To report a 36-year-old patient with intraocular lens (IOL) subluxation that was followed for IOL stability with evaluation of images captured with the iTrace combined aberrometer/topographer.
MethodsThe patient had undergone phacoemulsification with IOL implantation for congenital cataract 15years before. He presented with bilateral IOL subluxation, more severe in his right eye. Right eye was operated for IOL exchange and left eye was followed with the iTrace images. The images were captured with an infrared camera, and the pupil, the pupil center and the corneal vertex could be detected. The subluxated IOLs edge was visible through infrared light retroillumination. IOL position was evaluated with respect to the pupil, the pupil center and the corneal vertex.
ResultsThe patient's left eye was followed for 7 months, and IOL position was noted to be stable. Thus no intervention was planned.
ConclusionEvaluation of iTrace images is a reliable method to follow eyes with IOL subluxation.
Mostrar el caso de un paciente de 36 años con subluxación de lentes intraoculares (LIO), al que se realizó un seguimiento de estabilidad de LIO con evaluación de imágenes captadas con el sistema iTrace, el cual combina un aberrómetro y un topógrafo.
MétodosEl paciente había sido sometido a una facoemulsificación con implante de LIO debido a una catarata congénita 15 años antes. Presentaba una subluxación bilateral de LIO, más severa en su ojo derecho. Se realizó en el ojo derecho una reposición de la LIO, mientras que al el ojo izquierdo se le realizó un seguimiento mediante imágenes del iTrace. Se captaron las imágenes con una cámara de infrarrojos, pudiéndose determinar la pupila, el centro de la pupila y el vértice corneal. El borde de la LIO subluxada fue visible mediante la retroiluminación con luz infrarroja. Se evaluó la posición de la LIO con respecto a la pupila, el centro de la pupila y el vértice corneal.
ResultadosSe realizó un seguimiento del ojo izquierdo del paciente durante siete meses, comprobándose que la posición de la LIO era estable. No se planificó, por tanto, ninguna otra intervención.
ConclusiónLa evaluación mediante imágenes del iTrace constituye un método fiable para el seguimiento de los ojos con subluxación de LIO.
Posterior chamber intraocular lens (PC-IOL) subluxation is an infrequent complication of cataract surgery and IOL implantation, which can cause significant visual disturbance to the patient. It can occur either in the early postoperative period, or several months or years postoperatively. Etiologies are inadequate capsular support, progressive zonular dehiscence or trauma amongst others.1–3 In order to confirm the stability of the IOL position, close follow up of these patients is necessary. The most common method to follow IOL position is evaluation by slit lamp photography. We report a patient with bilateral IOL subluxation that was followed with images captured with the iTrace aberrometer/topographer (Tracey Tech, Houston, TX).
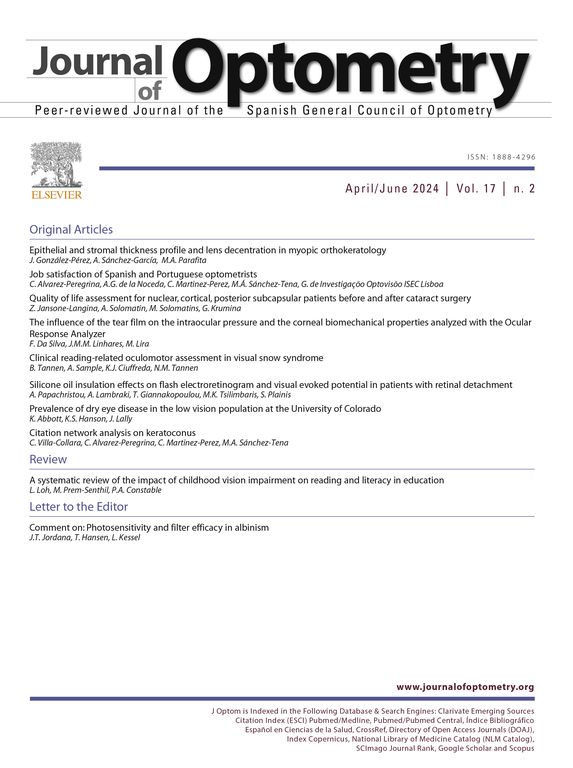
Case reportA 36-year-old male presented with visual deterioration in his right eye for the past 10days. The patient had undergone phacoemulsification and PC-IOL implantation 15years back for congenital cataract and high myopia in both eyes. Four years back, he had undergone YAG laser capsulotomy for posterior capsule opacification bilaterally. At presentation, corrected distance visual acuity (CDVA) in his right eye was 20/50 with manifest refraction of −1.00–4.00×95°, and in his left eye CDVA was 20/25 with manifest refraction of −3.50–2.00×80°. Slit lamp examination revealed PC-IOL subluxation bilaterally, more severe in his right eye. The iTrace was used to assess the relative position of the IOL with the pupil, the pupil center and the corneal vertex (Figs. 1 and 2a).
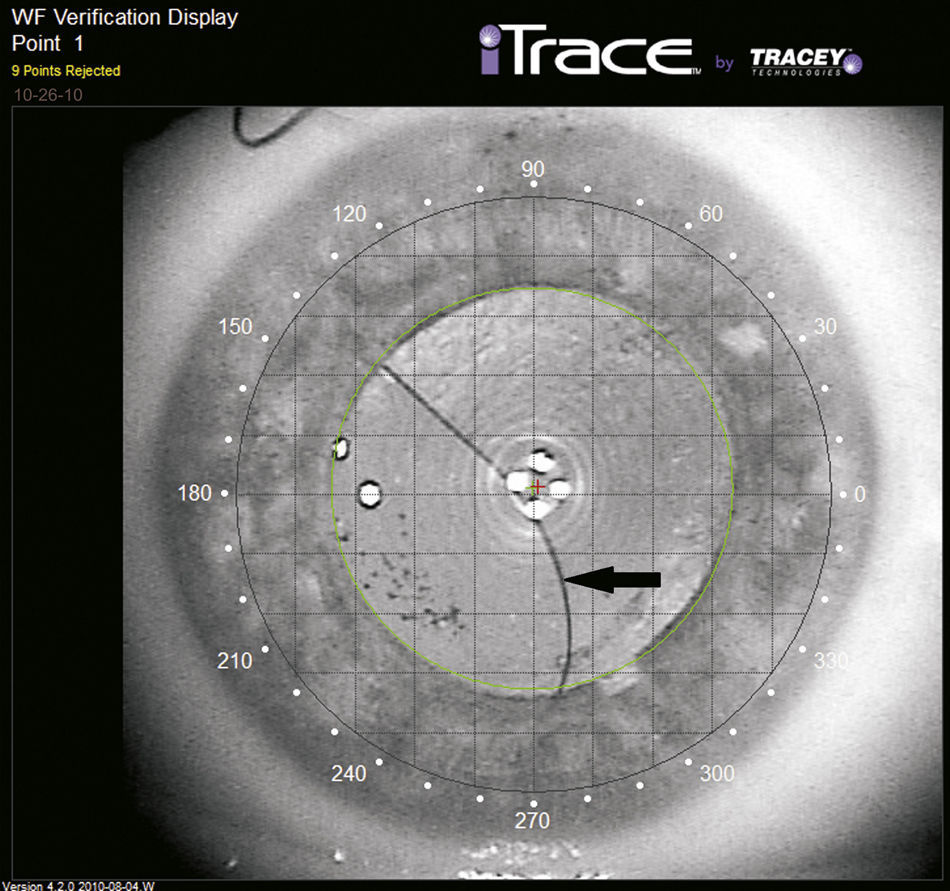
Images captured with the iTrace showing the IOL position with respect to the pupil center (green cross) and the corneal vertex (red cross) of the left eye: (a) first visit, (b) 4-month follow up, (c) 7-month follow up. White arrow shows the edge of IOL. IOL position is stable when compared to the reference points.
An IOL exchange was planned and performed after 1 month for the right eye, while for the left eye it was proposed to repeat examination in order to evaluate if IOL subluxation was progressive. Six months postoperatively CDVA in right eye was 20/20 with manifest refraction of +1.50–3.00×90° and CDVA in left eye was 20/25 with manifest refraction of −3.25–2.50×125°. Assessment of the IOL position was repeated with the iTrace 4 and 7months after first visit (Fig. 2). Evaluation of the IOL position was assisted by the instrument software, which shows the distance in mm and the angle distance of the pointer position on the image from the image center. Image center coincides with pupil center when measurement of aberrations is centered in the pupil. IOL position was stable in the left eye, as evaluated with respect to the pupil center and the corneal vertex in the eye images of the iTrace. As a result, no intervention was planned.
DiscussionIntraocular lens subluxation/dislocation is a potentially progressive condition that can occur even in the late postoperative period after cataract surgery and IOL implantation. This postoperative complication can lead to significant deterioration of the patient's visual acuity, and symptoms such as monocular diplopia, glare and haloes. When visual disturbance is significant, surgical management is required. Treatment consists of IOL reposition or replacement, with additional measures such as scleral suturing, whenever needed in order to avoid recurrence.1–6 In cases where no treatment is undertaken, close follow up with observation is required in order to confirm the stability of the IOL position.2,4 In our patient we decided to operate only on the right eye and to follow up the left eye in order to evaluate stability.
Follow up on such eyes is usually done by evaluation with slit lamp photography. This technique, albeit very useful, has a few limitations. A limitation of slit lamp photography is the difficulty to repeat depiction with the patient fixating at the same reference point each time. In addition, evaluation of the IOL position with respect to the pupil is difficult, as the pupil usually does not have the same diameter in each depiction. More significantly, in slit lamp photo there is no reference to pupil center and visual axis of the patient, which are optically significant reference points with regard to the IOL position. Other techniques that have been proposed for evaluation of IOL subluxation are ultrasound biomicroscopy7 and anterior segment optical coherence tomography (AS-OCT).8 Both are useful in studying the anatomical relationship of the subluxated IOL with the ocular structures. They also have the advantage of visualization of IOL tilt, but it is difficult to achieve same cross-sectional images for follow up of stability. Additionally, there is no reference on pupil and visual axis.
When measuring ocular aberrations with the iTrace aberrometer, eye image is captured with an infrared camera, while having the patient fixated at the instrument's target. The pupil center and corneal vertex can be automatically or manually detected. The IOL position is noted in the image due to the retroillumination of the infrared light, which is captured by the instrument's camera. The position can be evaluated with respect to the pupil center and corneal vertex, which is a close approximation of the intersection of the visual axis at the corneal plane.9 In our case the stability of the IOL position in the left eye of the patient was evident in the images captured with the iTrace through duration of 7 months follow up, and that was in accordance with the stability of the patient's visual acuity and refraction.
All instruments that provide retroillumination images with infrared light can be used for the evaluation of the position of dislocated IOLs. In a previous study, Rosales and Marcos10 used infrared retroillumination images provided by a custom-made ray-tracing laser system to evaluate IOL decentration with respect to the pupil.
In conclusion, evaluation of images captured with the iTrace or other systems with similar capabilities, whenever available, is a reliable method for follow up of IOL subluxation, with additional information on the relative position of the IOL in relation to optically significant reference points.
Financial supportNone.
Conflict of interestsDr. Pallikaris has a financial interest in Tracey Technologies, Inc. None of the other authors has a proprietary or commercial interest in any material discussed.