Systemic lupus erythematosus (SLE) is a multiorgan autoimmune disease of unknown etiology with many clinical manifestations.
We report the first case of SLE in which visual alterations were evaluated with multichannel perimetry.
Some achromatic and color vision alterations may be present in SLE, especially when treated with hydroxychloroquine. The sensitivity losses detected in the chromatic channels in the central zone of the visual field were consistent with the results of the FM 100 Hue color test. Likewise, the multichannel perimetry detected sensitivity losses in the parafoveal area for both chromatic channels, especially for the blue-yellow.
El lupus eritematoso sistémico (LES) es una enfermedad autoinmune multiorgánica de etiología desconocida, con muchas manifestaciones clínicas.
Reportamos el primer caso de LES en el que se evaluaron las alteraciones visuales utilizando la perimetría multicanal.
En el LES pueden presentarse ciertas alteraciones acromáticas y de la visión del color, especialmente cuando se trata la enfermedad con hidroxicloroquina. Las pérdidas de sensibilidad detectadas en los canales cromáticos de la zona central del campo visual fueron consistentes con los resultados de la prueba de color FM 100 Hue. De igual modo, la perimetría multicanal detectó pérdidas de sensibilidad en el área parafoveal para ambos canales cromáticos, y en especial para el azul-amarillo.
Systemic lupus erythematosus (SLE) is a multiorgan autoimmune disease of unknown etiology with many clinical manifestations. The eye can be affected by the disease, with risk of retinal hemorrhage and sudden loss of vision (5%).1 Ocular signs and symptoms include cotton wool spots (soft exudates), microaneurysms and vascular tortuosity in the retina, photophobia, dry eye syndrome, pain, red eye and even complete loss of vision.1 The pharmacological treatment of SLE can alter significantly the visual field and color vision.2 Several authors have reported a slight increase of the color threshold (specially for yellow),3 retinopathy induced by hydroxychloroquine intake generating slight changes in color vision and the presence of a paracentral scotoma,4 and retinopathy induced by chloroquine intake.5 Multichannel perimetry6–8 is a relatively new clinical tool that allows the clinician to measure the contrast sensitivity for the magno, parvo, and koniocellular pathways, with the possibility of detecting incipient alterations in each of these visual pathways that could be not detected in a conventional perimetric exam. We report the first case of SLE in which visual alterations were evaluated with multichannel perimetry.
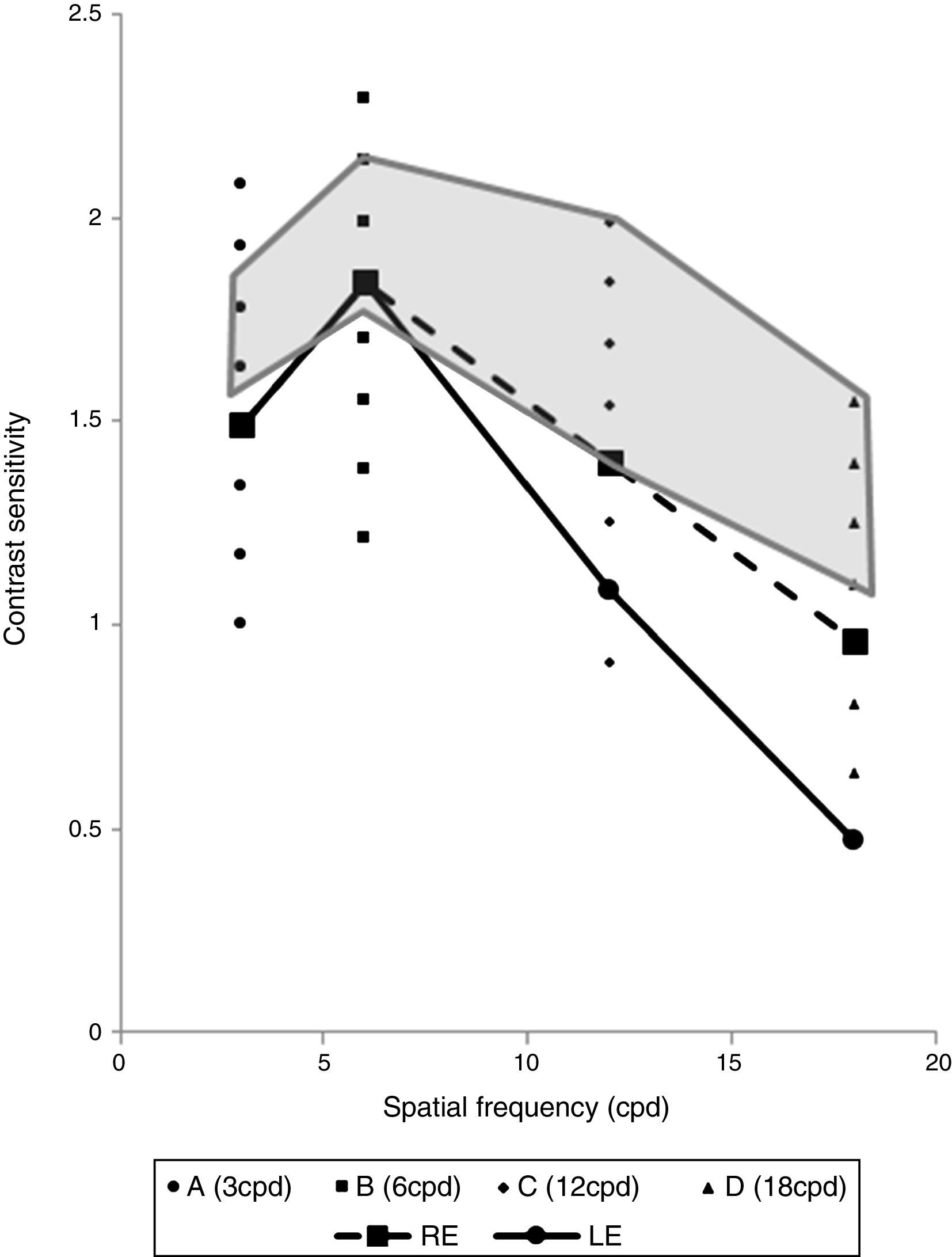
Case reportWe report the case of a visually asymptomatic 46-year old woman diagnosed with SLE and under treatment with hydroxychloquine during 15 years (hydroxychloroquine 200mg/day). The right eye (RE) had a manifest refraction of −1.00D and corrected distance visual acuity (CDVA) of 20/20. The left eye (LE) had a manifest refraction of (+4.00) (−1.75) 20° and CDVA of 20/25. Intraocular pressure was 12.7 and 13.3mmHg in RE and LE, respectively. Alterations were not detected either in the fundoscopic examination, 10-2 automated perimetry or in the examination of the macular structure by optical coherence tomography (Soct copernicus HR, Optopol). The results of the color vision examination (FM 100 Hue test) showed total and partial error score out of the range of normality for both eyes (RE: TES-128, RG-34, BY-94; LE: TES-144, RG-72, BY-72). The error value in the red-green (RG) axis was worse in LE, whereas the error value in the blue-yellow (BY) axis was worse in RE. Regarding the evaluation of the achromatic contrast sensitivity, a decrease in the contrast sensitivity function (CSF) was observed in both eyes for high spatial frequencies that was more significant in LE (Fig. 1). Besides these tests, visual perimetry was performed with a multichannel perimeter,6–8 selecting the following channels and frequencies to be examined9,10:
- •
Achromatic channel of magnocellular origin (A): spatio-temporal sinusoidal patterns of 0.5 cycles/degree flickering at 25Hz.
- •
Parvocellular red-green channel (RG): 0.5cycles/degree and 0Hz.
- •
Koniocellular blue-yellow channel (BY): 0.5cycles/degree and 0Hz.
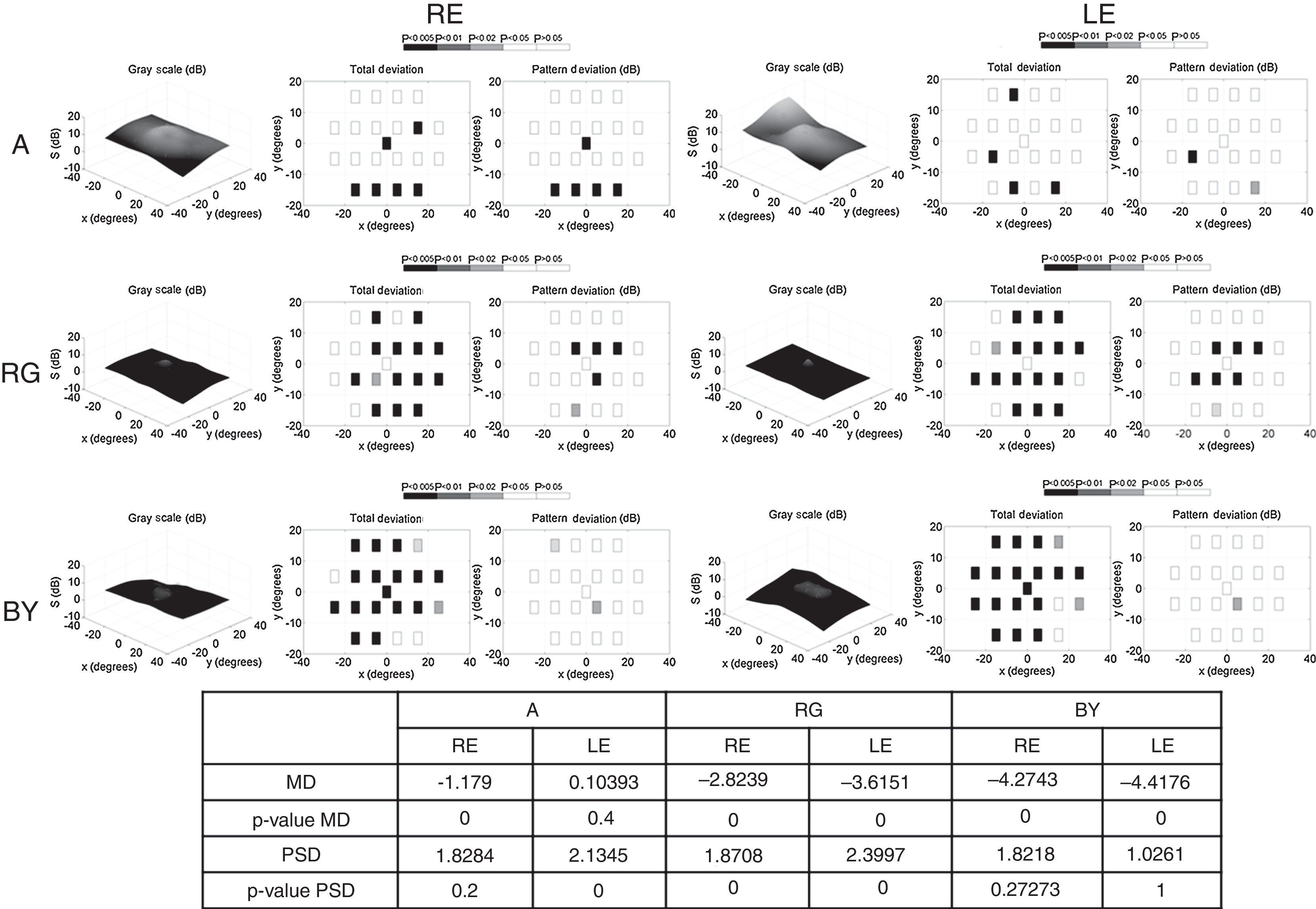
The results of this test for RE and LE are displayed in Fig. 2.
Results obtained with the multichannel perimetry. Top: maps of sensitivity (left), total deviation (center) and pattern deviation (right) for each eye and mechanism: achromatic (A), red-green (RG) and blue-yellow (BY). Bottom: statistical values for each mechanism: the medium defect (MD) and pattern standard deviation (PSD) are shown as well as the statistical significance (p-value) of the comparison with the normal healthy pattern.
All these visual alterations suggest a very incipient hydroxychloroquine maculopathy, with no OCT or 10-2 automated perimetry alterations. This information was sent to the rheumatologist who decided to discontinue the treatment.
DiscussionMultichannel perimetry measures the detection thresholds in a horizontal field of 60°×40°, centered at the fovea, and at a viewing distance of 25cm. It allows the clinician to detect incipient alterations in magno-, parvo-, and koniocellular pathways that cannot be detected in a conventional perimetric exam. To this date, this technology has been reported to detect impairment in the achromatic and RG and BY chromatic mechanisms in a case of essential tremor and in Alzheimer.11,12
The alterations detected in the achromatic channel with multichannel perimetry were not consistent with the CSF outcomes, as expected. The stimuli during the measurement of the CSF facilitate the response of the achromatic parvocellular channel, whereas the high temporal frequency in the multichannel perimetry estimulates the response of the magnocellular channel. Our results confirm the different behavior of these mechanisms in the patient evaluated. In our case, the multichannel perimetry detected significant losses of sensitivity in RE whereas the CSF showed data values with more departures from normality in LE. Furthermore, losses were not only detected in fovea, but also in the inferior portion of the visual field. These parafoveal losses may be the consequence of the adverse effect of the pharmacological treatment. The intake of hydroxychloroquine for SLE has been associated with a reduced parafoveal retinal sensitivity13 potentially due to an early damage of the ganglion cells and their photoreceptors of this region.5,14 This evidence is the first showing the presence of these visual alterations in a potential case of hydroxychloroquine maculopathy in SLE.
Concerning the color vision, we can observe in Fig. 2 that there was a significant decrease in retinal sensitivity compared to the normal pattern for red-green (RG) and blue-yellow (BY) channels in both eyes. The PSD values confirm that localized losses detected were statistically significant for the RG channel in both eyes. The sensitivity losses detected in the chromatic channels in the central zone of the visual field were consistent with the results of the FM 100 Hue color test. Likewise, the multichannel perimetry detected sensitivity losses in the parafoveal area for both chromatic channels, especially for the BY. Future studies should confirm if these parafoveal alterations are consistent with the defects detected by microperimetry in cases of hydroxychloroquine toxicity and if the chromatic changes are more incipient than microperimetric signs. Likewise, future studies should confirm if these multichannel perimetric alterations are also related to changes in fundus autofluorescence and multifocal electroretinogram that have been also shown to be useful in the detection of hydroxychloroquine maculopathy.15
In conclusion, some achromatic and color vision alterations may be present in incipient stages of hydroxychloroquine maculopathy in SLE. Future studies should investigate if these color vision alterations detected by means of multichannel perimetry may be used for the detection of incipient stages of SLE or incipient hydroxychloroquine toxicity when treated cases are analyzed.
Conflicts of interestThe authors have no financial or proprietary interest in a product, method, or material described herein. The study adheres to the tenets of the Declaration of Helsinki for Research Involving Human Observers and the project was approved by the ethics committee of the University of Alicante.