extend of foveation varies from 55 to 58° and 45–48° in abduction and adduction, respectively in young adults. However, the target used in Shechtman et al. was not a “threshold target”. They used one line above the best corrected near vision target to examine the foveation at extreme gazes. As aforementioned, considering that even a 1° away from fovea the visual acuity drops dramatically, using a suprathreshold target i.e., one line above near visual acuity target could have overestimated the extent of foveation.
The extend of foveation should be different from eye rotation because eye rotation was measured from the center of the pupil i.e., from the pupillary axis whereas foveation was measured through the visual axis. The visual axis is offset from the optical axis by ∼5° nasally when the orbit is in primary position; this is known as angle kappa. Although Shechtman indicated that the maximum degree of foveation along the horizontal meridian varies by 21–24% with age, it is not clear how this varies with different refractive errors. We hypothesize that the foveation would be different between emmetropes and myopes since angle kappa is smaller in myopes compared to emmetropes.9
This pilot study aimed to investigate how far in the visual field an emmetropic and myopic eye can foveate to focus the object of interest with eye rotation alone (without rotating the head) along the horizontal meridian by using psychophysically determined threshold visual acuity as a target. Visual acuity was used as a surrogate measure for foveation in this study.
Materials and methodsThis study was approved by the Institutional Ethics Committee of Kasturba Medical College and Kasturba Hospital, Manipal [IEC number: 409/2019 dated 12/06/2019]. All participants were treated per the tenets of the Declaration of Helsinki. Written informed consent was obtained from the participants after the complete explanation of the nature of the study. All the participants underwent a standard ophthalmic examination and had the best-corrected visual acuity of better than or equal to 0.0 logMAR. Both the emmetropes (spherical equivalent refraction: +0.50 to −0.50 D) and myopes (spherical equivalent refraction: <−0.50 D to −8.00 D) were recruited for this study. None of the participant's cylinder components exceeded 1 diopter. Individuals with strabismus, extraocular motility defects, retinal pathology/surface pathology, neurological defects, end gaze nystagmus in any of the extreme gazes, failed in the comprehensive eye examination were not included in the study.
Participants underwent visual acuity testing using custom-written software in MATLAB 2016a (MathWorks, MA), Psychtoolbox 3.0.10 Targets were presented in a 24 inch Dell LED monitor with a resolution of 1980 by 1080 pixes and a refresh rate of 60 Hz. Targets were always presented in the center of the monitor. The participants were seated at a distance of one meter from a computer monitor with the head stabilized by a chin rest and headband. Myopes were fully corrected using contact lenses (Bausch and Lomb SL-59 daily disposable lenses). The participant's task was to respond to the orientation of central Landot-C surrounded by flankers of Landot-C. The visual acuity was measured using a staircase test procedure with eight reversals. A target of 0.4 logMAR was shown first. For each response reversal, the step size was halved. The average of the last 5 reversals was taken as the threshold. For each eccentricity, participants underwent two staircase tests and an average of 2 staircases was taken as a final visual acuity threshold value. The two staircases were separated by 30 s of a mandatory break. All measurements were made monocularly. The right eye of the participant was chosen as the study eye and the other eye was occluded with an eye patch.
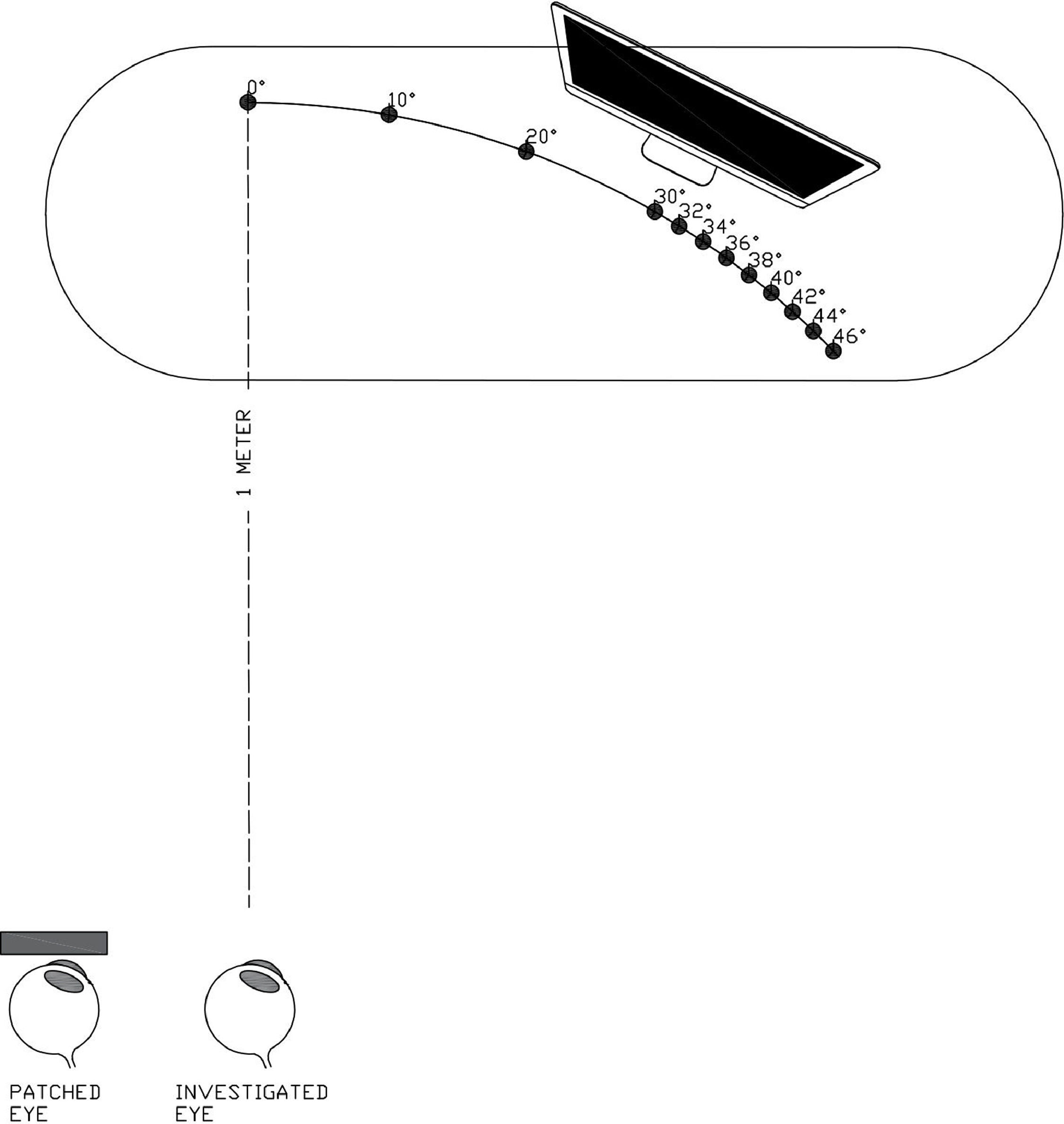
The visual acuity was measured at the fovea and different eccentricities (viewing angle) by physically moving the monitor in arc fashion to maintain distance between the eye and monitor. The schematic representation of the experiement set-up is shown in Fig. 1. We determined at which eccentricity the visual acuity drops as it indicates that the object was no longer falling on the fovea. Visual acuity was measured at different eccentricities, up to 30-degree visual acuity was measured in 10-degree step sizes and after that in 1-degree steps. Visual acuity was measured until there was a drop in visual acuity noted for at least 3 consecutive eccentricities. The step sizes and maximum eccentricity to be tested were calculated based on the pilot data. Table 1 shows the eccentricities at which visual acuity was measured for both emmetropes and myopes. The order of testing for different eccentricities was completely randomized.
Schematic representation of the experiment setup. The participants were seated at a distance of one meter from a computer monitor with the head stabilized. The visual acuity was measured using staircase procedure at the fovea and different eccentricities by physically moving the monitor in an arc fashion. This schematic representation shows the eccentricities at which visual acuity was measured for emmetropes at temporal direction.
Step size and maximum extent of eccentricities tested for both emmetropes and myopes.
R software11 was used for statistical analysis. A bilinear fit regression model was used to investigate the drop in the visual acuity in both nasal and temporal direction. The student t-test was used to compare the extent of foveal fixation between emmetropes and myopes. Differences were considered significant at p <0.05.
ResultsA total of 35 participants were recruited for the study, 28 emmetropes (15 males and 13 females), and 7 myopes (3 males and 4 females). The average age of emmetropes was 23.6 ± 2.3 years and myopes was 24± 2.2 years. There was no significant difference in the age of emmetropes and myopes (P = 0.672). The mean (±SD) spherical equivalent refractive error for myopes was −2.10 D (±0.81 D) with range: −1.00 D to −3.00 D.
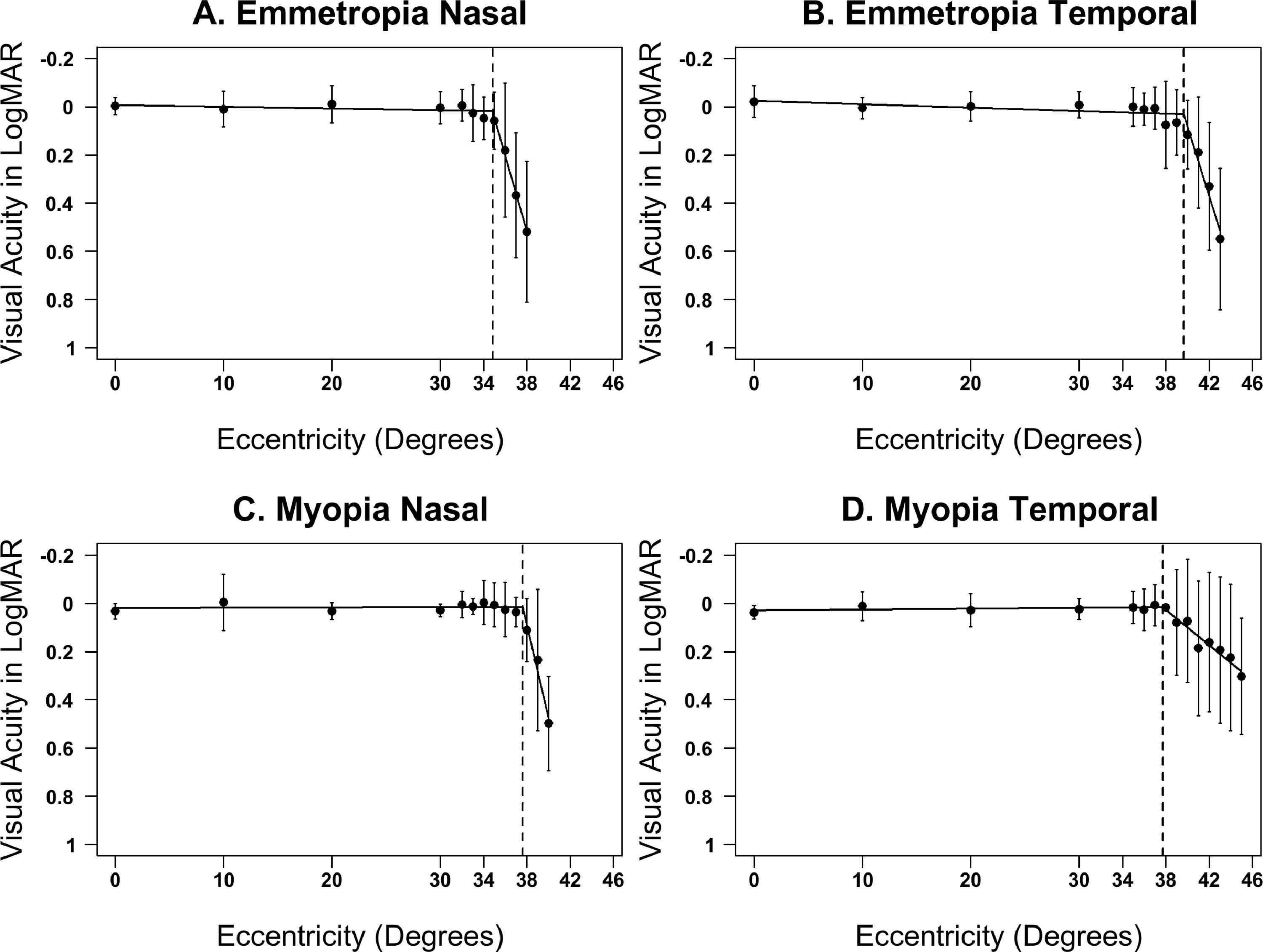
Fig. 2 shows visual acuity measurements at various eccentricities for all participants in both nasal and temporal directions. The visual acuity at fovea for emmetropes was 0.0 ± 0.03 logMAR and for myopes was 0.03 ± 0.02 logMAR in primary gaze (straight ahead viewing). The visual acuity at different eccentricities for emmetropes was maintained similar to that of fovea until 34.8 ± 2.0° along nasal (i.e. foveation through adduction) and 39.7 ± 2.7° along the temporal direction (i.e. foveation through abduction); corresponding values for myopes are 37.6 ± 2.0° and 37.8 ± 3.6° in nasal and temporal directions, respectively.
Visual acuity measures taken at different eccentricity for emmetropes and myopes in the nasal and temporal direction. The dot represents the mean visual acuity measurements for all participants and bars represent the standard deviation. The vertical line represents the eccentricity at which bilinear fit detected a change in the visual acuity.
Fig. 3 shows the box plot of eccentricity at which bilinear fit detected a change in slope for emmetropes and myopes in both nasal and temporal directions. Paired student t-test showed a significant difference in foveal fixation between nasal and temporal direction for emmetropes (P<0.001) but not in myopes (P = 0.168). An unpaired student t-test showed a significant difference in foveal fixation in nasal direction between myopes and emmetropes (P = 0.01) with the myopes foveating to a greater extent than the emmetropes. However, no such significant difference was found in foveal fixation in the temporal direction (P = 0.792).
DiscussionWe have reported the extent of foveal fixation with eye rotation in emmetropes and myopes. Shecthman et al. study was the only other study to have studied the extent of foveal fixation with eye rotation. However, the target they used was one line above best corrected near acuity.8 As expected we found a lesser extent of foveal fixation in our study compared to Shectman et al. study because we used a psychophysical threshold target. In Shechtman et al. study for a 20–29 year old the extent of foveal fixation was 48° nasally and 58° temporally. In our study, we found foveal fixation was 35° nasally and 40° temporally.
There was a statistical significance in the extent of foveal fixation in emmetropes and myopes in the nasal direction. One of the possible reasons for such difference in emmetropes and myopes could be due to angle kappa. Since myopes have smaller angle kappa9 they may tend to rotate their eyes larger as a result greater degree of foveation. Another reason for the difference in foveation between emmetropes and myopes could be due to retinal stretching in myopia which in turn could cause the stretch in the foveal pit. However, previous studies have reported smaller foveal diameter and depth in myopes compared to that of emmetropes.12,13 A recent study reported higher angular sampling density in myopes compared to emmetropes.14 While the asymmetrical differences were reported between the horizontal and vertical meridians, there is no information on how the foveal pit varies within the meridian (example: naso-temporally or supero-inferiorly). Given that retinal shapes tend to be different in myopes (more prolate in myopes) compared to that emmetropes, it is possible that the difference in foveation along naso-temporal meridian could be due to asymmetrical foveal stretching at extreme gaze positions. It should be noted that the possible explanations for the current findings are speculative at this stage based on limited literature in this area of research and need to be interpert cautiously.
Our study has few limitations. We did not measure the extent of foveal fixation in vertical directions, we intent to measure this in future study. Another limitation of our study was that we did not measure the axial length and angle kappa. It would be interesting to see how axial length and angle kappa are correlated with foveal fixation. In our study, we pilot tested only on myopes rather on hyperopes because the implications of our results are more applicable for myopes than hyperopes. For example, studies investigating peripheral refraction, or peripheral eye lengths. The range of ocular movement was shown to decrease with age.3,8 We included only young and mild myopes and it would be interesting to see how it varies for older myopes and with different degrees of myopia.
In conclusion, based on preliminary results and small sample size, we have shown that the young emmetropes can foveate up to 35° in nasal and 40° in the temporal direction, and myopes can foveate up to 38° in both nasal and temporal directions. The findings of our study indicate that eye rotation necessariliy does not match with the extent of foveation at extreme eye rotation and lays a foundation for further research work that aims at investigating various aspects of eye health in relation to eye rotation and foveation. The primary utility of our study is to a) improve the basic knowledge about the ability of eyes to fixate in extreme direction with the head fixed in the primary position and b) to help in customizing the ophthalmic instruments by fixing the endpoint of fixation and making it less cumbersome for the participant to not forcefully fixate the object in extreme gazes. For example, in studies investigating peripheral visual acuity, peripheral refraction, or peripheral eye lengths participants were given a target at different eccentricities to fixate by eye rotation. It can now be noted that such measurements may not be accurate beyond +/- 35°. These findings may also be of interest to those investigating “negative dysphotopsia”, a subjective perception of dark shadows in the periphery typically experienced by pseudophakes post cataract surgery due to focussing of image through the periphery of intraocular artificial lens.15,16 Given that restricted eye movements are known to be associated with degenerative changes, the findings of this study may also be used to understand any neurological deficits based on further evidence.
FundingNo direct funding has been reported as being related with the present study.
ORCID: https://orcid.org/0000-0002-4323-6035
Meeting presentation: Presented as poster at the British Congress of Optometry and Vision Science (BCOVS) conference, September 2020.