Low birth weight (BW) is associated with increased corneal aberrations in childhood and alterations of corneal geometry in adulthood. Increased corneal aberrations may be a factor contributing to decreased visual function in former low BW newborns in later life. Hence, the aim of this study was to analyze the long-term effect of low BW on corneal aberrations in adulthood.
MethodsIn the German population-based Gutenberg Health Study (GHS) participants (age: 40–80 years) were examined with Scheimpflug imaging (Pentacam HR, Oculus Optikgeräte GmbH, Wetzlar, Germany). The relationship between self-reported BW and the different types of corneal aberrations was analyzed using linear regression analysis as uni- and multivariable analysis with adjustment for potential confounders. The main outcome measures were corneal aberrations defined as astigmatism (Z2−2; Z22), coma (Z3−1; Z31), trefoil (Z3−3; Z33), spherical aberration (Z40) and root-mean square of higher order aberrations (HOA; 3rd up to 8th order; aperture size: 6 mm).
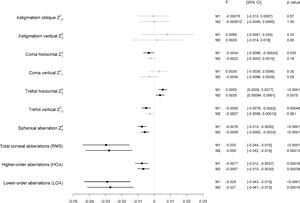
ResultsOverall, 5,628 participants were included in this analysis (3,004 women, aged 56.0 +/- 10.3 years). In a multivariable analysis lower BW was associated with decreased horizontal trefoil (B = 0.004 [0.001; 0.006] µm/500 g; p=.008); higher spherical aberrations (B=-0.006 [-0.008;-0.003] µm/500 g; p<.001), higher RMS (B=-0.028 [-0.042;-0.014] µm/500 g; p<.001), increased HOA (B=-0.007 [-0.010;-0.003] µm/500 g; p<.001) and increased LOA (B=-0.027 [-0.041;-0.013] µm/500 g; p<.001). No association was observed between birth weight and the other types of corneal aberrations in multivariable model.
ConclusionOur results indicate an association between BW and spherical aberration in adults aged 40 to 80 years. This indicates that low BW may have an association with an altered corneal shape development which may affect optical image quality and, hence, visual function.
Low birth weight is a surrogate of intrauterine growth restriction and is associated with premature birth and increased corneal aberrations in childhood.1,2 However, it is still under debate whether increased corneal aberrations contribute – amongst other factors – to the increased risk for reduced visual acuity of individuals with low birth weight. This question might have impact for public health and assessment of the economic burden associated with low birth weight. Up to now, the long-term effects of low birth weight on corneal aberrations are still unclear. It is well known, that low birth weight is associated with alterations of ocular structure and geometry in childhood, 3-7 adolescence8 and adulthood.9,10 This especially applies to corneal geometry as the cornea is exposed to lower temperature after preterm birth compared to previous intrauterine environment which may lead to a delay of corneal development resulting in a less corneal flattening.11 In former preterm low birth weight children aged 4 to 10 years a steeper corneal curvature and a smaller corneal diameter was observed.3 In a population-based study of 12 to 15 year old adolescents higher corneal power was linked to lower birth weight.8 In a recent report of the Gutenberg Health Study in adults aged 40 to 80 years the authors observed that former low birth weight individuals (<2500 g) revealed a steeper corneal curvature and a smaller corneal diameter compared to those with normal birth weight.9
The new Scheimpflug imaging contactless technical device allows detailed imaging of the anterior eye segment and corneal geometry.12,13 This technology can be used to assess corneal aberrations and to quantitatively describe its shape using mathematical modeling i.e. with Zernike (Z) coefficients. Corneal aberrations are reported to be one of the main reasons for reduced optical quality and visual function in human eyes.14 Some authors hypothesize that the relationship between refractive error and higher-order aberrations may indicate that corneal aberrations have a role in refractive error development and emmetropization. 15-19 The medical literature is still undecided as to whether corneal aberrations contribute, amongst others, to the increased risk for reduced visual acuity in former preterm low birth weight individuals.
Until now, two former studies investigated corneal aberrations in former preterm low birth weight children with Scheimpflug imaging. In one study, the authors demonstrated that former preterm children have increased corneal higher-order aberrations (HOA) at the age of 7 to 14 years.1 In accordance, results from our Wiesbaden Prematurity Study analyzing children at the age of 4 to 10 years showed an relationship of low gestational age with increased higher-order and lower-order aberrations as well as with vertical coma.2 However, to date the long-term effect of low birth weight and prematurity on corneal aberrations in adulthood is unknown and no population-based data is available.
Hence, the purpose of this study was to assess the relationship of low birth weight with different types of corneal aberrations in adults aged 40 to 80 years. We hypothesized that birth weight is linked to corneal aberrations and particularly lower birth weight is associated with increased corneal aberrations in adulthood.
Materials and methodsStudy populationThe interdisciplinary Gutenberg Health Study (GHS) is a prospective, population-based, observational cohort study in the Rhine-Main region of Western Germany (Rhineland-Palatinate).20 Recruitment and baseline examination were performed between 2007 and 2012 of participants aged between 35 and 74 years. The initial study design contained consecutive follow-ups every 5 years. Study participants were randomly drawn stratified by sex and residence (urban or rural) from local governmental registry offices where every resident has to be registered. For the present analysis, participants of the 5-year follow-up conducted between 2012 and 2017 were included because in the follow-up examination, every participant was examined with Scheimpflug imaging. Overall, 12,423 of 15,010 GHS participants (82.8%) returned for 5-year follow-up examination. In each participant, a detailed assessment of medical history was performed by a personal interview and an extensive ophthalmological examination was conducted. Written informed consent was obtained from all study participants prior to their entry into the study and the GHS complies with Good Clinical Practice (GCP), Good Epidemiological Practice (GEP), and the ethical principles of the Declaration of Helsinki. The study protocol and study documents were approved by the local ethics committee of the Medical Chamber of Rhineland-Palatinate, Germany (reference no. 837.020.07; original vote: 22.3.2007, latest update: 20.10.2015).
Birth weightParticipants were asked upon invitation to the GHS study center to review their records or family albums for a documented birth weight and were divided into the following birth weight groups: a low birth weight group < 2500 g (group 1); a normal birth weight group with a birth weight between 2500 and 4000 g (group 2); and a high birth weight group > 4000 g (group 3) as previously reported.21-25 Additionally, participants with birth weights below 1000 g and above 6000 g were excluded as these self-reported data are suspected to be unreliable. The distribution of low, normal and high birth weight in our cohort was compared to reported birth weight data in medical literature and to data of the German Federal Statistical Office as reported earlier.21,26,27 Furthermore, we validated birth weight by reviewing for a subsample of participants born in the UMCM documented birth weight in the birth register.
Ophthalmologic examinationThe ophthalmic examination of the GHS was described earlier.28 In brief, ocular examination consisted of testing distant corrected visual acuity and objective refraction (Humphrey® Automated refractor/Keratometer (HARK) 599™). Distant corrected visual acuity was measured using the built-in Snellen charts, ranging from 20/400 to 40/20 (decimal 0.05 to 2.0). Intraocular pressure was measured with a noncontact tonometer (NT 2000™, Nidek Co./Japan). Imaging of the macula and optic nerve head was conducted with a non-mydriatic fundus camera.28 Scheimpflug imaging (Pentacam™, Oculus, Wetzlar, Germany) and optical biometry (Lenstar LS900, Haag-Streit, Bern, Switzerland) was performed.28 The spherical equivalent was calculated by adding the spherical correction value to half the cylinder value.
Scheimpflug imagingThe anterior segment examination was performed with a Pentacam HR rotating Scheimpflug camera. Scheimpflug imaging enables anterior segment measurements from the anterior cornea surface to the posterior lens surface. All examinations were performed according to standardized operating procedures to diminish examiner dependent variance. Corneal tomography was based on 25 Scheimpflug images recorded within two seconds. The following corneal aberrations (analysis including anterior and posterior surface of the cornea) were recorded: oblique and vertical astigmatism (Z2–2; Z22), corneal vertical and horizontal coma (Z3–1; Z31), corneal vertical and horizontal trefoil (Z3–3; Z33), corneal spherical aberration (Z40) and corneal root-mean square of higher-order aberrations (RMS HOA; 3rd up to 8th order) and of lower-order aberrations (RMS LOA). Lower order aberrations included 1st and 2nd order aberrations (tilt, astigmatism, defocus). Zernike parameters were calculated on an optic zone of 6 mm diameter. A refractive index of 1.3375 was used to adjust the measurements of the anterior surface to match keratometer results. As reported by the manufacturer, ray tracing is used to calculate aberrations of the total cornea using the wavefront of light rays passing parallel through the cornea and to indicate the differences from an ideal (spherical) wavefront using both the shape of the anterior and posterior corneal surface.
Validation of all measurements was performed by checking quality description of the device. Furthermore, the graphical distribution of corneal parameters was analyzed and skewness was calculated. In the case of skewness ≤ |1|, we assumed approximately normal distribution. Scheimpflug images with measurements above the 4th standard deviation were manually graded by two board-certified ophthalmologists. If parts of the Scheimpflug images were of unsatisfied quality the complete Scheimpflug measurement of the participant was excluded. In every participant only one Scheimpflug measurement was performed.
CovariatesFactors that may affect corneal aberrations in our participants were considered as covariates. These included (1) age (in years), (2) sex (reference: male), (3) corneal power (in diopter), (4) axial length (mm), (5) white-to-white (mm), (6) pseudophakia (yes), (7) intraocular pressure (mmHg).
Inclusion/exclusionFor the present analysis, only participants with available self-reported birth weight, no reported history of eye injury, no report of previous corneal surgery and sufficient Scheimpflug imaging were included.
Statistical analysisA detailed statistical analysis plan was developed before conducting the analysis. The primary outcomes were total corneal aberrations as well as corneal HOA and LOA aberrations. As secondary outcome the association of birth weight with oblique and vertical astigmatism (Z2−2; Z22), corneal vertical and horizontal coma (Z3−1; Z31), corneal vertical and horizontal trefoil (Z3−3; Z33) and corneal spherical aberration (Z40) were assessed. A comparison of characteristics of included and excluded participants was conducted. Descriptive statistics were computed. Absolute and relative frequencies were calculated for dichotomous parameters, the mean and standard deviation were calculated for approximately normally distributed data, and the median and interquartile range were calculated for the remaining variables. For an eye level analysis linear regression models with generalized estimating equations (GEE) were used to assess associations and to account for correlations between corresponding eyes. Before conducting statistical analysis, the terms astigmatism oblique, coma horizontal and trefoil horizontal of the left eyes were transformed (multiplied with −1), as they showed an inverse correlation with the right eyes. In model #1, self-reported birth weight was the only predictor for the main outcome measures; in model #2, adjustment for age (in years), sex (female), corneal power (in diopter), axial length (mm), white-to-white (mm), pseudophakia (yes) and IOP (mmHg) was performed. As this is an explorative study, P values should be regarded as a continuous parameter reflecting the level of evidence; and are therefore reported exactly.29 A p-value <0.001 was considered as strong association and p<.05 as likely association and p≥.05 as not significant. R2 was calculated by the change when including birth weight as additional parameter in the multivariable model. Furthermore, two sensitivity analyses were performed. In the first analysis, participants wearing contact lenses were excluded, and in the second analyses pseudophagic subjects were excluded. All models were computed in a first step including birth weight as a continuous variable and in a second step including birth weight as a categorical variable (birth weight < 2500 g, birth weight between 2500 and 4000 g, a birth weight > 4000 g). The data were analyzed with R version 3.6.1 (2019–07–05) R Core Team (2019). R: A language and environment for statistical computing. R Foundation for Statistical Computing, Vienna, Austria. URL https://www.R-project.org/.
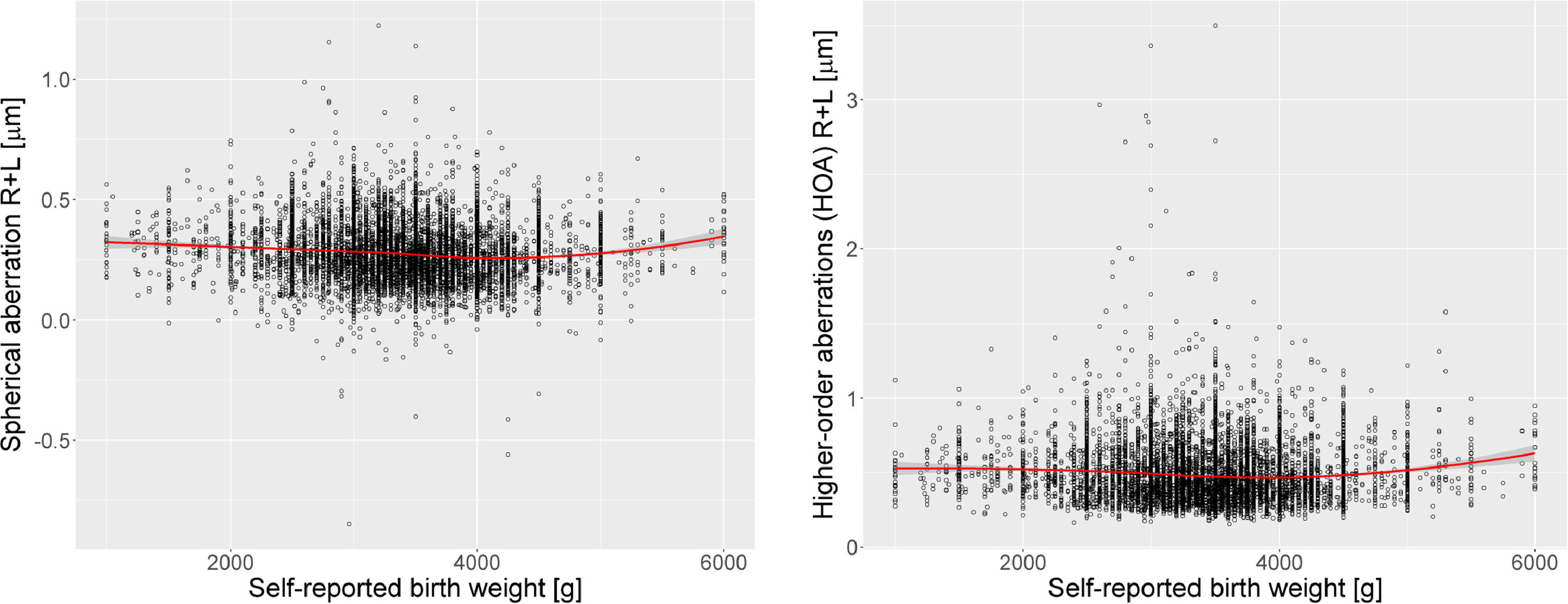
ResultsParticipant characteristicsOf the 15,010 participants at baseline 12,423 were examined at the five-year follow-up. Overall, of these participants 5269 participants were excluded because of missing birth weight data or a birth weight above 6000 g or below 1000 g. Furthermore, in 1002 participants Scheimpflug measurement was not available or not sufficient, 121 were excluded because of self-reported corneal surgery or missing information about self-reported corneal surgery and 403 because of self-reported corneal injury or missing information. In total, 5628 were included in the present study with available self-reported birth weight and Scheimpflug measurements. The mean age of study participants was 56.0 ± 10.3 years and 53.4% (n = 3004) were female. Birth weight below 2500 g (group 1) was reported by 313 participants, birth weight between 2500 g and 4000 g (group 2) was reported by 4629 participants, and a birth weight above 4000 g (group 3) was reported by 686 participants (Table 1). Measurements of corneal aberrations by birth weight groups with Scheimpflug tomography are displayed in Table 2. In Fig. 1 scatterplots of birth weight with spherical aberrations and higher-order aberrations are presented.
Characteristics of the study sample (n = 5628). Data from the population-based Gutenberg Health Study (2012–17) by sex groups. Mean ± Standard Deviation or Median and 25%/75% Quantiles.
SES – socioeconomic status; g - gram; mm-millimeter; dpt – diopter; AMD - age-related macular degeneration: WWD – White to white distance, OD - right eye; OS – left eye.
Measurements of corneal aberrations by birth weight groups with Scheimpflug tomography. Data from the population-based Gutenberg Health Study (2012–17). Mean ± Standard Deviation or Median and 25%/75% Quantiles.
All aberrations are reported in µm. OD – right eye; OS – left eye.
A p-value <0.001 was considered as strong association, p<.05 as likely association, p≥.05 as not statistically significant association.
In the non-responder analysis included subjects were younger (56.0 ± 10.3 years versus 62.4 ± 10.5 years) and more likely female (53.4% versus 45.0%).
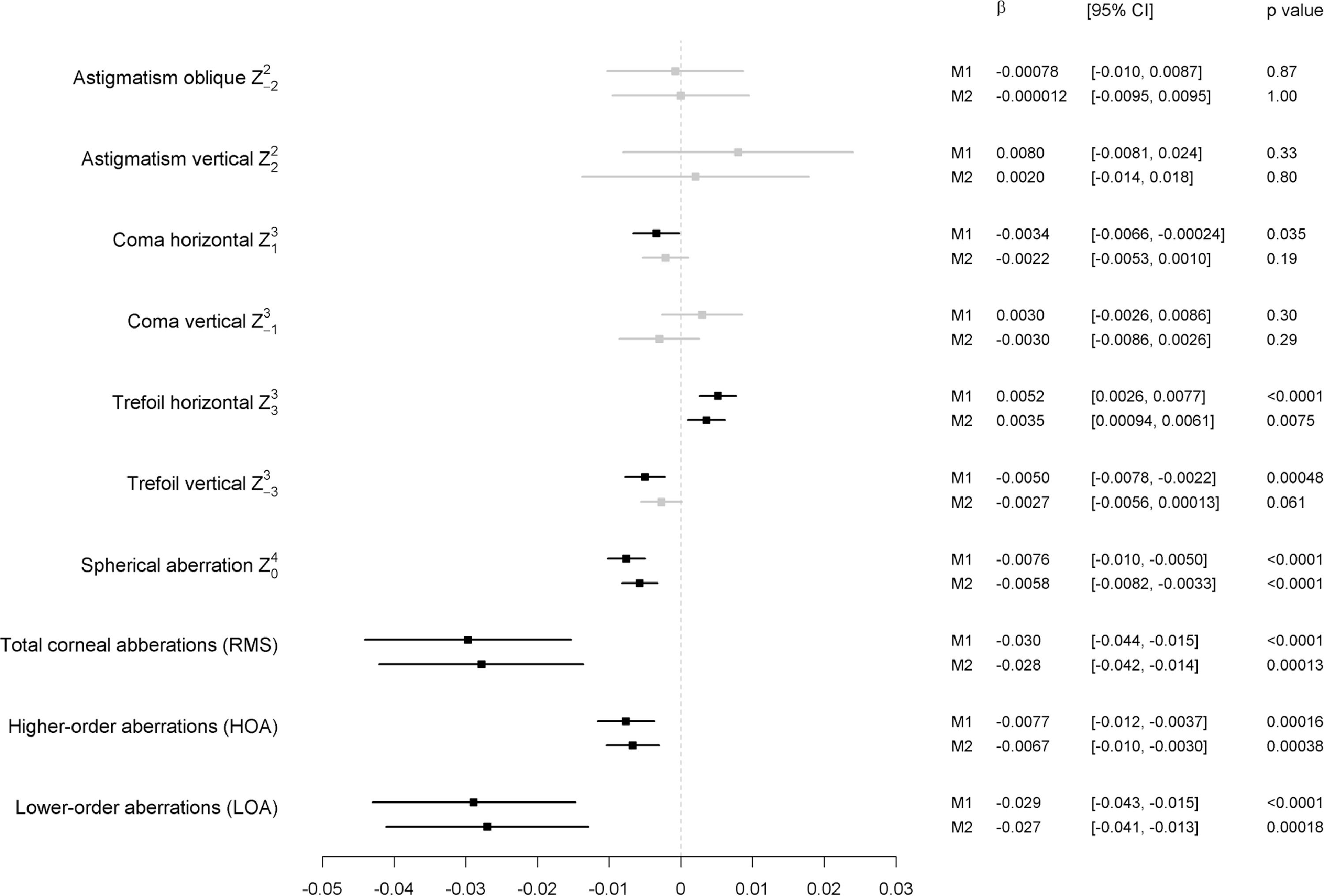
Birth weight as a continuous variableLower birth weight was strongly associated with increased spherical aberrations in multivariable model #2 (per 500 g: B=−0.006 µm [95%-CI: −0.008; −0.003], p<.001; R2 = 0.003). A strong association was also observed for lower birth weight and increased higher order aberrations in model #2 (per 500 g: B=−0.007 µm [95%-CI: −0.010; −0.003], p<.001; R2 = 0.002) and increased lower order aberrations in model #2 (per 500 g: B=−0.027 µm [95%-CI: −0.041; −0.013], p<.001; R2 = 0.002) (Fig. 2). In multivariable model #2 a likely association was observed between birth weight and horizontal trefoil (Z33), while no statistic significant association was observed between birth weight and oblique (Z2−2) and vertical astigmatism (Z22), horizontal (Z31) and vertical coma (Z3−1), and vertical trefoil (Z3−3) (Fig. 2). Corneal aberrations for corneal front and back surface are presented in appendix Table 1 and 2.
Associations of the different corneal aberration types with birth weight (continuous) in the Gutenberg Health Study (2012–2017).
Linear regression analysis using generalized estimating equations to control for correlations between right and left eyes. Estimates are present per 500 g. B – Beta; CI – Confidence interval
M1 Crude model without adjustment.
M2 Model adjusted for age; sex; corneal power, axial length, white-to-white, pseudophakia, IOP.
A p-value <0.001 was considered as strong association, p<.05 as likely association, p≥.05 as not statistically significant association.
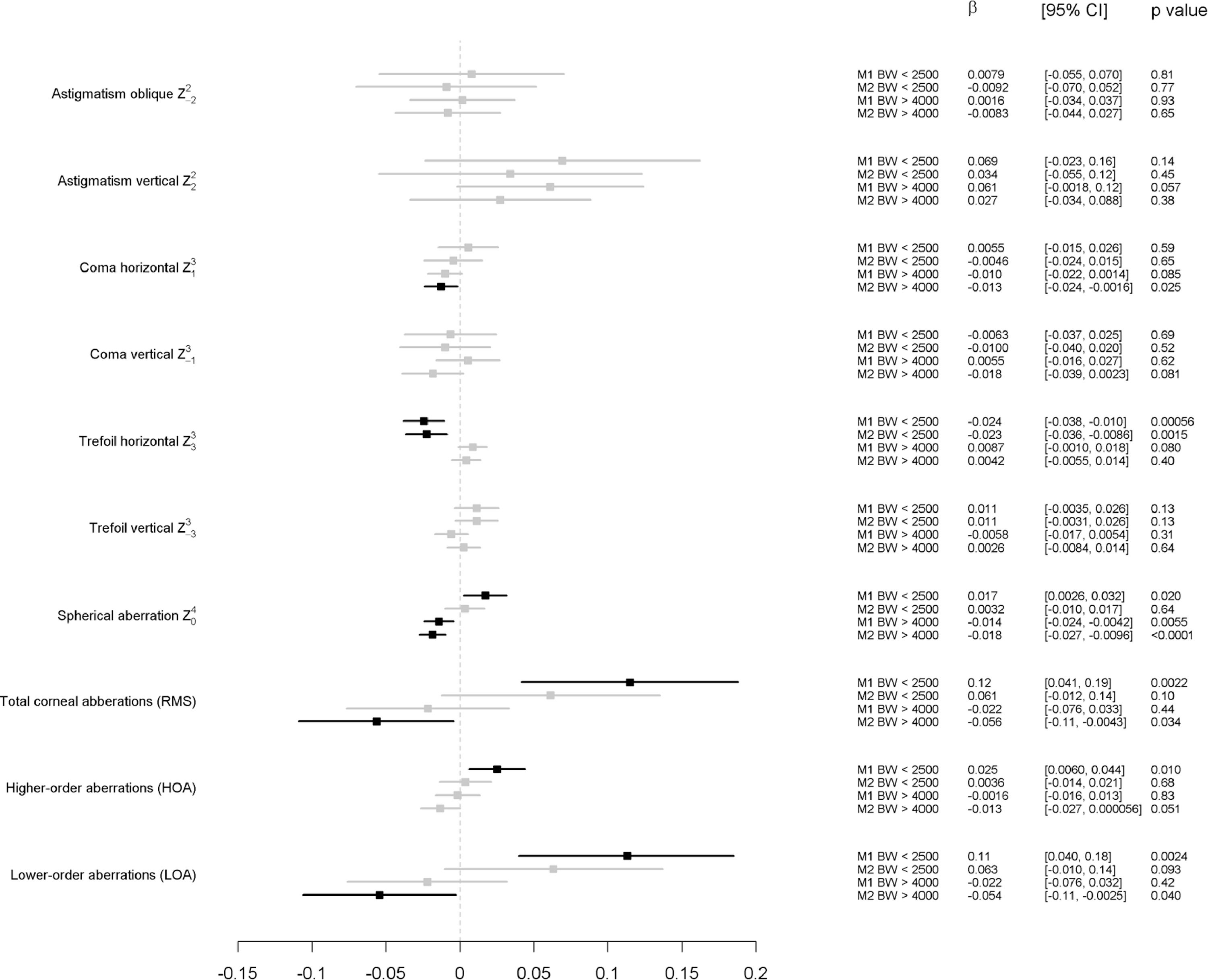
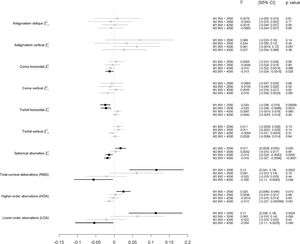
When analyzing associations with birth weight categorized into low, normal and high birth weight, no strong statistically significant associations were observed between low birth weight and the different types of aberrations. A likely association was observed between low birth weight and decreased horizontal trefoil (Z33). The higher birth weight group revealed in comparison to the normal birth weight group in the multivariable analysis after adjustment for potential confounders a strong association with lower spherical aberrations (Z40), a likely association with lower horizontal coma (Z31) and decreased total corneal and lower order aberrations while no statistically significant association was observed with the other different types of aberrations (Fig. 3).
Associations of the different corneal aberration types with Birth Weight Groups (low birth weight n = 313; normal birth weight n = 4629; high birth weight n = 686) in the Gutenberg Health Study (2012–2017).
B – Beta; CI – Confidence interval
Linear regression analysis using generalized estimating equations to control for correlations between right and left eyes.
M1 Crude model without adjustment.
M2 Model adjusted for age; sex; corneal power, axial length, white-to-white, pseudophakia, IOP.
A p-value <0.001 was considered as strong association, p<.05 as likely association, p≥.05 as not statistically significant association.
After exclusion of persons wearing contact lenses, the association analysis revealed comparable results. Furthermore, the exclusion of pseudophagic persons the results remained stable.
DiscussionThis population-based study shows that former low birth weight newborns are more likely to have increased spherical aberrations and higher order aberrations, though the effect is small. These results suggest a long-term effect of birth weight on corneal shape.
Our findings of increased corneal higher-order and lower-order aberrations in former low birth weight participants in adulthood are in accordance with previous data in former preterm and / or low birth weight individuals in childhood. Results of the Wiesbaden Prematurity Study showed that one factor contributing to increased corneal HOA in childhood was low gestational age accompanied by low birth weight while no association was observed with the occurrence of retinopathy of prematurity (ROP). 2 In that study, 226 former preterm newborns were examined and compared to 259 former full-term individuals aged 4 to 10 years using Scheimpflug imaging. Ecsedy and colleagues reported corneal aberrations in 27 (50 eyes) former preterm infants with and without ROP and compared them to 34 (68 eyes) former full term born children aged 7 to 14 years. 1 In their study sample they found increased corneal higher-order aberrations in former preterm infants.
Overall, low birth weight is associated with several anatomic alterations of ocular growth in childhood and adolescence. In the few population-based studies which are available, low birth weight children and adolescents had a steeper corneal shape,30 an increased corneal power7 as well as smaller axial length.30 We previously reported in the only population-based report assessing the association between low birth weight and ocular geometry in adulthood, that low birth weight (<2500 g) was associated with a steeper and thinner cornea, smaller corneal diameter and shorter axial length in adults at age 40 to 80 years.9 One further finding of this analysis is that low birth weight is linked to a different shape of the cornea, as indicated by increased spherical aberration and increase higher-order aberrations of the cornea. However, the effect size was small and the clinical impact remains unclear.
The mechanism leading to a different shape in former low birth weight newborns in later life is unclear. However, it is well known that low birth weight and associated factors such as intrauterine growth restriction and prematurity may cause life-long alterations of the ocular development. Fiedler and colleagues hypothesized that the difference between intra- and extra-uterine temperature after premature birth leads to a different corneal development resulting in less flattening of corneal curvature. This may lead to a different corneal shape, as indicated by corneal aberrations, as well.
Corneal aberrations are an important factor contributing to reduced retinal image quality. Some authors hypothesized that ocular aberrations are decisive for the processes of emmetropization which is linked to refractive error development.31 In our recent report on the GHS sample we found that former low birth weight individuals are at an increased risk for myopic refractive error in adulthood.21 Previous studies reported that corneal spherical aberrations of the periphery may have an effect on myopia development.32 In addition, a correlation between myopia and ocular fourth-order aberrations was reported.33
Former low birth weight individuals of the GHS cohort showed lower reduced visual acuity in adulthood, thus there is the possibility, that changes of corneal aberrations may be one of several factors leading to reduced visual acuity in low birth weight individuals.
However, it has to be stated that the effects of corneal aberrations on visual perception are small in comparison to myopia and astigmatism,34 and in congruence, a large cross-sectional study of former preterm and / or low birth weight children showed no association between visual acuity and corneal aberrations.2 Furthermore, the effect size in the present study was small which would support the hypothesis that our observed associations may be of subclinical importance.
Different regulating factors are supposed to be important for the development of corneal shape and ocular geometry. While evidence exist that axial length and spherical equivalent amongst others are regulated by genetic factors, it is assumed that corneal shape is more likely influenced by nongenetic factors.35 In a twin study of Tabernero et al.36 the authors found that genetic factors contribute up to 52% for spherical aberration development. Another important factor for corneal shape development is intraocular pressure. Particularly children with increased intraocular pressure i.e. suffering from glaucoma show an increased axial length, large corneal diameters and flatter corneal shape. These affected children have an increased corneal astigmatism in the 5 mm zone and their corneal shapes reveal more irregularities.37 Lid movements are a further important factor leading to altered corneal aberrations. Previous reports found associations of palpebral position with corneal astigmatism.38 Grey and colleagues39 observed that a narrower palpebral aperture is linked to increased cylindrical error. Read and colleagues40 observed that the corneal cylindrical axis is linked to the eyelid angle.41 These results may indicate the importance of altered palpebral development and its influence on aberration development.
Overall, our findings might be important for both, children and adults: in our previous report2 we could demonstrate that extreme prematurity is associated with increased corneal higher-order aberrations. The present study extends the previous report indicating that increased corneal aberrations are present in former low birth weight newborns in adulthood. Thus, low birth weight may be a previously unknown factor – amongst others – predisposing to increased corneal aberrations. Previous studies assumed that peripheral corneal aberrations lead to alterations in myopia development32 and others found increased coma in highly myopic eyes.17 Overall, effects of higher-order aberrations on visual quality in comparison to myopia and astigmatism are small.34 Optical quality of the human eye is only one of several components of visual perception. In addition, it is possible that corneal aberrations may be “compensated” by internal optical components and thus not effect image quality and visual perception. In our analyses trefoil, spherical aberration, and total RMS, are only 0.01 to 0.03 µm worse in low birth weight individuals. Consequently, the question about the clinical importance of this small difference remains unclear particularly whether our findings have a clinical impact on optical quality, refractive error development and visual perception or whether these differences reflect only a subclinical change.
Strengths and limitationsOne of the major limitations of the present study is that 42.4% of all GHS study participants did not provide self-reported birth weight data at baseline. Included participants were more frequently female and younger. Our data are additionally restricted because self-reported birth weight data were not validated by review of medical records for all participants. In order to ensure a high validity of self-reported birth weight data in our analyses we asked every study participant at study invitation to review personal records or family albums for recorded birth weight data and previous authors found a high reliability of self-reported birth weight10 thus we assume that this is a valid parameter in our study. In addition, we compared self-reported birth weight of a subsample of participants (n = 86) born in the UMCM. We observed a high correlation between self-reported birth weight and documented birth weight in the birth register (Correlation coefficient: 0.89 95%-CI 0.83; 0.92). Furthermore, birth weight distribution of our cohort was compared to previous reports of the German Federal Statistical Office reporting comparable distributions as reported earlier.21,42 Therefore, we assume that our findings can be generalized to the German population. Other limitations are missing perinatal data such as gestational age, intrauterine growth restriction, postnatal occurrence of ROP. In contrast to the two previous studies1,2 assessing corneal aberration in former extreme preterm children with postnatal occurrence of ROP our data reflects rather the effects of low birth in a population-based setting in adults. A further limitation is that no ocular wavefront analysis was conducted. Therefore, our study cannot report on optical quality of the human eye and we cannot state whether the increase of higher-order aberrations leads to decreased image quality on the retina in adulthood. Furthermore, corneal HOA in middle-aged adults could be affected by other factors than low BW, and we cannot state on causal relationships. Another limitation is that the presence of corneal ectasia and corneal dystrophy as well as other ophthalmic diseases apart from surgery and injury was not surveyed and may have affected our results. A further limitation is that contact lens wearers were eligible for the analysis. Participants wearing rigid gas permeable contact lenses may be expected to have some degree of corneal warpage that affects the aberrations measured. Thus we performed a sensitivity analysis and excluded persons with any contact lens use which resulted in comparable results. Limitations with respect to corneal imaging are the scanning protocol with 25 Scheimpflug images used in the present study. A previous validation study43 showed slightly poorer repeatability than, and reduced agreement with, Placido-disk videokeratoscopy particularly for certain aberrations with higher azimuthal frequenties using a scanning protocol of 50 Scheimpflug images. This has to be considered when interpreting our results.
Strengths of our study are the population-based study design, the large sample size, strict standardized examinations of all participants, and all investigators were masked to participants’ birth weight.
SummaryIn summary, this is the first report assessing corneal aberrations in former low, normal and high birth weight individuals in adulthood. Our population-based results highlight that low birth weight may be linked to life-long alterations of corneal shape. Higher-order aberrations of the cornea are inversely related to birth weight.
Funding/supportAll authors: The Gutenberg Health Study is funded through the government of Rhineland-Palatinate (“Stiftung Rheinland-Pfalz für Innovation“, contract AZ 961–386,261/733), the research programs “Wissen schafft Zukunft” and “Center for Translational Vascular Biology (CTVB)” of the Johannes Gutenberg-University of Mainz, and its contract with Boehringer Ingelheim and PHILIPS Medical Systems, including an unrestricted grant for the Gutenberg Health Study. Funders were involved in the development of the study design as scientific consultants. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Schuster AK holds the professorship for ophthalmic healthcare research endowed by „Stiftung Auge“ and finanzed by „Deutsche Ophthalmologische Gesellschaft“ and „Berufsverband der Augenärzte Deutschlands e.V.“ Wild PS is funded by the Federal Ministry of Education and Research (BMBF 01EO1503) and he is the PI of the German Center for Cardiovascular Research (DZHK). Pfeiffer N receives financial support from Novartis, Ivantis, Santen, Thea, Boehringer Ingelheim Deutschland GmbH & Co. KG, Alcon, and Sanoculis. Beutel ME received speaker honorarium from Pfizer Deutschland GmbH, Shire Deutschland GmbH and currently receives research grants from the governments of Rhineland-Palatinate and Nordrhein-Westfalen, the German Association of Psychoanalysis and Psychotherapy (DGPT), the German Research Foundation, the German Ministry of Research, the German Cancer Aid and the European Union. Fieß A, Nickels S, Urschitz MS, Münzel T, and Lackner KJ: none.
Financial disclosure/conflict of interestPfeiffer N receives financial support and grants from Novartis, Ivantis, Santen, Thea, Boehringer Ingelheim Deutschland GmbH & Co. KG, Alcon, and Sanoculis. Beutel ME received speaker honorarium from Pfizer Deutschland GmbH, Shire Deutschland GmbH and currently receives research grants from the governments of Rhineland-Palatinate and Nordrhein-Westfalen, the German Association of Psychoanalysis and Psychotherapy (DGPT), the German Research Foundation, the German Ministry of Research, the German Cancer Aid and the European Union. Schuster AK receives research support from Allergen, Bayer Vital, Novartis and Heidelberg Engineering. Fieß A., Nickels S, Urschitz MS, Münzel T, and Lackner KJ: none.
Competing interestsThe authors declare that they have no competing interests.
Boehringer Ingelheim, PHILIPS Medical Systems and Novartis Pharma provided funding towards this study. There are no patents, products in development or marketed products to declare.
Authors' contributionsConceived and designed the study: AF, AKS, SN, MEB, TM, PSW, KL, and NP; analyzed the data: AF, AKS, SN, MN, and MSU; wrote the paper: AF, critically revised the manuscript: SN, MSU, TM, PSW, MEB, KJL, NP and AKS; all authors read and approved the final manuscript.
Access to data, responsibility and analysisMN and PSW had full access to all the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis. Statistical analyses were performed by MN.
The written informed consent of GHS study participants does not approve public access to the data. This concept was requested by the local data protection officer and ethics committee. Access to data at the local database in accordance with the ethics vote is offered upon request at any time. Interested researchers can make their requests to the Principal Investigators of the Gutenberg Health Study (email: info@ghs-mainz.de).
Appendix Table 1: Anterior surface measurements of corneal aberrations by birth weight groups. Data from the population-based Gutenberg Health Study (2012–17) using Scheimpflug tomography. Mean ± Standard Deviation or Median and 25%/75% Quantiles. There are higher HOA and LOA in the low birth weight group in the anterior surface measurements compared to the normal birth weight group.
Appendix Table 2: Posterior surface measurements of corneal aberrations by birth weight groups. Data from the population-based Gutenberg Health Study (2012–17) using Scheimpflug tomography. Mean ± Standard Deviation or Median and 25%/75% Quantiles. There were higher HOA and LOA in the low birth weight group. There are higher HOA and LOA in the low birth weight group in the posterior surface measurements compared to the normal birth weight group.