To evaluate mid-term refractive outcomes and higher order aberrations of aspheric PRK for low, moderate and high myopia and myopic astigmatism with the AMARIS excimer laser system (SCHWIND eye-tech-solutions GmbH, Kleinostheim, Germany).
MethodsThis prospective longitudinal study evaluated 80 eyes of 40 subjects who underwent aspheric PRK. Manifest refractive spherical equivalent (MRSE) of up to −10.00 diopters (D) at the spectacle plane with cylinder up to 3.25 was treated. Refractive outcomes and corneal wavefront data (6mm pupil to the 7th Zernike order) were evaluated out to 2 years postoperatively. Statistical significance was indicated by P<0.05.
ResultsThe mean manifest spherical equivalent refraction (MRSE) was −4.77±2.45 (range, −10.00D to −0.75D) preoperatively and −0.12±0.35D (range, −1.87D to +0.75D) postoperatively (P<0.0001). Postoperatively, 91% (73/80) of eyes had an MRSE within ±0.50D of the attempted. No eyes lost one or more lines of corrected distance visual acuity (CDVA) and CDVA increased by one or more lines in 26% (21/80) of eyes. Corneal trefoil and corneal higher order aberration root mean square did not statistically change postoperatively compared to preoperatively (P>0.05, both cases). There was a statistical increase in postoperative coma (+0.12μm) and spherical aberration (+0.14μm) compared to preoperatively (P<0.001, both cases).
ConclusionAspheric PRK provides excellent visual and refractive outcomes with induction in individual corneal aberrations but not overall corneal aberrations.
Evaluar los resultados refractivos a medio plazo así como de aberraciones de alto orden corneales de la técnica PRK asférica para miopía baja, moderada y alta y astigmatismo miópico con el sistema de láser excímero AMARIS (SCHWIND eye-tech-solutions GmbH, Kleinostheim, Alemania).
MétodosEn este estudio longitudinal prospectivo se evaluaron 80 ojos de 40 sujetos que se sometieron a PRK asférica. Se trató un equivalente esférico de la refracción manifiesta (EERM) de hasta −10,00 dioptrías (D) en el plano de la gafa con un máximo de 3,25 D de cilindro. Se evaluaron los resultados refractivos y los datos de frente de onda (wavefront) corneal (pupila de 6mm hasta el orden 7 de Zernike) durante 2 años tras la cirugía. La significación estadística fue indicada por P<0,05.
ResultadosLa media del equivalente esférico de la refracción manifiesta (EERM) fue de -4,77±2,45 (intervalo: de -10,00D a −0,75D) en el preoperatorio y de −0,12±0,35D (intervalo: de −1,87D hasta +0,75D) en el postoperatorio (P<0,0001). En el postoperatorio, el 91% (73/80) de los ojos presentaron un EERM dentro de un intervalo±0,50D respecto al objetivo. Ningún ojo perdió una o más líneas de agudeza visual mejor corregida y ésta aumentó en una o más líneas en el 26% (21/80) de los ojos. El valor cuadrático medio de las aberraciones de alto orden y el defecto trefoil corneal no cambiaron estadísticamente en el postoperatorio en comparación con el preoperatorio (P>0,05 en ambos casos). Se observó un aumento estadístico en el coma a nivel postoperatorio (+0,12μm) y en la aberración esférica (+0,14μm) en comparación con el preoperatorio (P<0,001 en ambos casos).
ConclusiónLa PRK asférica proporciona unos resultados refractivos y visuales excelentes, con inducción de algún tipo específico de aberración corneal, pero sin afectación global de las aberraciones corneales.
Photorefractive keratectomy (PRK) is a surgical procedure for the treatment of refractive error and higher order wavefront aberrations.1–3 PRK for myopia is a surface ablation procedure that flattens the cornea by removing corneal tissue centrally, thereby changing the refractive power of the cornea and reducing myopia and may be combined with a reduction of the higher order aberrations specific to the eye.
Postoperative regression, haze and the introduction of laser in situ keratomileusis lead to reduced demand for PRK with a conventional ablation profile within a decade after introduction. However, wavefront and aspheric ablation algorithms, larger optical zones, the incorporation of transition zones and the treatment of higher order aberrations have improved its safety and accuracy over the last two decades.2–5 The ablation algorithm, named “Aberration-Free™”, which is available in the SCHWIND AMARIS platform, aims at maintaining the preoperative levels of higher order aberrations by planning the optimal ablation pattern for each individual eye. Other aspheric approaches include “customized”,6 ocular wavefront,6 corneal wavefront, topography-guided,7 wavefront-optimized,8 asphericity preserving,9 or Q-factor profiles.10
Thanks to the SCHWIND CAM software, aspheric ablation profiles are integrated in order to compensate for the peripheral loss of energy which occurs during the LASIK. In addition, the same software, in order to keep stable the preoperative corneal higher order aberrations, changed the postoperative corneal curvature using ablation algorithms that take into account the stigmatic condition, the spot overlapping and the tissue remodeling.11
The increased safety combined with the incorporation of mitomycin C to mitigate corneal haze has led to a resurgence of PRK.12 However, the long-term outcomes of PRK remain largely undocumented.
The current study prospectively evaluated the refractive outcomes and higher order aberrations of aspheric PRK for low, moderate and high myopia and myopic astigmatism with the AMARIS excimer laser system (SCHWIND eye-tech-solutions GmbH, Kleinostheim, Germany) at 2 years postoperatively.
Subjects and methodsSubject population and baseline examinationsIn this prospective study a total of 80 eyes of 40 subjects were treated with aspheric PRK for spherical myopia and myopic astigmatism. Manifest refractive spherical equivalent (MRSE) of up to −10.00 diopters (D) at the spectacle plane with cylinder up to 3.25 was treated. Subjects were enrolled in the study if they were 18 years of age or older, had a stable refraction for 1 year prior to the study and discontinued contact lenses for at least 2 weeks to 4 weeks (depending on contact lens type) prior to the baseline examination to stabilize keratometry and corneal topography. Subjects who were pregnant, breast feeding or intended to become pregnant during the course of study, were taking concurrent topical or systemic medications that may impair healing, or had systemic condition(s), which may impair healing, with active ophthalmic disease, or evidence of glaucoma or intraocular pressure greater than 22mmHg at baseline, had any prior ophthalmic surgery, had corneal topographic irregularity indicative of keratoconus in either eye, a history of recurrent corneal erosion or epithelial basement dystrophy were excluded from the study.
Preoperative examination included measurement of uncorrected distance visual acuity (UDVA), corrected distance visual acuity (CDVA), manifest refraction, cycloplegic refraction, biomicroscopy, corneal topography, manual keratometry, central corneal thickness with ultrasound pachymetry, intraocular pressure measurement, corneal wavefront measurements (6mm pupil to the 7th Zernike order), and a dilated fundus examination.
Postoperative examinations included UCDVA and CDVA as well as corneal aberrations measurements (Keratron Scout, Optikon 2000, Rome, Italy), and were performed at 1 day, 1 week, 1 month, 3 months, 9 months, 1 year and 2 years postoperatively. The same measurements at preoperatively were performed at 2 year postoperatively.
Surgical protocolA personalized nomogram was used for all treatments. All treatments were planned with the SCHWIND CAM (SCHWIND eye-tech-solutions GmbH and Co. KG, Kleinostheim, Germany) treatment planning software that compensates for the peripheral loss of energy due to an increased angle of incidence on the cornea. Sphere and cylinder input values were based upon manifest refraction measurements values. Laser software version AMARIS 2.3 combined with CAM 4.2, was used to treat all subjects. Treatments were simulated to ensure complete coverage of the mesopic pupil and to treat the refraction while respecting wavefront aberration. Optical zones were programmed into the laser, ranging between 5.75mm and 6.75mm. One surgeon (IMA) performed all treatments.
All eyes were targeted for plano postoperatively. Preoperatively, the eyes undergoing surgery were prepared by cleansing the periocular area and draping the eye. One or two drops of topical anesthetic were instilled. A lid speculum was inserted to allow maximum globe exposure. The corneal epithelium was removed using a transepithelial approach. The laser was focused on the cornea and centered on the pupil using the microscope reticule. Eyetracking during laser ablation was achieved using a 1050Hz infrared eye tracker centered on the pupil. Subjects fixated on a green fixation light, coaxial with the surgeons’ line of sight and the excimer laser beam, throughout the ablation. Correction for static cyclotorsion was implemented on all patients with astigmatism more than 1D. After the ablation, the eye was thoroughly irrigated with balanced salt solution, removing debris, and a bandage contact lens was placed on the eye. When the stromal ablation was more than 75μm, mitomycin C (MMC) was applied for 30s. Subjects received topical flouroquinolone antibiotic to use 4 times per day for 7 days, topical nonpreserved 0.5% tetracaine (Alcon Laboratories, Fort Worth, TX, USA) every 2h as needed for the first 72h and artificial tears to use 4 times per day for 2 weeks and then as needed. Topical fluorometholone (0.1%) was used on a tapering schedule of 4 times a day for 2 weeks, then 3 times a day for the next two weeks, twice a day for next 2 weeks, and then once a day for 2 weeks. The bandage contact lenses were removed after complete re-epithelialization. Retreatments although optional were not performed during the study.
Data analysisThe change in refractive outcomes and higher order aberrations was analyzed with the paired t-tests and the statistical significance of the correlations using LibreOffice Calc v3.3.2 (LibreOffice open source software).
All acuity scores are presented as the logarithm of minimum angle of resolution (LogMAR) values. Statistical significance was indicated by P<0.05.
ResultsPostoperatively, data for 80 eyes were available for the last follow-up visit at 2 years.
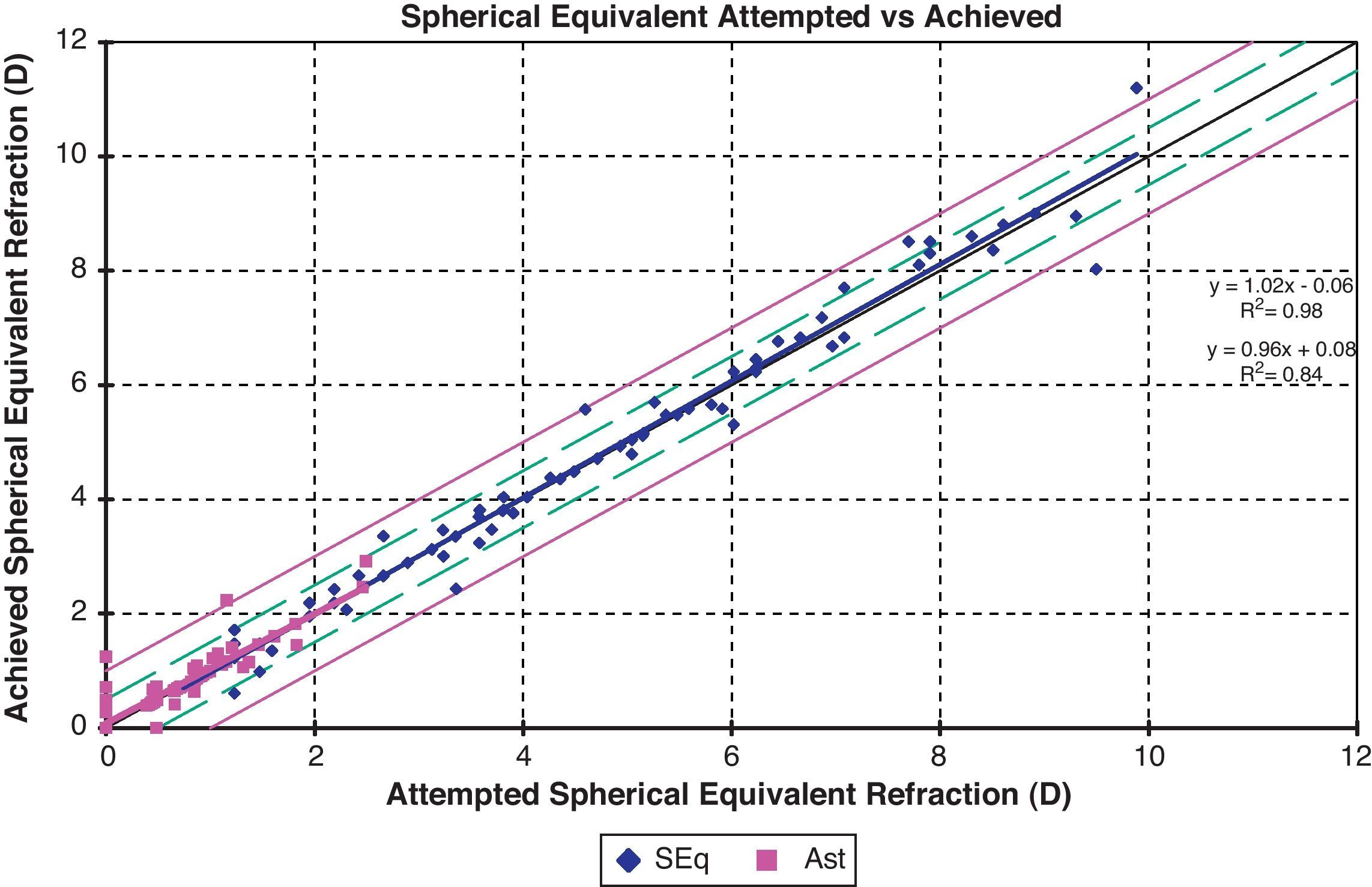
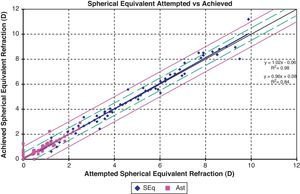
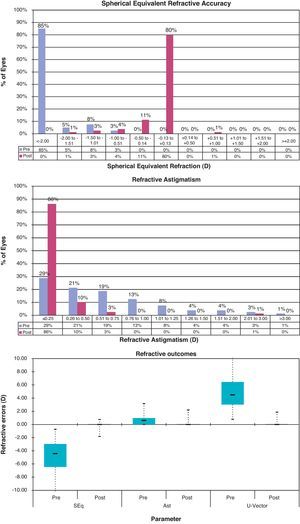
RefractionThe mean manifest spherical equivalent refraction (MRSE) was −4.77±2.45 (range, −10.00D to −0.75D) preoperatively and −0.12±0.35D (range, −1.87D to +0.75D) postoperatively (P<0.0001). The mean cylinder was 0.67±0.64D (range, 0–3.25D) preoperatively and 0.10±0.30D (range, 0–2.25D) postoperatively (P<0.0001). The attempted versus achieved MRSE and the astigmatism for all eyes are plotted in Fig. 1. Postoperatively, the attempted versus achieved MRSE was within 0.5D in 91% (73/80) of the patients and cylinder within 0.5D in 96% of them (77/80) (Fig. 2).
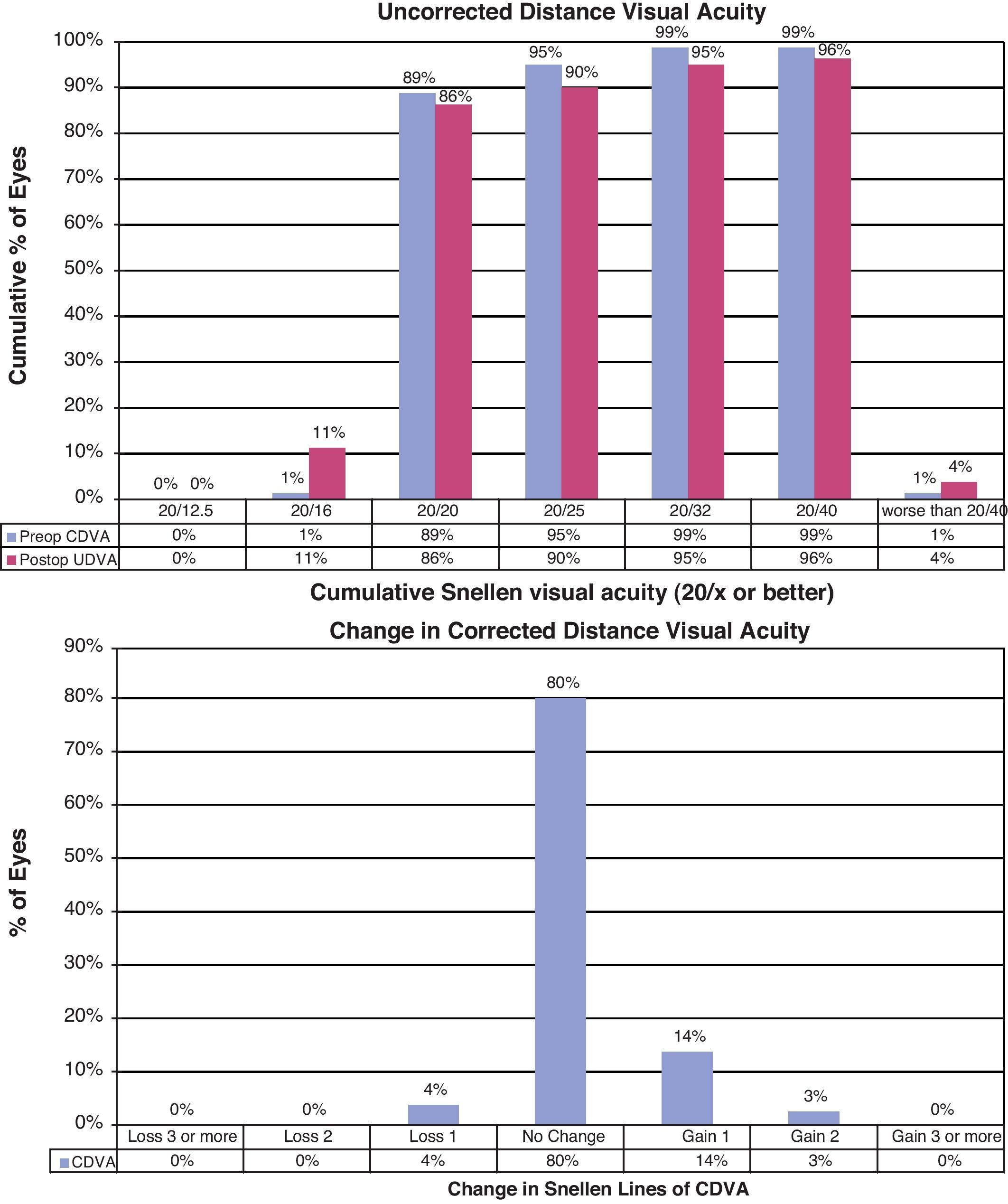
Postoperatively, 70% (56/80) of eyes had an UDVA of 0 LogMAR or better and CDVA were increased by one or more lines in 26% of eyes. Fig. 3 plots the change concerning the loss or gain of CDVA postoperatively.
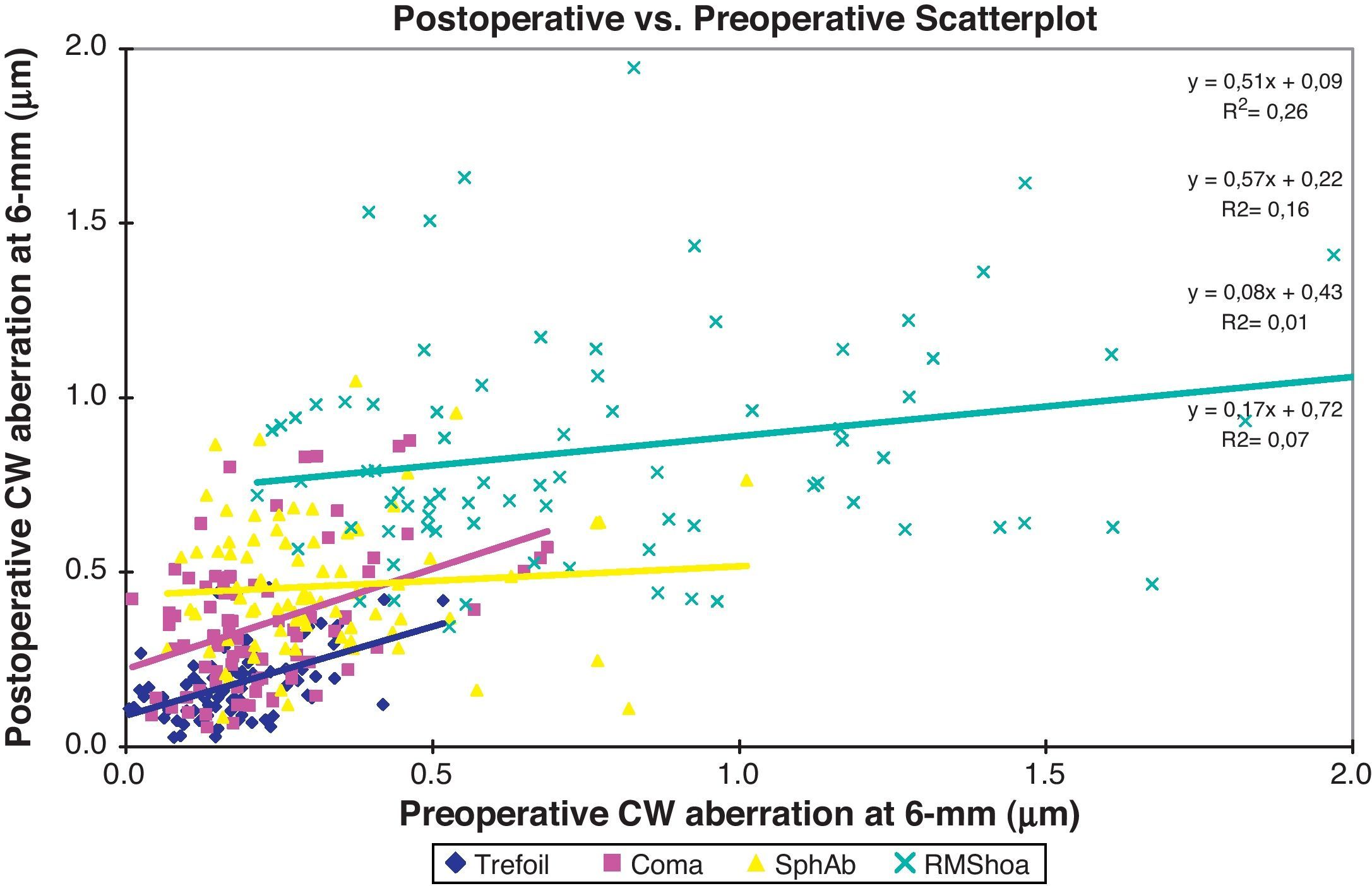
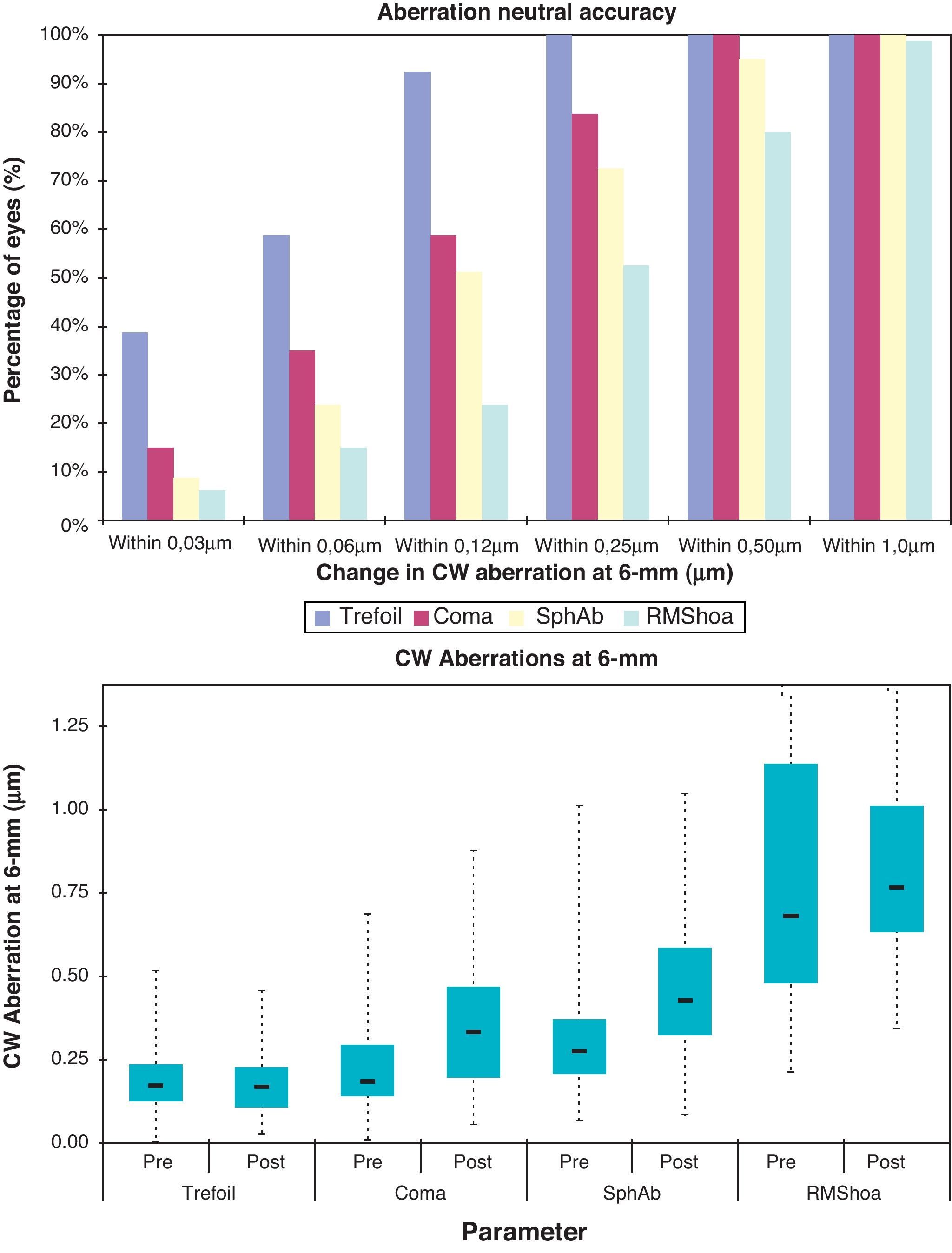
Wavefront aberrationsThe root mean square (RMS) for the total corneal higher order aberrations was 0.83±0.50μm preoperatively and 0.86±0.33μm postoperatively. The mean RMS corneal trefoil was 0.18±0.10μm preoperatively and 0.19±0.10μm postoperatively. This change was not statistically significant (P>0.05, both cases). There was a statistically significant increase in corneal coma from 0.23±0.14μm preoperatively to 0.35±0.20μm postoperatively (P<0.001). Spherical aberration increased statistically and significantly from 0.32±0.18μm preoperatively to 0.46±0.19μm postoperatively (P<0.001).
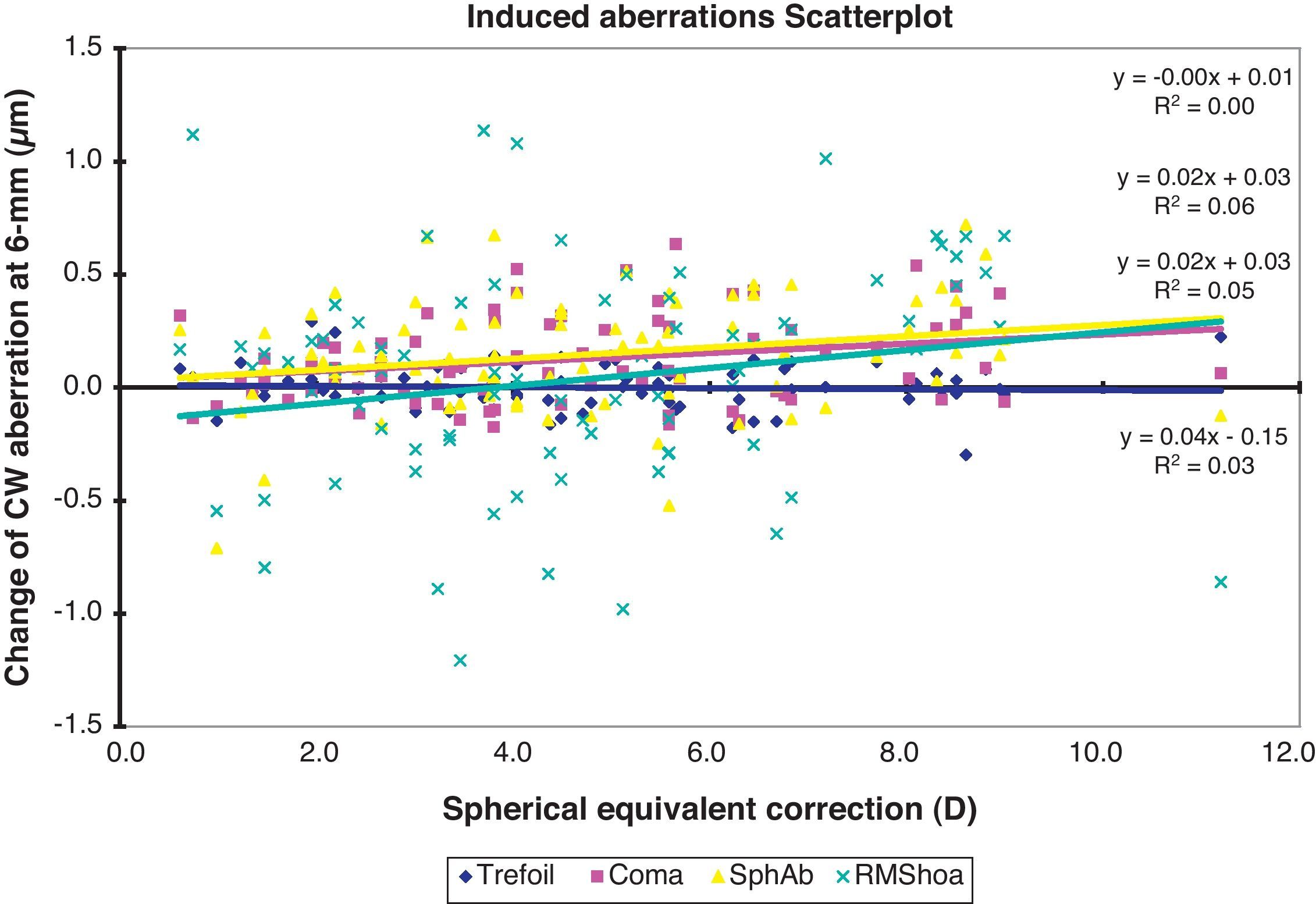
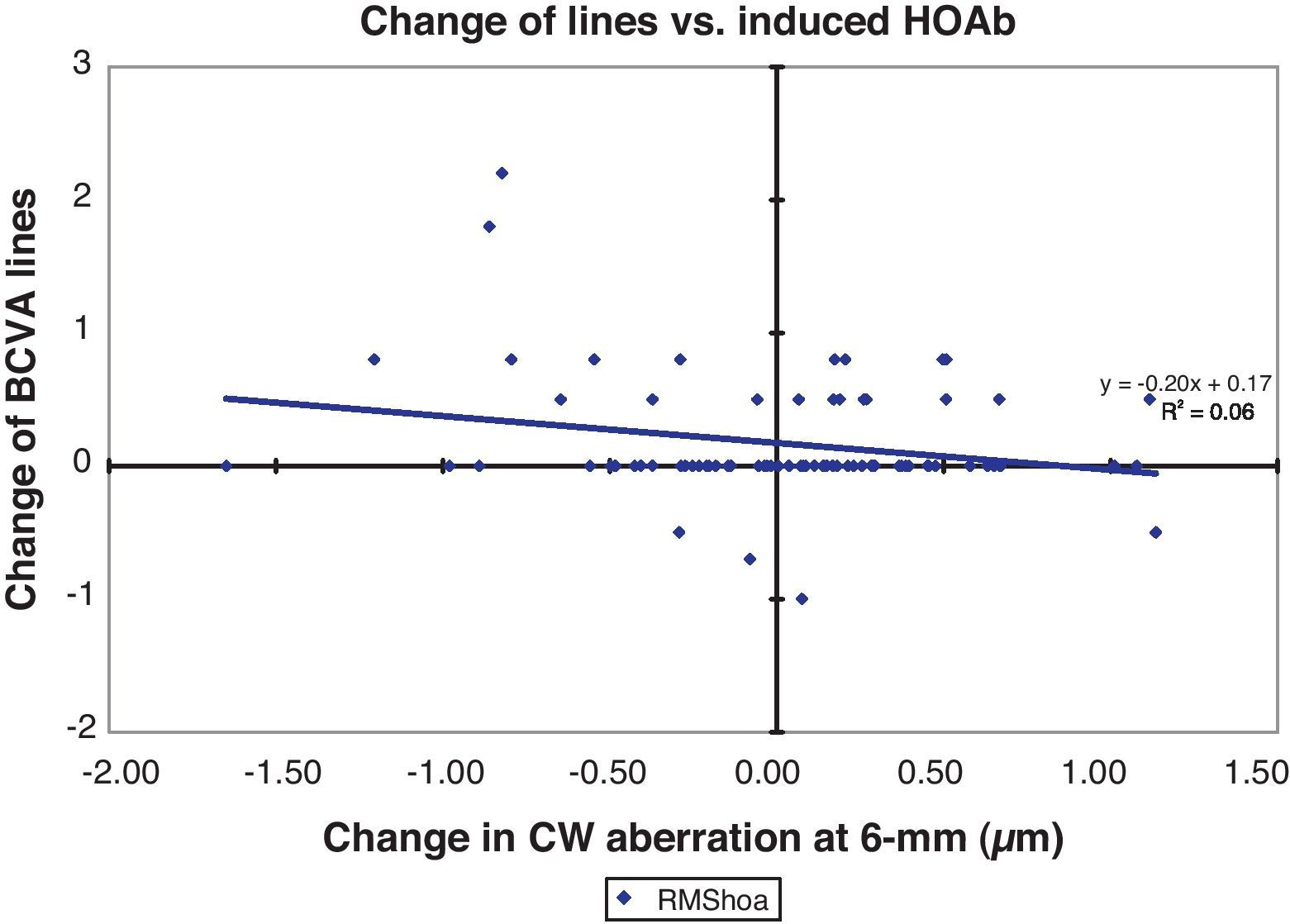
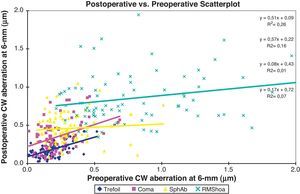
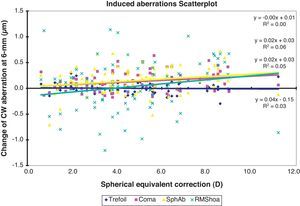
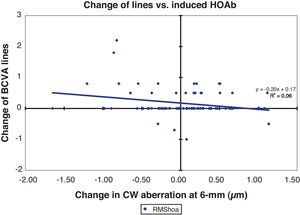
Fig. 4 plots the change in RMS of corneal higher order aberrations as a function of preoperative higher order aberrations. Postoperative coma and trefoil were correlated to their preoperative values (P<0.001 and P<0.05 respectively). The distribution of induced higher order aberrations in the cohort is presented in Fig. 5. Fig. 6 plots the change in corneal aberrations as a function of preoperative MRSE. Coma increased by 0.02μm/D of preoperative spherical equivalent (P>0.05) (Fig. 6). Spherical aberration increased by 0.02μm/D of preoperative spherical equivalent (P>0.05) (Fig. 6). Higher order RMS increased 0.03μm/D and was statistically correlated to astigmatism only (P<0.005). Fig. 7 plots the change in corneal higher order aberrations and the loss or gain of CDVA postoperatively.
Scattergram of the correlation of various corneal higher order aberrations preoperatively and postoperatively of eyes that underwent aspheric photorefractive keratectomy with the AMARIS excimer laser. All aberrations are reported for a 6mm pupil to the 7th Zernike order. SphAb denotes corneal spherical aberration; RMShoa denotes higher order aberration root mean square values. All aberrations are reported for a 6mm pupil to the 7th Zernike order.
Correlation of the change in corneal wavefront (CW) aberration and the change in best corrected visual acuity (BCVA, snellen lines) of eyes that underwent aspheric photorefractive keratectomy with the AMARIS excimer laser. All aberrations are reported for a 6mm pupil to the 7th Zernike order.
The 2-year outcomes from this prospective study indicate that aspheric PRK with AMARIS provides excellent visual and refractive outcomes. For example, postoperative MRSE was −0.12±0.35D and 91% of eyes were within 0.50D of the intended MRSE 2 years postoperatively. Postoperatively, the UDVA was 20/20 or better in 70% of patients indicating excellent level of functional visual acuity.
In previous reports, this excimer laser platform demonstrated good capabilities for sparing tissue in customized wavefront-guided treatments,13 good preservation of the bilateral symmetry before and six-months after Aberration-Free™ correction,14 as well as good hyperopic outcomes both refractively15 and in terms of effective optical zone,16 or short-term presbyLASIK outcomes.17 The eye-tracker characteristics of this specific system have also been matter of study.18
PRK remains an alternative to LASIK in cases with inadequate residual stromal thickness and patients who are apprehensive to undergo a LASIK procedure. PRK does not require the creation of a corneal flap thus eliminating flap associated complications and remains the preferred treatment for cases of recurrent corneal erosion, epithelial basement membrane dystrophy and those at risk of trauma.19 Besides, as no other pieces of equipment are required it is more cost effective than LASIK.
The visual acuities from our PRK cohort were excellent and met or exceeded FDA criteria for refractive and visual acuity including: 85% or greater eyes with UCVA of 20/40 or better, less than 5% of eyes losing more than 2 lines of CDVA; 50% or more eyes with an MRSE±0.50D of the intended correction. Safety was demonstrated with no eyes losing 2 lines or more of CDVA. At 2 years postoperatively 79% of eyes (63) were 20/16 with correction.
Our results were similar to previous reports of wavefront guided PRK that treated a similar preoperative MRSE with other excimer laser platforms.4 Nagy et al. used the Meditec MEL 70 G-Scan (Zeiss Meditec, Jena, Germany) reporting 98.6% of eyes were within 0.50D of the targeted refraction and no eyes lost CDVA at 6 months postoperatively.4 In a prospective, randomized trial of 56 patients who underwent wavefront guided PRK, Ghoreishi et al. using the Wavelight excimer laser (Alcon Inc., Fort Worth, TX, USA) reported 60% of eyes achieving 20/20 or better without correction, 96.4% of eyes were within 0.50D, and 2% of eyes lost CDVA.20
It is known that aspheric PRK is similar to wavefront optimized (or aspheric) PRK. Mastropasqua et al. treated a higher range of myopia using a wavefront optimized algorithm and found 54.2% of 24 eyes were 20/20 or better without correction.21 A prospective, randomized analysis of 56 patients who underwent wavefront optimized PRK reported 64% of eyes were 20/20 or better, 100% of eyes were within 0.50D of the targeted MSE and 2% of eyes lost 2 or more lines of CDVA.22 A recent retrospective analysis of 100 eyes that underwent wavefront optimized PRK for a preoperative MRSE of −4.97D reported mean MRSE of +0.11D at 3 months postoperatively.23 Comparison to the aforementioned studies indicates that aspheric PRK outcomes with AMARIS are equivalent to those reported for wavefront optimized or aspheric treatments.
In our cohort corneal higher order RMS remained unchanged after aspheric PRK compared to preoperatively. We can conclude that in our experience this procedure does not induce clinically significant corneal higher order aberrations. Coma and spherical aberrations did increase postoperatively but not by a clinically relevant amount. Possible causes for induced higher order aberrations include an incorrect preoperative wavefront measurement, improper centration of the ablation, imperfect alignment of the ablation to the wavefront and the postoperative healing response. Cyclotorsional alignment is important for the treatment of astigmatism and may be critical to mitigate induction of coma.24 The cyclotorsional alignment was used with all our patients (with static eye registration for all treatments with one or more diopters of astigmatism). Despite the mean induction of coma and spherical aberration, aspheric PRK did not result in an overall induction of aberrations compared to PRK with conventional ablations. A previous study of conventional PRK reported a 1.69-fold increase in higher order RMS 3 months postoperatively.25
We found postoperative coma increased as the magnitude of preoperative coma increased. Similar trends were seen for total RMS of higher order corneal aberrations and for corneal coma. Higher order RMS increased by 0.03μm/D of astigmatism indicating a correlation to preoperative refractive error. Although not investigated here, a correlation between induced total higher order aberrations and contrast sensitivity has been previously reported.26 The mild induction of total corneal higher order aberrations in the current study may have little or no effect on postoperative visual quality. In conclusion aspheric PRK was safe, effective and predictable for myopia and myopic astigmatism with clinically insignificant induction of corneal higher order aberrations.
Conflicts of interestThis work has been conducted without external financial support. Dr. Samuel Arba-Mosquera is an employee of SCHWIND eye-tech-solutions.