Albinism poses a significant threat to visual functions and causes remarkable ocular morbidity often resulting in visual disabilities. The study aimed at describing the visual status in patients with diagnosed cases of complete oculocutaneous albinism (OCA) attending to a tertiary eye hospital in Nepal.
MethodsThis was a cross-sectional descriptive hospital-based study of all diagnosed oculocutaneous albinotic cases (16 males and 9 females; mean age of 16 years) who visited the Department of Ophthalmology at the Institute of Medicine, for ocular consultation between September 1, 2011 and December 1, 2013.
ResultsTwenty-five cases (50 eyes) with OCA were enrolled in the study. All the participants had maximally reduced visual acuity (mean: 1.24±0.50logMAR). Myopic astigmatism was the most common refractive error (n=17; 34%). 58% of all participants had with-the-rule astigmatism.
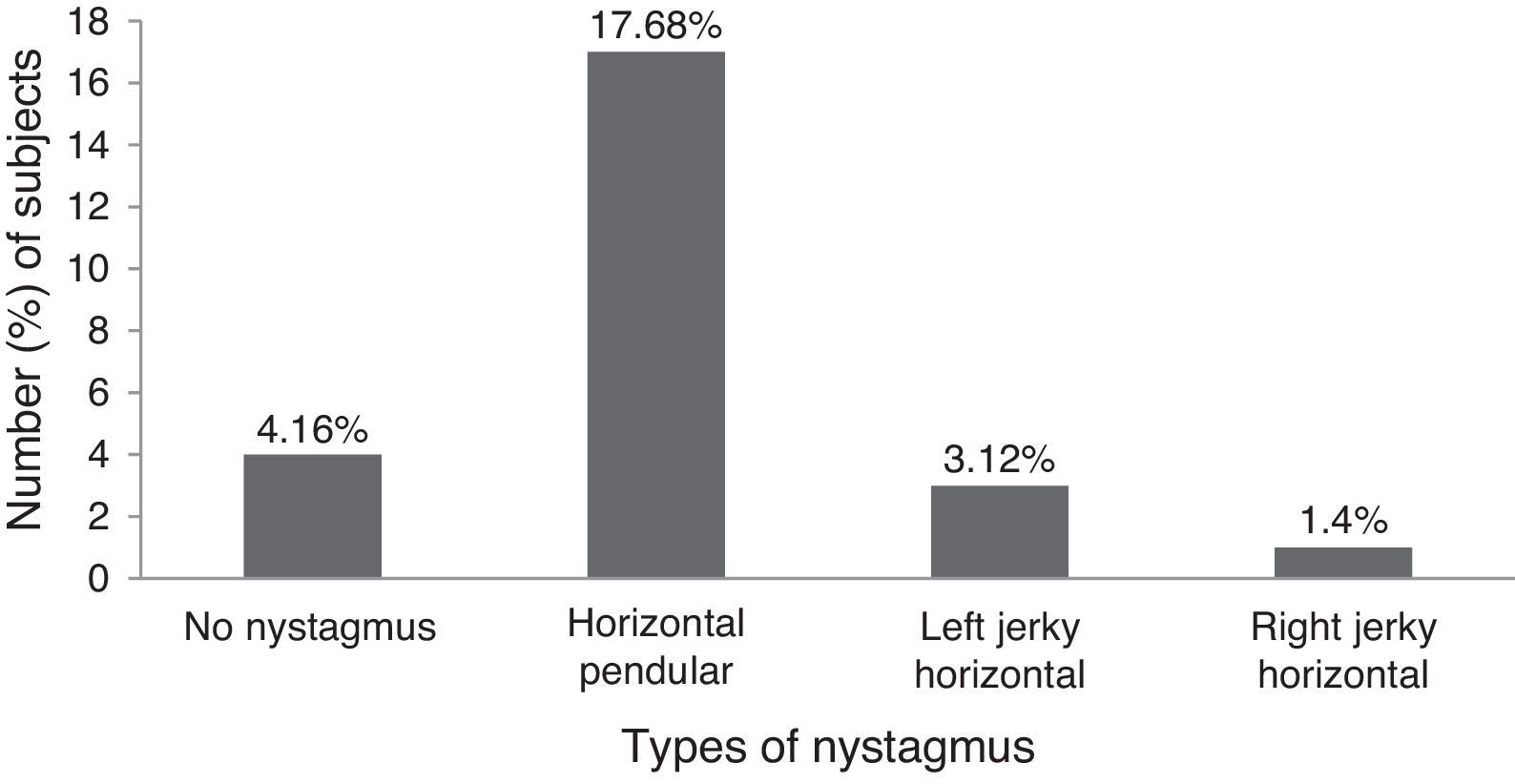
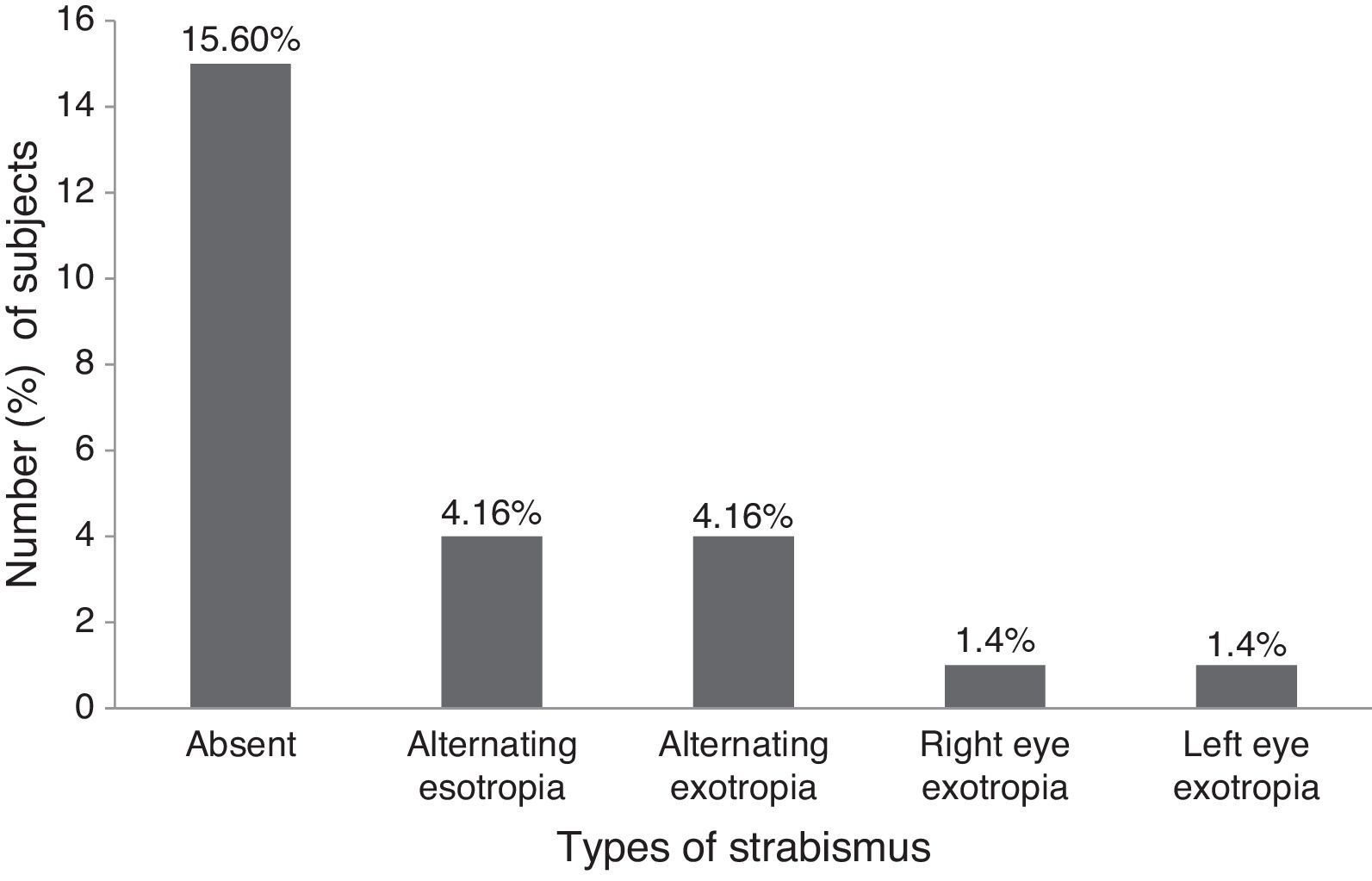
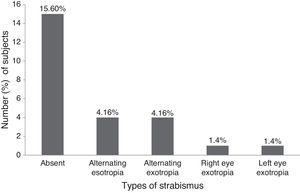
Considering the spherical equivalent power, most of the eyes (n=30; 60%) had myopia, with overall mean SE refractive error of −1.59±5.39D. Visual acuity improved significantly with refractive correction in place (paired sample t-test, p<0.05). Horizontal pendular nystagmus was the most common nystagmus (n=34 eyes; 68%). Alternating esotropia and alternating exotropia each were observed in 16% of participants who had strabismus (40% of all cases). The diaphanous iris, foveal hypoplasia and poliosis were the most consistent clinical features.
ConclusionPatients with OCA present with a broad spectrum of visual deficits that impair the visual functions. Significant improvement in visual acuity following optical correction serves as an impetus to the reduction of visual disabilities in individuals with albinism.
El albinismo constituye una amenaza significativa para las funciones visuales, y causa una morbilidad ocular considerable que deriva a menudo en discapacidades visuales. El objetivo del estudio fue la descripción de la condición visual de los pacientes con diagnóstico de albinismo oculocutáneo completo (OCA), en un hospital ocular terciario de Nepal.
MétodosEste es un estudio transversal y descriptivo llevado a cabo en ámbito hospitalario, que incluyó a todos los casos diagnosticados de albinismo oculocutáneo (16 varones y 9 mujeres; edad media, 16 años) que visitaron el Departamento de Oftalmología del Instituto de Medicina para realizar una revisión ocular entre el 1 de septiembre de 2011 y el 1 de diciembre de 2013.
ResultadosSe incluyó en el estudio a veinticinco casos (50 ojos) con OCA. Todos los participantes tenían agudeza visual máximamente reducida (media: 1,24±0,50logMAR). El astigmatismo miópico constituyó el error refractivo más común (n=17; 34%). El 58% de los participantes tenía astigmatismo a favor de la regla.
Considerando el equivalente esférico, la mayoría de los ojos (n=30; 60%) tenían miopía, con un valor medio de -1,59±5,39 D. La agudeza visual mejoró considerablemente con la realización de la corrección refractiva (prueba de t de la muestra pareada, p<0,05). El nistagmo pendular horizontal fue el nistagmo más común (n=34 ojos; 68%). La esotropía alternante y la exotropía alternante se observaron cada una en el 16% de los casos con estrabismo (el 40% de los casos). Iris diáfano, hipoplasia foveal y poliosis fueron la características clínicas más consistentes.
ConclusiónLos pacientes con OCA presentan un amplio espectro de déficits visuales que afectan a la función visual. La mejora considerable de la agudeza visual tras la corrección óptica sirve de estímulo para reducir las discapacidades visuales en los individuos con albinismo.
Albinism is a genetic disorder involving defective melanin biosynthesis, attributed to an inborn error of metabolism. A defective synthesis of melanin from tyrosine or its absence resulting from the mutation of one or more associated genes causes albinism.1 The consequence of such mutations is a reduction or absence of melanin in various parts of the body, particularly hair, skin and eyes. Albinism is universal, though unevenly distributed.2 Its frequency is estimated to be approximately one in 20,000.2 On account of its autosomal recessive inheritance pattern in most cases, males and females are often equally affected.3,4
Varying degrees of hypopigmentation occur due to different mutation types, which give rise to phenotypic heterogeneity. Traditionally the phenotypic classification of albinism hinges on dichotomous foundation – oculocutaneous albinism (OCA) and ocular albinism (OA). Oculocutaneous albinism succinctly implies reduction (incomplete OCA) or absence (complete OCA) of melanin in the eyes, skin and hair, whereas ocular albinism entails the reduction or absence of melanin in the eyes only, with the melanocytic system offering normal pigmentation to the rest of the body.5
Oculocutaneous albinism is associated with a number of visual disorders. Abnormal refractive profiles in patients with OCA have been previously established, with high refractive errors, including high with-the rule astigmatism being frequently encountered.6 There has been a bias towards both hyperopia2,15,16 and myopia6,17 in various studies regarding the distribution of refractive errors.2 Furthermore, OCA has significant anatomical defects, such as large corneal astigmatism, foveal hypoplasia and abnormal decussation of optic nerve fibers. The abnormal decussation is due to reduced or absent melanin, which is thought to determine the neuronal target specificity in the brain. This occurs secondary to misrouting of retinogeniculate projections resulting in strabismus and reduced stereoscopic vision.3,4,7 Consequently, visual acuity is generally reduced, leading to visual impairment, and cases tend to have severe photophobia as a consequence of ocular hypopigmentation. In addition, nystagmus and color vision impairment tend to occur frequently in patients with OCA.4
Although the condition is rare, it is potentially blinding because of its strong association with higher amounts of refractive error, especially corneal astigmatism, intra-ocular light scatter, light-induced retinal damage, and a partially or un-differentiated fovea.5 It is highly important that refractive errors and poorer visual acuity presenting from an early age be detected and managed appropriately. In the Asian literature, there is a paucity of data on the vision and refractive status of patients with OCA. Optometric care can help albinotic cases enhance their visual performance by improving their retinal image or training them to use their residual vision in the best possible way. As the first of its kind in Nepal, the study documents the visual deficits present in a clinical population with OCA and compares them with those observed in previous studies abroad.
MethodologyThis was a cross-sectional descriptive hospital-based study. Twenty-five consecutive cases (50 eyes) diagnosed with complete oculocutaneous albinism were included in the study. These patients with OCA were referred for ocular consultation to the B.P. Koirala Lions Center for Ophthalmic Studies, Institute of Medicine between September 1, 2011 and December 1, 2013. The study adhered to the tenets of the Declaration of Helsinki and written informed consent was obtained from all the participants.
The diagnostic criteria for oculocutaneous albinism were the presence of iris transillumination, retinal hypopigmentation and depigmentation of the skin, hair, and nails.5,8 Due to the absence of tyrosinase hair bulb incubation tests in the hospital, the participants were not further classified into tyrosinase positive or negative. A semi-structured questionnaire was designed to record the relevant history and clinical findings. The information extracted and the clinical evaluations completed were demographics (age and sex), unaided and aided visual acuities by using the Balie-Lovie logMAR illiterate and literate charts (whichever appropriate), a case history of chief complaints, previous ocular examination and use of any refractive correction, objective refraction (retinoscopy) findings and subjective acceptance, a detailed examination of the anterior and posterior segments by using slit lamp biomicroscopy and fundus evaluation under mydriasis with auxiliary lenses, and assessment of extraocular motility, strabismus, color vision, stereopsis, nystagmus, null zone and head posture. Cycloplegic refraction was carried out, in which cycloplegia was achieved upon the instillation of three drops of 1% cyclopentoalate (Cyclogyl) 10min apart. Retinoscopy was carried out 30min after the instillation of the last drop.
Iris transillumination was graded following the description of Summers et al.: grade I, normal iris pigmentation; grade II, reduced iris pigment with punctuate iris transillumination in visible locations; grade III, almost complete transillumination with the collarette having minimal pigment; grade IV, completely unpigmented irides.9 Also, the description of Summers et al. was used to grade macular transparency: grade I, a transparent macula with easily visible choroidal vasculature; grade II, slightly obscured choroidal vasculature; grade III, an opaque macula with invisible choroidal vasculature.9 Amblyopia was defined when there was reduced best corrected visual acuity or interocular difference in visual acuity in the presence of amblyogenic factors (both functional and organic). Absence of the annular and foveolar light reflexes constituted foveal hypoplasia. The unilateral cover test was used to determine whether the participants were orthotropic or heterotropic. When the heterotropia was observed, its direction and magnitude were determined by using the alternate cover test while the Krimsky test was used to find the magnitude of the manifest ocular deviation in the presence of poor fixation. The Titmus Fly Stereotest was used to assess stereopsis, which was subsequently graded into the three groups, namely no stereopsis (NS), coarse stereopsis (CS) and fine stereopsis (FS); NDS group – no stereoacuity, CS group – no better than 140″ of stereopsis and FS group – at least 100″ of stereopsis and the assessment was carried out with refractive correction, whenever appropriate.10 The 38-plate Ishihara Colour Vision Test was used to assess color vision. All the objective tests were carried out by an optometrist while the anterior and posterior segment findings were confirmed by an ophthalmologist.
Ametropia was classified into myopia, hyperopia, myopic astigmatism, hyperopic astigmatism and mixed astigmatism. Astigmatism was further classified into with-the rule, against-the rule and oblique on the basis of the strongest and weakest meridian. Visual function was classified into four levels, namely normal vision, moderate visual impairment, severe visual impairment and blindness, according to the International Classification of Disease-10. Low vision, comprising moderate and severe visual impairment together with blindness represented all types of visual impairment.11 Statistical analyses were performed by using SPSS version 20.0. The Student's t-test was used to determine the significance of the differences between the means of two groups and a Pearson linear correlation coefficient was used to study the correlation; p<0.05 was considered statistically significant.
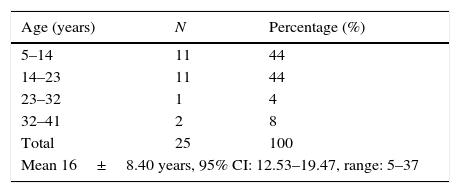
ResultsTwenty-five albinotic cases (median age=16 years; interquartile range=12) were included in the study. There were 16 males (64%) and 9 females (36%), with a male: female sex ratio of 1.78. The class intervals were exclusive and obtained using Sturges’ formula. The 5–14 and the 14–23 age groups had an equal number of participants, 11 in each (44%), whereas the least number of participants (n=1) was in the 23–32 age group (Table 1).
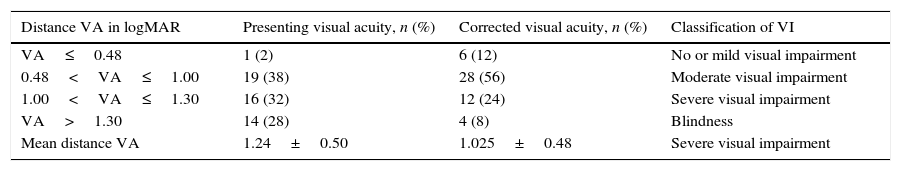
Presenting distance visual acuity was >1.30logMAR in 14 eyes (28%), >1.00logMAR but ≤1.30logMAR in 16 eyes (32%), >0.48logMAR but ≤1.00logMAR in 19 eyes (38%) and 14 eyes were blind. Mild visual impairment was observed in only one eye, with PVA of 0.48logMAR, out of 50 eyes. After optical correction using glasses, six eyes (12%) had mild visual impairment, 28 eyes (56%) had VA greater than 0.48 but ≤1.00logMAR; 12 eyes (24%) had VA greater than 1.00logMAR, but ≤1.30logMAR, and four eyes (8%) had VA greater than 1.30logMAR (Table 2). As per the World Health Organization classification based on best corrected distance visual acuity, 12%, 56%, 24% and 8% of 50 eyes had mild VI, moderate VI, severe VI and blindness respectively.
Distance visual acuity analysis.
| Distance VA in logMAR | Presenting visual acuity, n (%) | Corrected visual acuity, n (%) | Classification of VI |
|---|---|---|---|
| VA≤0.48 | 1 (2) | 6 (12) | No or mild visual impairment |
| 0.48<VA≤1.00 | 19 (38) | 28 (56) | Moderate visual impairment |
| 1.00<VA≤1.30 | 16 (32) | 12 (24) | Severe visual impairment |
| VA>1.30 | 14 (28) | 4 (8) | Blindness |
| Mean distance VA | 1.24±0.50 | 1.025±0.48 | Severe visual impairment |
Abbreviations: VA, visual acuity; n, number.
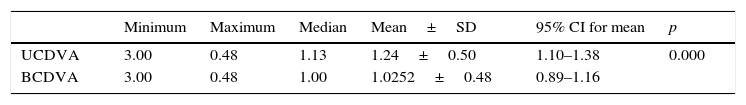
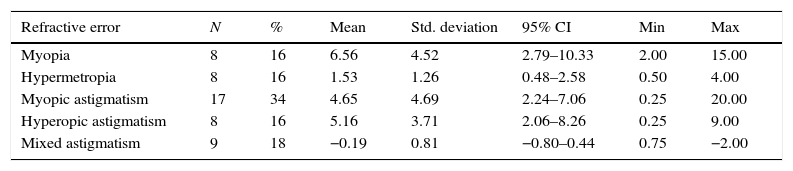
There occurred a significant mean difference between uncorrected acuity (mean acuity: 1.24±0.50logMAR) and corrected acuity (mean acuity: 1.0252±0.48logMAR); t(49)=4.91, p<0.0001. A moderately positive correlation (Karl Pearson linear correlation coefficient, r=0.80, p<0.001) was obtained between uncorrected and corrected distance visual acuities (Table 3). Myopic astigmatism was most prevalent (n=17, 34%), which was followed by mixed astigmatism (n=9, 18%), and simple myopia (n=8), simple hypermetropia (n=8) and hypermetropic astigmatism (n=8) each accounted for 16% of all refractive error (Table 4). Considering the spherical equivalent refractive error, 60% eyes were myopic and 40% eyes were hyperopic. All cases of astigmatism were the with-the-rule type except two cases, which had against-the-rule astigmatism. No oblique, or bioblique astigmatism was diagnosed. The astigmatic cylinder ranged from 0.50 diopters to 4.00 diopters, with a mean of 1.93±1.00 diopters.
Refractive error analysis.
| Refractive error | N | % | Mean | Std. deviation | 95% CI | Min | Max |
|---|---|---|---|---|---|---|---|
| Myopia | 8 | 16 | 6.56 | 4.52 | 2.79–10.33 | 2.00 | 15.00 |
| Hypermetropia | 8 | 16 | 1.53 | 1.26 | 0.48–2.58 | 0.50 | 4.00 |
| Myopic astigmatism | 17 | 34 | 4.65 | 4.69 | 2.24–7.06 | 0.25 | 20.00 |
| Hyperopic astigmatism | 8 | 16 | 5.16 | 3.71 | 2.06–8.26 | 0.25 | 9.00 |
| Mixed astigmatism | 9 | 18 | −0.19 | 0.81 | −0.80–0.44 | 0.75 | −2.00 |
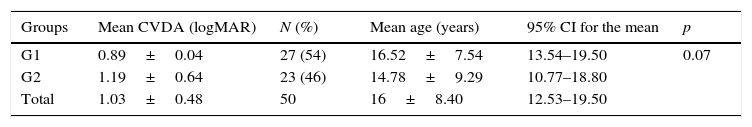
Visual acuity improvement was noted in 27 eyes following the refractive correction, while 23 eyes demonstrated no change in distance visual acuity even after the correction. Those whose visual acuity were reduced and remained statistically the same before and after the correction in the presence of amblyogenic factors (functional and organic) were diagnosed with amblyopia. Very notable visual acuity improvement occurred when it reached 1.00logMAR and 0.48logMAR from 2.0logMAR and 1.48logMAR respectively. The eyes were divided into two groups based on the whether their acuity improved upon optical correction. Group 1 (G1) showed an improvement, while Group 2 (G2) did not. The participants in G1 had a mean age of 16.52±1.45 years, and a mean corrected distance visual acuity of 0.89±0.04logMAR. The participants in G2 had a mean age of 14.78±1.93 years, and a mean corrected distance visual acuity of 1.19±0.64logMAR (Table 5).
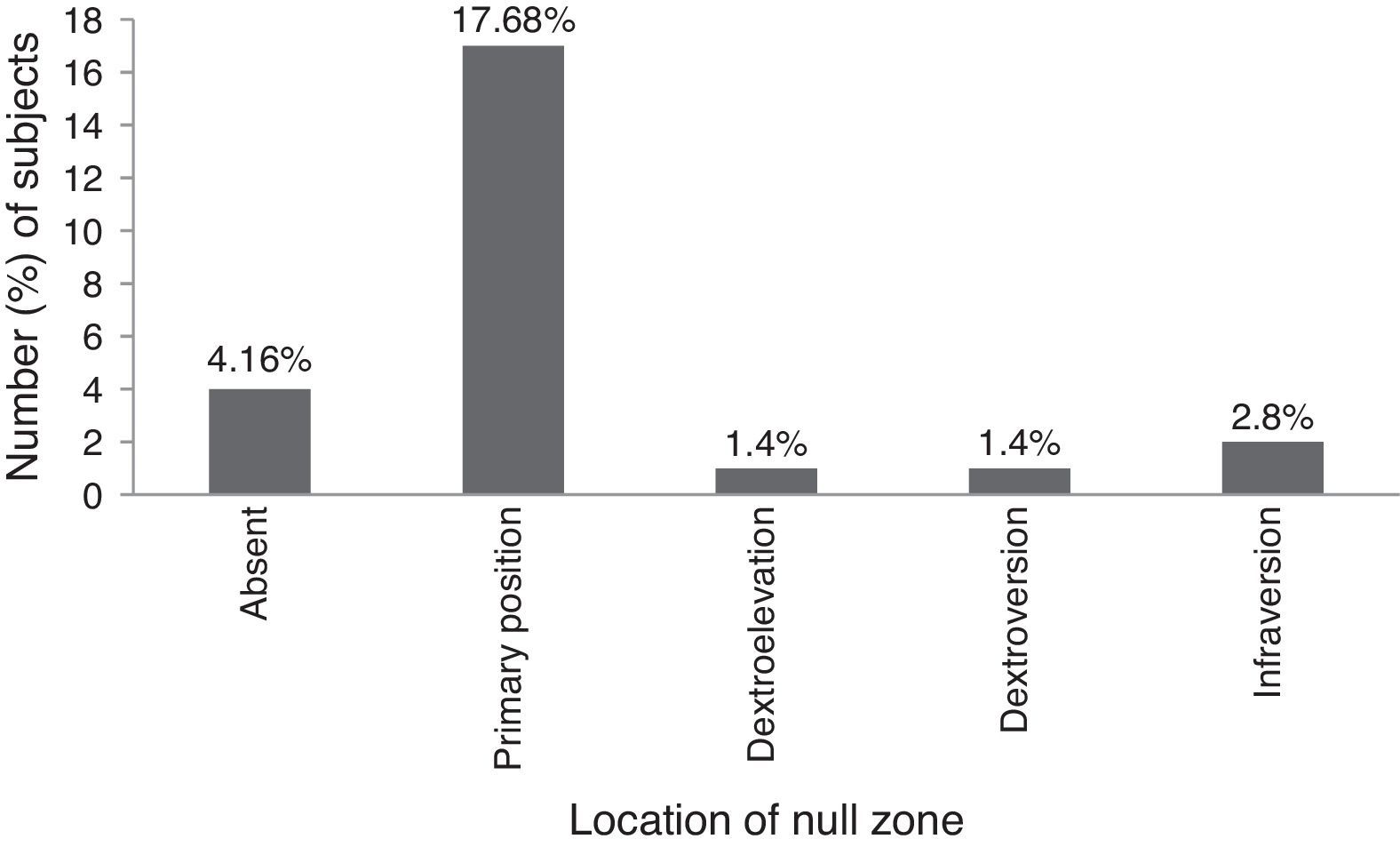
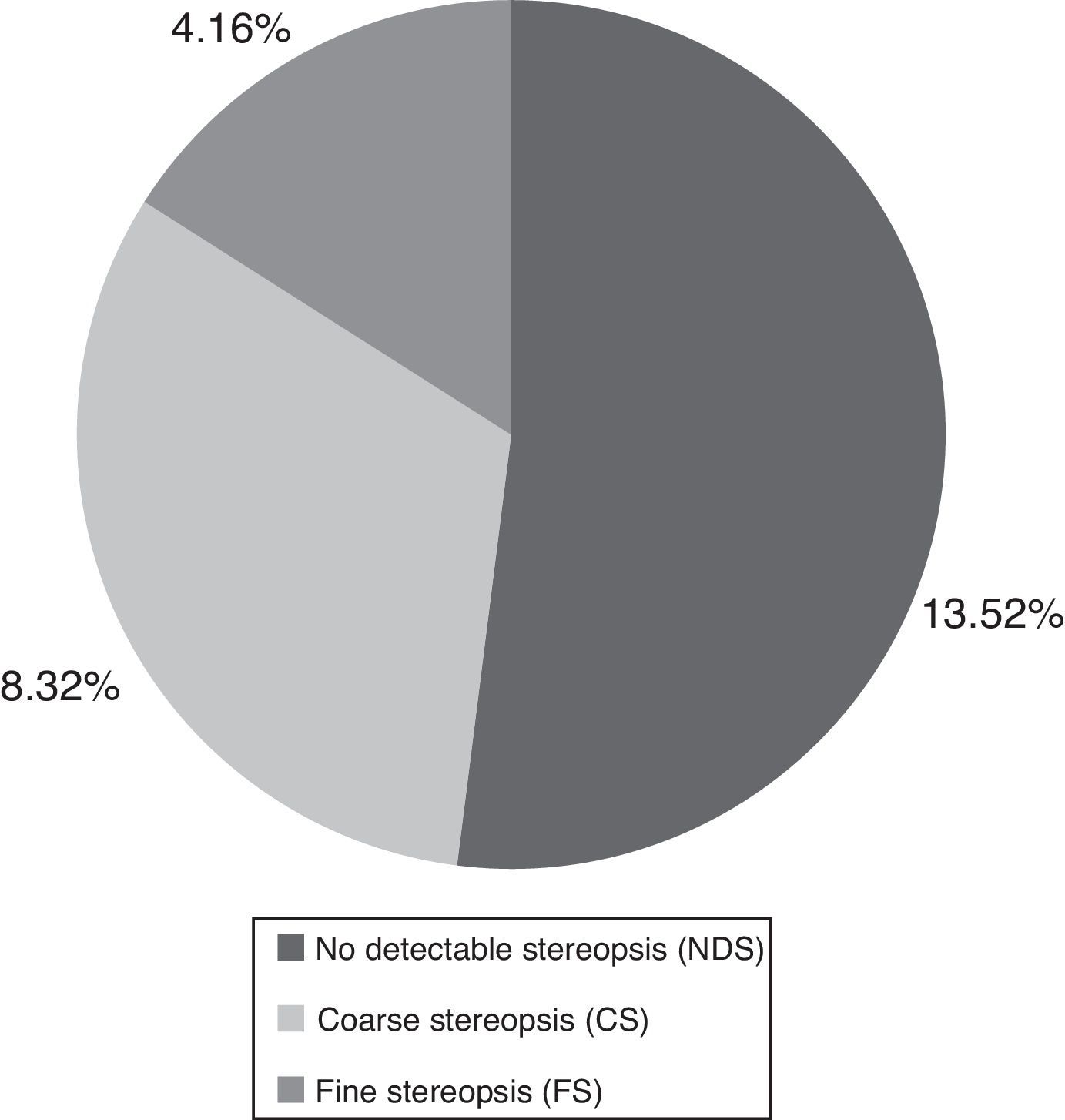
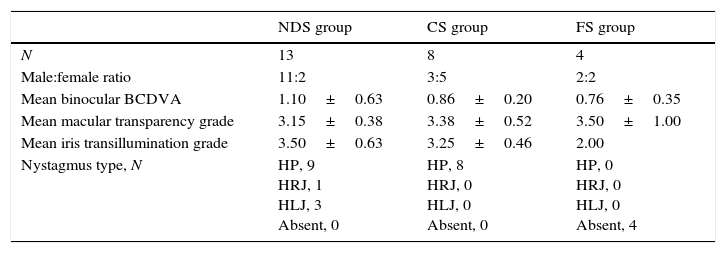
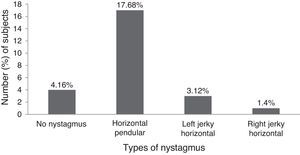
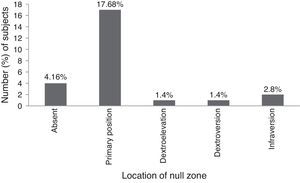
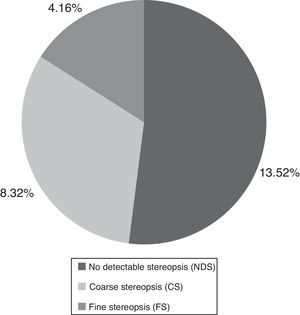
We could not single out any error type that showed best improvement statistically after the institution of an optical correction. All the eyes showed full ocular motility in all cardinal gazes. Nystagmus was present in 21 participants (84%), with horizontal pendular type (n=34 eyes, 68%) being most common, followed by horizontal left jerky (n=6, 12%) and horizontal right jerky (n=2; 4%) nystagmus (Fig. 1). Primary position (n=34, 68%) was the most common null point (Fig. 2). No heterotropia was observed in 15 participants (60%). Alternating esotropia and alternating exotropia each were present in four participants (16%). Right eye exotropia (n=1; 4%) and left eye exotropia (n=1; 4%) were the least common of all (Fig. 3). Fine stereopsis (FS) was observed in four participants (16%), coarse stereopsis (CS) in 8 participants (32%), and no detectable stereopsis (NDS) in 13 participants (52%) (Fig. 4).
All of the participants reported they had blurring of vision for both distance and near and experienced photophobia. Foveal hypoplasia, iris diaphanous translucency and the absence of foveal reflex were universally present. The participants were also divided into three groups based on the stereopsis grading (Table 6). The NDS group consisted of 13 participants, the CS group consisted of 8 participants and the FS group consisted of 4 participants. As stereopsis improved, the visual acuity was seen to increase; however, this increment in distance visual acuity was not of statistical significance (one-way ANOVA with post hoc tests, p=0.66). Of the three groups, macular transparency was found to be least in the NDS group; the highest transparency was observed in the FS group, followed by the CS group. The mean difference in the macular transparency was not statistically significant whilst comparing the NDS and CS groups, whereas the transparency difference was significant whilst comparing the NDS and FS groups (p=0.010), and comparing the CS and FS groups (p=0.04). Participants in the FS and CS groups exhibited a lower iris transillumination defect compared to those in the NDS group. The mean iris transillumination grade in the NDS group was the highest and differed significantly from that in the FS group (p=0.036), whose mean also differed from that of the CS group (p=0.038). No significant mean difference was observed between the NDS and CS groups (Fig. 4). Color vision was normal in 19 participants (76%), while three participants (12%) had a red-green color vision deficiency. In three participants (12%) color vision function could not be assessed. The magnitude of strabismus averaged 24.15±8.02 prism diopters (magnitude interval, 12–40 prism diopters). None of the participants were found to adopt a compensatory head posture to dampen nystagmus.
Analysis of groups based on stereopsis.
| NDS group | CS group | FS group | |
|---|---|---|---|
| N | 13 | 8 | 4 |
| Male:female ratio | 11:2 | 3:5 | 2:2 |
| Mean binocular BCDVA | 1.10±0.63 | 0.86±0.20 | 0.76±0.35 |
| Mean macular transparency grade | 3.15±0.38 | 3.38±0.52 | 3.50±1.00 |
| Mean iris transillumination grade | 3.50±0.63 | 3.25±0.46 | 2.00 |
| Nystagmus type, N | HP, 9 HRJ, 1 HLJ, 3 Absent, 0 | HP, 8 HRJ, 0 HLJ, 0 Absent, 0 | HP, 0 HRJ, 0 HLJ, 0 Absent, 4 |
Abbreviations: NDS, no detectable stereopsis; CS, coarse stereopsis; FS, fine stereopsis; HP, horizontal pendular; HRJ, horizontal right jerk; HLJ, horizontal left jerk.
Individuals with oculocutaneous albinism have visual impairment that renders their social interactions compromised compared to their typical peers, hence encumbered cognitive, emotional, social and academic development. This makes them more prone to social isolation and greater stigmatization. As a result, they are caught in a vicious circle of the poor development and social ostracism. In the current study, that all the eyes had visual impairment with the majority (38%) of them having moderate VI can be explained in part by higher refractive error that was amblyogenic and in part by other factors, such as hypoplastic foveae, squint, nystagmus, and photophobia; this is consistent with the results by Eballé et al.12 who reported that the majority (70%) of the eyes had moderate visual impairment.
There have been reports in the literature that higher spherical and astigmatic refractive errors are associated with albinism.13,14 As both hypermetropia2,15,16 and myopia6,17 have been reported to be associated with albinism, this study also encountered both types even with higher magnitude refractive errors. In much the same way, this study found that 20% of all participants (5 participants, 10 eyes) had refractive error greater than 10D. This finding is also comparable to that obtained by Perez-Carpinell et al. who reported that 14% of the albinos had refractive error greater than 10D.18 The participants in this study exhibited a refractive bias towards myopia; the finding being distinct from Wildsoet et al.’s study which showed a bias towards hypermetropia.2 Mvogo et al, in their study, reported the prevalence of 61.9% and Eballe et al. observed that of 40% establishing myopic astigmatism to be the most common refractive error in albinos.12,19 This study also found the similar result in which 34% of the cases had myopic astigmatism making it the most prevalent refractive error in patients with OCA. On the contrary, other studies reported hypermetropia to be the most common refractive error.2,15,16 Because emmetropization is afflicted by large corneal astigmatism and a constant motion of the retinal image, large refractive errors ensue.20 In strong agreement with our study which obtained larger amounts of astigmatism, especially a with-the-rule type, the studies also maintain strong associations of albinism with with-the-rule astigmatism.2,12,15 Refractive astigmatism thus seen is largely corneal in origin, in that the cornea is steeper along the vertical meridian compared to the horizontal meridian. The preferential curvature change along the vertical meridian is possibly due to the pressure exerted by the upper lid on the moving cornea.17,21
In this study, the mean PVA was 1.24logMAR, while the same in the study by Eballé et al. had a mean PVA of 0.96logMAR, which was expressed as a decimal value of 0.11.12 These acuities are comparable. The fact that significant improvement in visual acuity followed after refraction correction bears strong positive resemblance to the study by Eballé et al.,12 who also categorized all eyes in two groups: one group (G1) which showed improvement and the other (G2) that did not show improvement; the ratio of the number of eyes in G1 to that in G2 was approximately 1.06. Similarly, in our study the ratio is obtained as 1.17. This suggests that acuity rises in a greater number of eyes. This calls for more refraction services and optometric care.
Binocular anomalous color vision was reported in 44% of cases in the study by Perez-Carpinell et al.18 In this study, binocular color vision was normal in 19 participants (76%), which represents a substantial percentage. Misrouting of reticulate projections at the optic chiasm is attributed to melanin deficiency, causing strabismus which is frequent in albinism and therefore results in a lack of stereoscopic vision.22 A large angle kappa as high as 17.11 exo prism dioptres was observed in a study.23 This angle may simulate, mask or exaggerate tropia. In this study, the mean magnitude of strabismus was recorded at 24.15±8.02 prism diopters (magnitude interval, 12–40 prism diopters), which is significant. Absence of nystagmus and strabismus correlated well with fine stereopsis, i.e., there was no fine stereopsis if either nystagmus or strabismus or both were present and when either or both of them were absent, individuals possessed a stereoscopic vision. This signifies that the absence of both is crucial for stereopsis. And also that visual acuity was greatest in the FS group suggests the role of nystagmus in the deterioration of visual acuity. This study is similar to the study by Lee et al. which reported that the patients with fine stereopsis had better visual acuity.10
Similar to the reports that nystagmus is invariably present in OCA and that in most cases it is horizontal and pendular, this study had 84% of participants with nystagmus and 68% had a horizontal and pendular type.2,24 None of the participants assumed an abnormal head posture. It could be explained by the fact that there occurred no vertical misalignment and the participants had adapted to the straight-head posture. In addition, 17 participants (68%) had the null zone in the primary position. Also, as obtained in the study by Lee et al., who reported more melanin in the macula and the iris in albinism is associated with greater acuity and increased stereopsis, this study confirmed those findings.10 In relation to the fovea only, poor visual acuity can therefore be ascribed to less pigment as suggested by this study, and varied cone morphology and cone specialization.25
Despite its low prevalence, albinism remarkably causes visual impairment, blindness, amblyopia and challenges an educational environment, all leading to educational retardation; therefore, optometric care must be administered with refractive optical correction which incorporates filters to lessen or eliminate photophobia and prisms to eliminate abnormal head postures, if any, at their very early age so as to prevent them from stigmatization related to poor development and impairment.12,26,27 In light of a significant role that optometrists can play in the rehabilitation of the individuals with albinism and improving their quality of life, it is high time other health care professionals started referring albinos for optometric intervention in the form of refractive correction and low vision rehabilitation.
The fact that the 5–14 and 14–23 age groups each had 44% of all participants (the highest compared to any other age group) illustrates that oculocutaneous albinos seek medical attention as early as possible in their lives because it is a congenital and visually impairing condition, which limits a child's overall development; a greater number of males in this study could be suggestive of easier access to health care by males than females, who are still unjustly treated, because of Nepal's patriarchal societies which view females as subordinate to males.
Due to small sample size, caution should be taken while generalizing the findings of the study. However, small sample size signifies the rarity of condition in Nepal and the lack of appropriate referrals for low vision examination. Despite a small sample size, the present study effectively presents the gravity of the visual deficits found in oculocutaneous albinism and attempts to apprise the concerned authority of the burden, and also calls for planning and advocacy of appropriate optometric care essential for visually impaired people living with albinism in Nepal and abroad. In low-income countries like Nepal where disability care is often not a priority, this study helps mark an important milestone for more optometric care. The ultimate aim of this study is to increase awareness and improve vision care and intervention for albinism cases. In addition, this study provides a baseline for possible prospective research in the future, including studies on visual deficits in albinism by OCA sub-types.
As a result of various factors associated with oculocutaneous albinism, visual performance can be greatly enhanced by instituting appropriate optical treatment following cycloplegic refraction performed by optometrists. Optical treatment is a blend of refractive correction and photophobia alleviation with appropriate lenses and filters. Since albinism has strong associations with higher refractive error and ocular pathologies, the likelihood of occurrence of amblyopia (both functional and organic) increases, whose severity becomes likely to be reduced, if not effaced, provided refractive intervention is done early in life. This study warrants adequate optometric interventions to help care for oculocutaneous albinos because 54% of all participants significantly improved their acuity with refractive correction. Albinism is a condition, but carries a spectrum of other deficits which necessitate optometric care, which is possible by increased public awareness and appropriate referral.
Conflicts of interestThe authors have no conflicts of interest to declare.