Describe surgical treatment and results in a group of patients diagnosed and operated on of fat adherence syndrome following inferior oblique surgery.
Patients, material and methodsRetrospective study of 6 cases diagnosed and treated of fat adherence syndrome following inferior oblique surgery. Mean age was 24.67 years (range, 5–41), 3 males, 5 unilateral and 1 bilateral. Mean vertical deviation was 16.16pd (range, 4–25). Esotropia was associated in 4 cases, diplopia in other 2, and anomalous head posture in 3. A good outcome was considered when the final deviation was less than 10pd, with mild limitation of elevation, without anomalous head posture, and a negative duction forced test.
ResultsThe final vertical deviation was 6.83pd (range, 0–14). A 2–4mm inferior rectus recession was performed on 4 patients associated to an inferior oblique surgery/exploration. All patients were operated on once, except 1 case. A good outcome was achieved in 3 patients. Anomalous head posture was resolved in 2 of 3 cases. Diplopia resolved after surgery. Only one case achieved orthophoria. Mean evolution time was 34.83 months (range, 6–78).
ConclusionIn the treatment of the fat adherence syndrome, an inferior rectus recession is recommended, associated to inferior oblique exploration or surgery. A good favorable outcome was only achieved in half of the cases with surgical treatment. Limitation of elevation could not be completely resolved in any of the patients.
Describir el tratamiento quirúrgico y los resultados en un grupo de pacientes con diagnóstico de síndrome de adherencia grasa tras una cirugía de oblicuo inferior.
Pacientes, material y métodosEstudio retrospectivo de 6 casos diagnosticados y tratados de síndrome de adherencia grasa tras una cirugía de oblicuo inferior. La edad media fue de 24,67 años (rango, 5–41), 3 varones, 5 cirugías unilaterales y 1 bilateral. La desviación vertical media fue de 16,16 dioptrías prismáticas (rango, 4–25). Se asoció esotropía en cuatro casos, diplopía en dos, y Tortícolis en tres. Se consideró un buen resultado cuando la desviación final fue inferior a 10pd, con leve limitación de la elevación, Tortícolis, y resultado negativo en el test de ducción forzada.
ResultadosLa desviación vertical final fue de 6,83pd (rango, 0–14). Se realizó una recesión del músculo recto inferior de 2 a 4mm en cuatro pacientes, asociada a una cirugía/exploración del oblicuo inferior. A todos los pacientes se les intervino una sola vez, exceptuando un único caso. Se logró un buen resultado en tres pacientes. La postura de cabeza anómala se resolvió en dos de tres casos. La diplopía se resolvió tras la intervención. En un único caso se logró ortoforia. El tiempo medio de evolución fue de 34,83 meses (rango, 6–78).
ConclusiónEn el tratamiento del síndrome de adherencia grasa se recomienda la recesión del músculo recto inferior, asociada a una exploración o cirugía del oblicuo inferior. Se logró un resultado favorable y bueno únicamente en la mitad de los casos con tratamiento quirúrgico. La limitación de la elevación no pudo resolverse completamente en ninguno de los pacientes.
The fat adherence syndrome, described by Parks, is a rare but serious complication that causes a restrictive ocular motility disorder.1 There are no actual figures of its incidence, but according to Parks it is 13% after performing inferior oblique myectomy and 2% after its detachment.2
The syndrome is caused by disruption of the orbital fat during inferior oblique muscle or scleral buckling surgery, and in rare cases secondary to infection, trauma or blepharoplasty.3–6 Clinical features are progressive hypotropia of the affected eye, limitation of the elevation (specially in abduction), a very positive forced duction test and an upper lid retraction.1
There are other situations following inferior oblique surgery causing limitation of elevation, such as the inferior oblique inclusion syndrome and the anti elevation syndrome.3,7–9
As preventive measures, damaging the posterior Tenon capsule must be avoided during inferior oblique surgery. However, since the current cause is still unknown, it is not always possible to correlate this disorder with a bad surgery.3,10 Published papers on the use of antimetabolites are controversial as they can worsen the inflammation and increase the restriction.1,11,12
The treatment is surgical, but difficult, and the recurrence rate is high.1
Subjects, material and methodsThe purpose of this article is to describe the treatment and results of the fat adherence syndrome in a series of patient who underwent strabismus surgery.
We conducted a retrospective study of 6 patients diagnosed and treated of fat adherence syndrome after prior inferior oblique muscle surgery between 1998 and 2012. Patients with clinical suspicion of fat adherence syndrome were included (hypotropia, positive forced duction test and limitation of elevation). Cases of doubtful differential diagnosis with antielevation syndrome and cases that were not operated on were excluded.
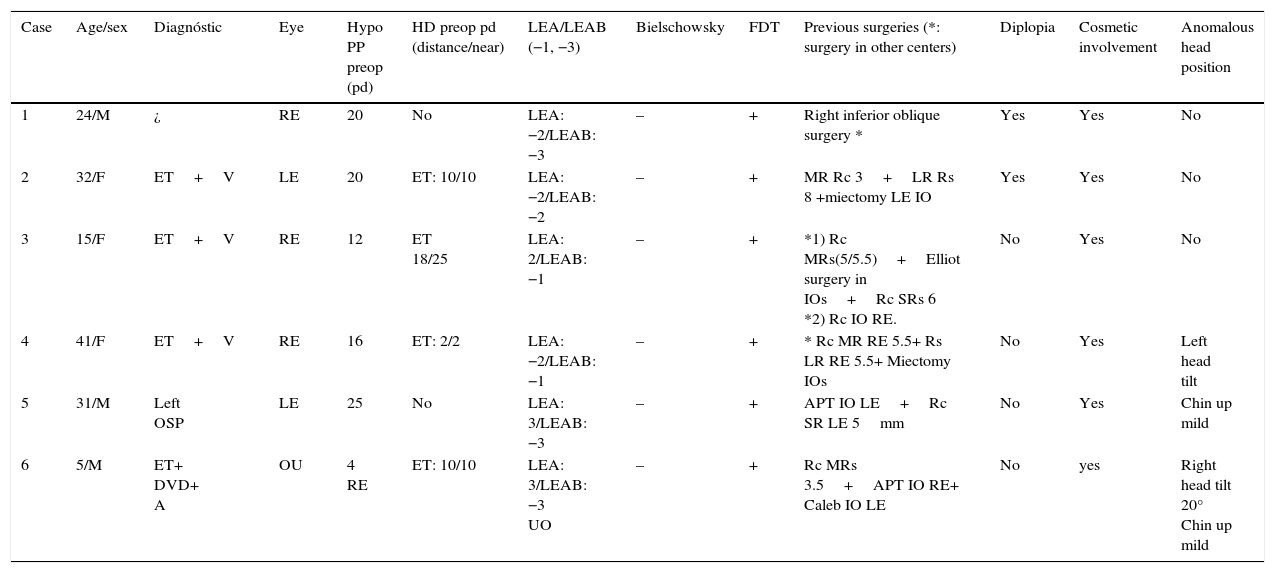
The data collected from the patients’ medical records included age, sex, affected eye and initial diagnosis. The preoperative examination included alternate prism and cover testing in the primary position of gaze. The limitation of the elevation in adduction and abduction was classified from −1 (mild) to −3 (severe). The forced duction test was performed in the operating room prior to surgery and confirmed the diagnosis. The type and number of surgeries that were performed previously, the presence of diplopia, cosmetic involvement and the abnormal head posture were recorded and summarized in Table 1.
Clinical data.
| Case | Age/sex | Diagnóstic | Eye | Hypo PP preop (pd) | HD preop pd (distance/near) | LEA/LEAB (−1, −3) | Bielschowsky | FDT | Previous surgeries (*: surgery in other centers) | Diplopia | Cosmetic involvement | Anomalous head position |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 24/M | ¿ | RE | 20 | No | LEA: −2/LEAB: −3 | – | + | Right inferior oblique surgery * | Yes | Yes | No |
| 2 | 32/F | ET+V | LE | 20 | ET: 10/10 | LEA: −2/LEAB: −2 | – | + | MR Rc 3+LR Rs 8 +miectomy LE IO | Yes | Yes | No |
| 3 | 15/F | ET+V | RE | 12 | ET 18/25 | LEA: 2/LEAB: −1 | – | + | *1) Rc MRs(5/5.5)+Elliot surgery in IOs+Rc SRs 6 *2) Rc IO RE. | No | Yes | No |
| 4 | 41/F | ET+V | RE | 16 | ET: 2/2 | LEA: −2/LEAB: −1 | – | + | * Rc MR RE 5.5+ Rs LR RE 5.5+ Miectomy IOs | No | Yes | Left head tilt |
| 5 | 31/M | Left OSP | LE | 25 | No | LEA: 3/LEAB: −3 | – | + | APT IO LE+Rc SR LE 5mm | No | Yes | Chin up mild |
| 6 | 5/M | ET+ DVD+ A | OU | 4 RE | ET: 10/10 | LEA: 3/LEAB: −3 UO | – | + | Rc MRs 3.5+APT IO RE+ Caleb IO LE | No | yes | Right head tilt 20° Chin up mild |
Hypo: hypotropia; preop: preoperative; HD: horizontal deviation; LEA: limitation to elevation in adduction; LEAB: limitation to elevation in abduction; FDT: duction forced test; M: male; F: female; ET: endotropia; V: V pattern; A: A pattern; OSP: oblique superior palsy; RE: right eye; LE: left eye; pd: prism diopters; MR: medial rectus; LR: lateral rectus; Rc: recession; Rs: resection; IO: inferior oblique; SR: superior rectus.
Mean age of the sample was 24.67 years (SD: 12.97 years; range, 5–41 years), 3 men and 3 females. Of the 6 cases, 5 were unilateral and 1 was bilateral.
Mean vertical deviation was 16.16pd (SD: 7.39pd; range, 4–25pd); 18.6pd (SD: 4.88pd; range, 12–25pd) excluding the bilateral case. In 4 cases there was an associated esotropia, 2 had diplopia, and 3 had abnormal head posture. All of them wanted to improve their cosmetic appearance.
Treatment was considered successful if a final vertical deviation was less than 10pd in primary position of gaze, with an improvement of elevation to a −1 degree, and the abnormal head posture and forced duction test were resolved.
The study was performed in accordance with the principles set out in the Declaration of Helsinki.
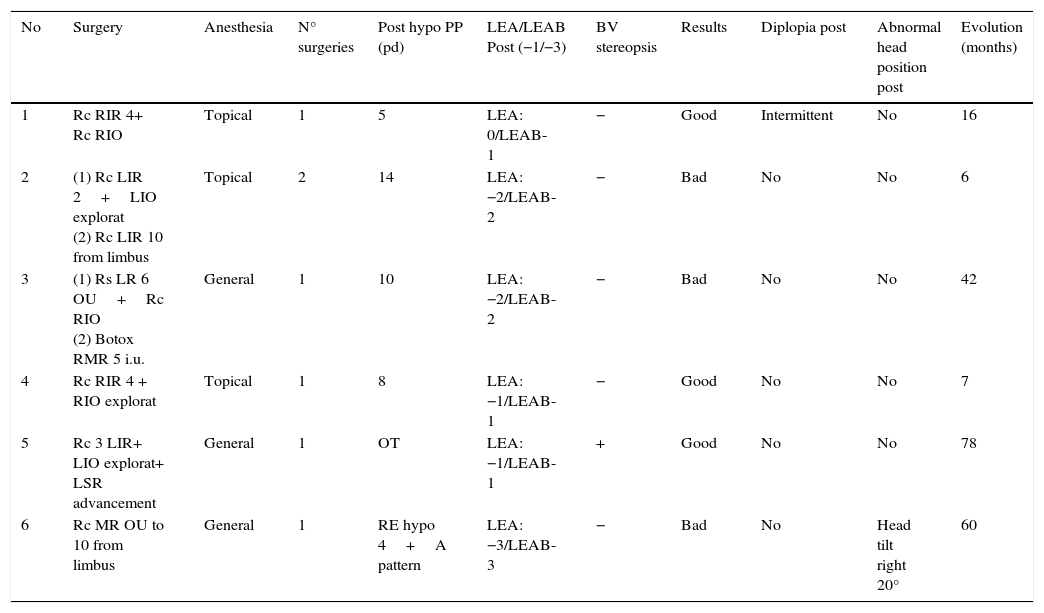
ResultsMean final hypotropia was 6.83pd (SD: 4.91pd; range, 0–14pd); 7.4pd (SD: 5.27pd; range, 0–14pd) excluding the bilateral case. The surgeries performed to treat motor and cosmetic involvement relating to adherence syndrome are described in Table 2. Our approach was to perform an inferior rectus muscle recession 2–4mm, associated to an inferior oblique exploration or surgery in 4 cases.
Treatment and results.
| No | Surgery | Anesthesia | N° surgeries | Post hypo PP (pd) | LEA/LEAB Post (−1/−3) | BV stereopsis | Results | Diplopia post | Abnormal head position post | Evolution (months) |
|---|---|---|---|---|---|---|---|---|---|---|
| 1 | Rc RIR 4+ Rc RIO | Topical | 1 | 5 | LEA: 0/LEAB-1 | − | Good | Intermittent | No | 16 |
| 2 | (1) Rc LIR 2+LIO explorat (2) Rc LIR 10 from limbus | Topical | 2 | 14 | LEA: −2/LEAB-2 | − | Bad | No | No | 6 |
| 3 | (1) Rs LR 6 OU+Rc RIO (2) Botox RMR 5 i.u. | General | 1 | 10 | LEA: −2/LEAB-2 | − | Bad | No | No | 42 |
| 4 | Rc RIR 4 + RIO explorat | Topical | 1 | 8 | LEA: −1/LEAB-1 | − | Good | No | No | 7 |
| 5 | Rc 3 LIR+ LIO explorat+ LSR advancement | General | 1 | OT | LEA: −1/LEAB-1 | + | Good | No | No | 78 |
| 6 | Rc MR OU to 10 from limbus | General | 1 | RE hypo 4+A pattern | LEA: −3/LEAB-3 | − | Bad | No | Head tilt right 20° | 60 |
Post hypo PP: postoperative hypotropia in primary position; pd: prismatic diopters; LEA: limitation to elevation in adduction; LEAB: limitation to elevation in abduction; BV: binocular vision; Rc: recession; RIR: right inferior rectus; RIO: right inferior oblique; LIR: left inferior rectus; LIO: left inferior oblique; Explorat: exploration; Rs: resection; LR: lateral rectus; RMR: right medial rectus; LSR: left superior rectus; MR: medial rectus.
In case no. 3, only surgery in the inferior oblique was performed because the medial and superior recti muscles had been operated on previously (Table 2). Because this patient had a residual esotropia, both lateral recti resection were performed, so we considered not to operate on the inferior rectus to prevent an anterior segment ischemia syndrome. Subsequently Botox® (Allergan, Inc, Irvine, California, USA) was injected into right medial rectus (5 i.u.).
In case no. 6, both inferior recti were not operated on because a severe A-pattern (it would worsen following the inferior recti muscles recession) was associated. A further recession of the medial recti was performed to treat the residual esotropia and improve abnormal head posture. In case no. 2, the inferior rectus was recessed 2mm, resulting in a postoperative undercorrection that required a further increased recession. In case no. 5, a 5mm-left superior rectus recession and Apt of the left inferior oblique had been performed to treat a left superior oblique paresis. At two-weeks post-operative visit, the patient showed a progressive hypotropia, severe limitation of elevation in both abduction and adduction (−3), chin up position and a very positive forced duction test in the elevation. The condition resolved after a 3mm-left inferior rectus recession associated to left superior rectus advancement to its original insertion.
During surgeries, topical anesthesia was used in 3 cases and general in other 3. Only one operation was performed in all cases except in no. 2, which was operated on twice to treat the adherence syndrome. The outcomes were good in 3, but only 1 case (no. 5) had orthophoria. The abnormal head posture resolved in 2 of the 3 patients. Diplopia resolved after surgery, although 1 patient complained of intermittent post-operative diplopia (case no. 1). In none of the cases the limitation of the elevation was resolved completely, but patients with a good outcome were associated with less limitation of the supraduction (−1), while cases with poor outcome had a more severe limitation of the elevation (−2 and −3). Final binocular vision and stereopsis were only presented in 1 case (case no. 5). Mean evolution time from the adherence syndrome surgery until data collection was of 34.83 months (SD: 30.02 months; range, 6–78 months).
DiscussionInferior oblique surgery may have post-operative complications causing hypotropia with limitation of the elevation, such as fat adherence, inferior oblique adherence and antielevation syndromes.1,12 The inferior oblique inclusion syndrome is another complication that occurs after lateral rectus surgery (especially resection) though the ocular motility disorder is not common because the path of the inferior oblique is not changed. Therefore the patients have minimal hypotropia or may even have hypertropia.1 In this small series of 6 cases the median hypotropia in primary gaze position was 16.16±7.39pd, similar to other studies.12
Fat adherence syndrome is described primarily as a complication of any inferior oblique surgery12 unlike the anti-elevation syndrome following inferior oblique anteriorization that makes this muscle into depressor.13,14 The actual incidence of fat adherence syndrome is currently unknown.1 The differential diagnosis between the anti-elevation and the fat adherence syndrome may be confusing because both share some characteristics. Nevertheless, there are some differences. First, the adherence syndrome happens after any inferior oblique or scleral buckling surgery, trauma, and blepharoplasty.1,5,12,15 The forced duction test is more positive in the adherence syndrome than in the anti-elevation, where only a slight resistance is found in the temporal superior direction.7 Finally, the deviation progressively worsens in the adherence syndrome and may occur later than in the anti-elevation (earlier onset and a stable deviation).16 In our series of 6 cases were all diagnosed of adherence syndrome because surgery performed on the inferior oblique had been variable [in one case (no. 1) was unknown and in another an anterior transposition was performed in only one eye while the limitation of elevation occurred in both (case 6)]. The forced duction test was very positive in all 6 cases.
Preventive measures are difficult since the current cause is still unknown.1,3,12 Some have speculated that vomiting and coughing may facilitate their development in the presence of a damaged Tenon's capsule.2
Surgical indications include correcting vertical deviation, eye elevation, abnormal head posture, diplopia, and improving the cosmetic appearance.12 All of our cases had a vertical deviation, limitation of elevation, and a cosmetic involvement, 3 with abnormal head posture and 2 with diplopia. Fat adherence syndrome treatment is difficult and a good outcome is not always achieved.1,2,12,17 Exploration of the inferior oblique is mandatory to release adhesions, to avoid recurrences and to improve eye elevation. Other surgeries imply inferior oblique reposition, or cutting muscle fibers remnants that had been left in previous surgeries.1 However, according to other studies, it is necessary to associate the inferior rectus recession to resolve its contracture secondary to hypotropia and to achieve a good outcome.1 Some authors also perform a 180° conjunctival peritomy, recessing the conjunctiva and leaving the sclera to re-epithelialise.12 In this small sample of 6 cases an inferior rectus surgery was performed in 4, 3 of them with good outcome. Recession varied between 2mm and 4mm, although the case where only 2mm inferior rectus recession was performed remained undercorrected and a further surgery was required. Inferior recti were not operated on in two cases (1 for high risk of anterior segment ischemia and another because of a potentially worsening A–pattern) and both had poor outcome. The limitation of elevation was not completely resolved in any patient. Patients’ expectations of strabismus surgery are often unrealistic. Resetting their expectations is therefore important, but it can be a challenging issue.
Some authors reported good results with repeated injections of botulinum toxin in the inferior rectus in the acute phase of the disease.2,17 However, there are few publications validating and recommending its use.
Our study is limited by its retrospective design (some data were not included in all the clinical histories, such as the excyclotorsion and the reports of previous surgeries operated on in other centers) and the small number of patients. (Adherence syndrome is a rare condition and not easily diagnosed.)
In conclusion, inferior rectus recession is strongly recommended to treat the fat adherence syndrome associated to an inferior oblique muscle exploration. However, in our series, surgery was successful only in half of the cases with fat adherence syndrome, and the ocular motility disorder could not be completely resolved.
Conflicts of interestThe authors have no conflicts of interest to declare.
This work was presented as an oral communication in the Meeting of the Spanish Society of Strabismus, Cuenca, April 24th to 26th, 2014.