To evaluate the demographic profile, refraction, visual acuity (VA), corneal curvature (K) and severity of keratoconus (KC) patients from a cornea specialist centre in Malaysia. This may improve the management of KC patients in this country.
MethodsRecords of 13,000 patients were reviewed. The patients were categorized into 4 age groups: (Gp 1: <23 years, Gp 2: 23–32 years, Gp 3: 33–42 years, Gp 4: >42 years). Refraction and VA were determined using subjective refraction and Snellen chart. Corneal curvature was measured using Orbscan II topography. Severity of KC was graded following Amsler–Krumeich system. Data were analysed according to age, gender and ethnicity.
ResultsA total of 159 patients had KC and the prevalence was 1.2%. Mean age of onset was 20.9±5.6 years, with 71.1% of males and 28.9% of females. Majority were of Indian and Malay origins. Percentages of patients within each age group were 26.4%, 52.8%, 18.9% and 1.9% respectively. Regarding severity, 37.6% were stage I, 30.1% stage II, 4.4% stage III and 27.8% stage IV at the time of diagnosis. The age of onset, refraction, mean K and VA was found to be similar between gender and ethnicity (p>0.05). Age of onset was not strongly correlated to the severity of the disease.
ConclusionThis study concludes that there are higher percentages of Malays and Indians with KC than other races in Malaysia. The condition was found to manifest at a younger age and was more common in males than females. These findings should be considered during vision screening in Malaysia.
Evaluación del perfil demográfico, refracción, agudeza visual (AV), curvatura corneal (K) y severidad de los pacientes de queratocono por en de un centro especializado en Malasia. Los hayazgos de este trabajo podrán mejorar el tratamiento de dichos pacientes de en ese país.
MétodosSe revisaron las historias clínicas de 13.000 pacientes. Dichos pacientes se clasificaron conforme a 4 grupos de edad: (Grupo 1: <23 años, Grupo 2: de 23 a 32 años, Grupo 3: de 33 a 42 años, Grupo 4: >42 años). La refracción y la AV se determinaron utilizando la el procedimiento de refracción subjetiva y los optotipos de Snellen. La curvatura corneal se midió utilizando un topógrafo Orbscan II. La severidad del queratocono se clasificó mediante el sistema Amsler-Krumeich. Los datos fueron analizados de acuerdo a edad, sexo y etnicidad.
ResultadosUn total de 159 pacientes padecían queratocono, con una prevalencia del 1,2%. La edad media de aparición era de 20,9±5,6 años, con un porcentaje del 71,1% de varones y un 28,9% de mujeres. La mayoría era de procedencia india y malaya. Los porcentajes en cada grupo de edad fueron: 26,4%, 52,8%, 18,9% y 1,9% respectivamente. En cuanto a la severidad, 37,6% se presentaron en estadio I, 30,1% en estadio II, 4,4% en estadio III y 27,8% en estadio IV en el momento del diagnóstico. La edad de aparición, refracción, K media y AV era similar en cuanto a sexo y etnicidad (p>0,05). La edad de aparición no estaba fuertemente ligada a la severidad de la enfermedad.
ConclusionesEste estudio concluye que existen mayores porcentajes de malayos e indios con queratocono que en otras razas en Malasia. Se ha constatado que dicha situación se manifiesta a edad muy temprana, siendo más común en varones que en mujeres. Dichos hallazgos deberán considerarse durante los exámenes visuales en Malasia.
Keratoconus is a non-inflammatory, self limiting ectasia of the cornea, characterized by a progressive thinning and steepening. The aetiology of the disease remains unknown, although there is evidence of genetic inheritance and possible linkage with systemic disease and circumstantial evidence that certain behaviours, such as excessive eye rubbing and contact lens wear, may be associated with the disease.1,2
The reported incidence of keratoconus varies between countries with most estimates being between 50 and 230 per 100,000 in general population (approximately 1 per 2000 to 1 per 500).3,4 Variation in the incidence of keratoconus suggests the possibility of genetic factor involvement in the aetiology. Earlier studies reported that compared to Caucasian eyes, Asians had 4-fold increase in incidence, were younger at presentation and required corneal grafting at earlier age.5,6 A relatively high incidence has been documented in the Mediterranean and Middle Eastern areas; a relatively lower incidence has been reported in places such as Japan and Taiwan.7,8 In India, the prevalence of KC amongst individuals aged 30 years and above and living in the rural region of Central India was found to be 2.3±0.2%.9 The prevalence was also found to be associated with lower body height, myopic refractive errors and thinner central cornea.9
Gender related differences are also believed to play a role in keratoconus.10 In a multicentre Collaborative Longitudinal Evaluation of Keratoconus (CLEK) study, Fink et al.11 reported that gender differences exist in the history, vision and ocular symptoms of keratoconus patients. In a study performed in New Zealand, men were reported to have earlier onset of keratoconus and experienced a more rapid disease course.12 In another study conducted at a specialist contact lens clinic in United Kingdom, approximately 60% of the 130 keratoconic patients were men.13
Awareness of the factors influencing the development of keratoconus is important in the prevention, diagnosis and management of the condition. This retrospective study was planned with the aim of understanding the demographic pattern of keratoconus in Malaysia with respect to age, gender and race. To the best of our knowledge this is the first reported data on keratoconus in Malaysia. It is possible that there are some ethnic variations in the incidence and development of keratoconus in the population. Understanding ethnic variations is important for the management within the South East Asian region so that early intervention can be provided and quality of life can be improved.
MethodsClinical records of 13,000 patients attending a cornea specialist clinic in Kuala Lumpur within 10 years were reviewed in this study. The diagnosis of keratoconus was based on slit lamp biomicroscopic findings (corneal stromal thinning, conical protrusion of the cornea at the apex, Fleischer ring, Vogt's striae and corneal scar) in at least one eye and corneal images generated by Orbscan II corneal topography system (Bausch and Lomb Surgical, Orbtek Inc., Salt Lake City, UT, USA). At least 3 best corneal images of each eye were obtained and analysed using printed colour coded axial maps with absolute scales in step of 1D and pachymetry maps in steps of 20μm. The topographic parameters that were analysed for the purpose of diagnosis include simulated keratometer readings, elevation points and the thinnest point pachymetry of the cornea.
Exclusion criteria included any patient with history of ophthalmic surgery or significant ophthalmic disease other than keratoconus. All eyes underwent a comprehensive ophthalmologic examination that included visual acuity measurements (using Snellen chart), manifest refraction (using retinoscopy and refined by subjective refraction), slit lamp biomicroscopy, corneal topography, tonometry and fundus examination. This study was approved by the Medical Ethics Committee of Universiti Kebangsaan Malaysia and followed the tenets of Declaration of Helsinki.
Keratoconus can be classified according to the shape of the cone, the severity level (based on central keratometric readings) or its progression. In this study, classification of keratoconus was based on central corneal curvature values measured by keratometric (K) readings following the Amsler–Krumeich grading system.14 Mean K was calculated automatically by the Orbscan II corneal topography system as the mean value of flattest and steepest central curvatures in the 3-mm zone. For the purpose of analysis, the subjects were categorized into 4 different age groups that is Group 1: <23 years, Group 2: 23–32 years, Group 3: 33–42 years and Group 4: >42 years. Results were evaluated using statistical analysis software (SPSS 15; SPSS Inc.). Normality of data in every group was tested using the normal probability plots. Student t test and one-way ANOVA were used to compare the means of parameters between gender and age groups respectively. The association between age with mean K and age with manifest refraction for every age group were calculated using Pearson correlation.
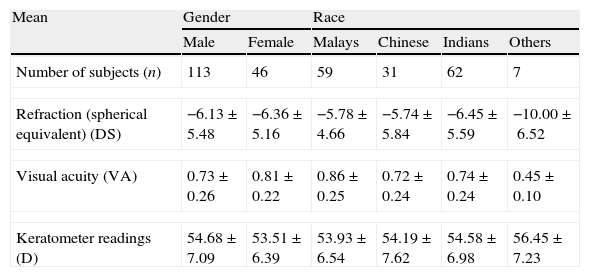
ResultsClinical records of 13,000 patients were reviewed. Demographic information of patients is presented in Table 1. The racial distribution was 50.5% Chinese, 20.8% Malays, 18.2% Indians and 10.5% others (mixed parentage, Caucasians and others). The mean age of the patients was 31.46±9.17 years (range, 5–80, median 40). A total of 159 patients were diagnosed as keratoconus. The prevalence was therefore 1.2%. One hundred and thirteen (113) of them were males and 46 were females. Mean age at the time of diagnosis was 21.46±6.17 (range, 9–38, median 29) years old, being 21.96±6.07 for males and 20.20±6.29 for females. No significant difference was detected in the mean age between genders (p=0.681). Around 77% of the cases were bilateral keratoconus. The measurements reported here were from the right eye only. Mean keratometer reading was 51.27±5.91D and mean steepest keratometer reading was 51.26±5.91D. Mean refraction in spherical equivalent was −6.19±5.37D and mean best corrected visual acuity (BCVA) was 0.75±0.25 (6/9 Snellen) (Table 1). The mean duration from diagnosis to the end of this study was 5.28±4.71 years.
Mean of measurements and distribution of keratoconus cases following gender and race.
| Mean | Gender | Race | ||||
| Male | Female | Malays | Chinese | Indians | Others | |
| Number of subjects (n) | 113 | 46 | 59 | 31 | 62 | 7 |
| Refraction (spherical equivalent) (DS) | −6.13±5.48 | −6.36±5.16 | −5.78±4.66 | −5.74±5.84 | −6.45±5.59 | −10.00±6.52 |
| Visual acuity (VA) | 0.73±0.26 | 0.81±0.22 | 0.86±0.25 | 0.72±0.24 | 0.74±0.24 | 0.45±0.10 |
| Keratometer readings (D) | 54.68±7.09 | 53.51±6.39 | 53.93±6.54 | 54.19±7.62 | 54.58±6.98 | 56.45±7.23 |
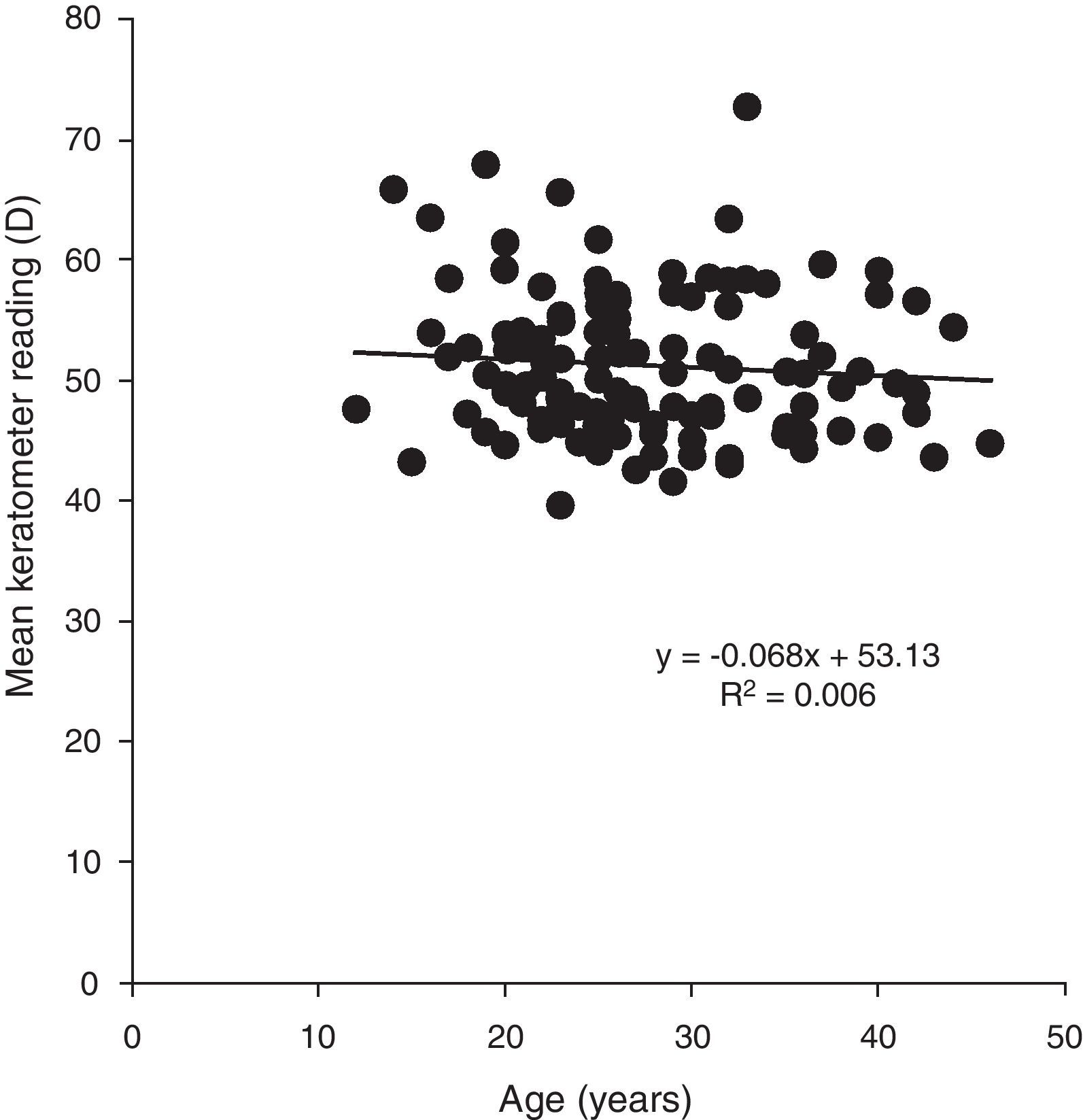
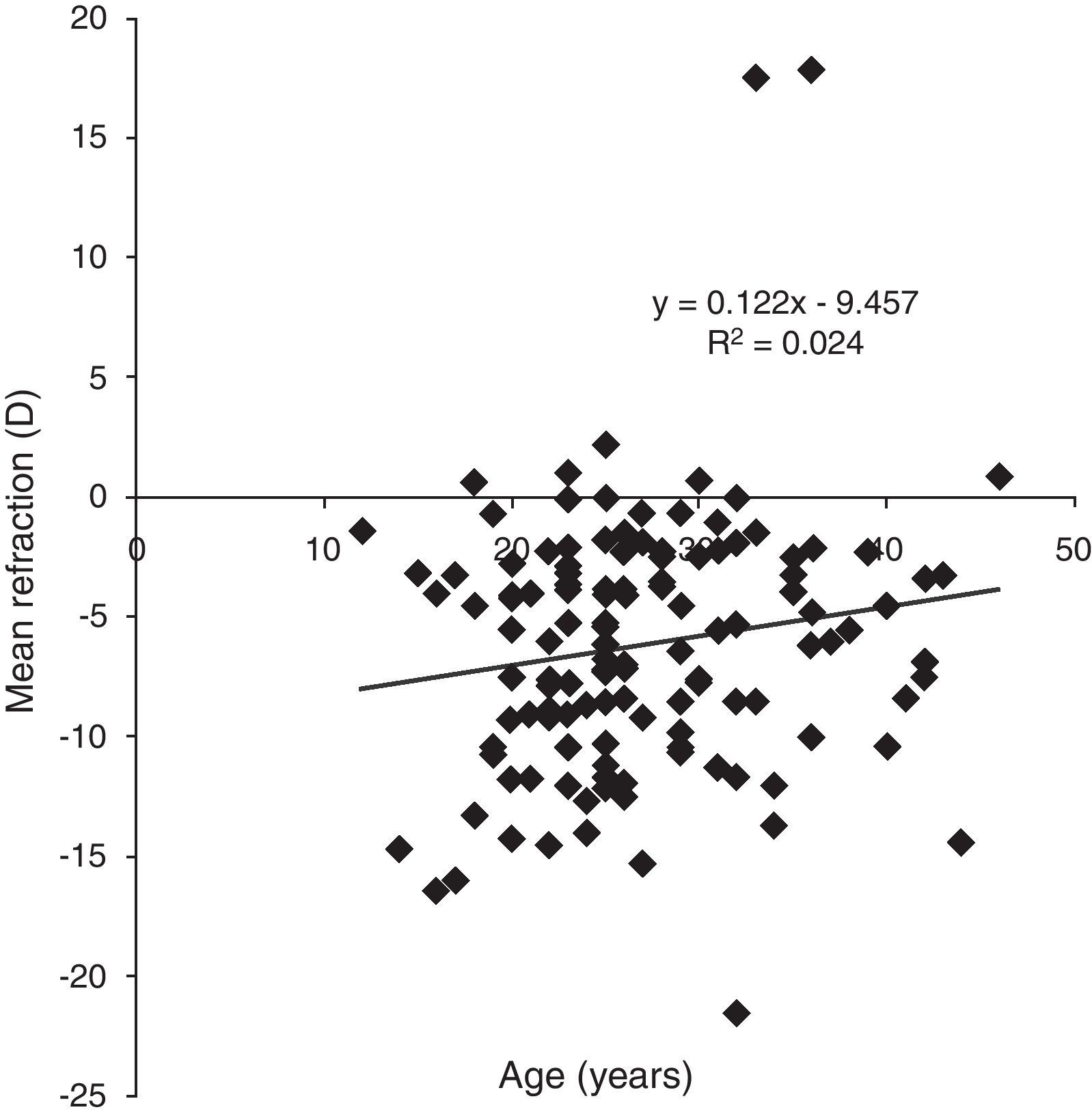
Majority of the patients observed were of Indian (39%) and Malay (37%) origin. No significant difference was detected between races and gender in all the parameters measured (p>0.05). Pearson correlation analyses were performed between age of onset and mean K reading as well as between age of onset and mean refraction. The results showed negative but no statistically significant correlation between mean K versus age of onset (p=0.696, r=−0.081) and positive but no statistically significant correlation between mean refraction versus age of onset (p=0.292, r=0.155). Similar analyses were performed in every age group and the results also indicate poor and no statistically significant correlations for both parameters in every age group. Figures 1 and 2 depict the correlation between age of onset and mean K and refraction.
With regards to general health, around 29% of patients had asthma and 6% had problems of allergy. However, only 5% of them reported constant eye rubbing. Slit lamp findings showed that 11% had signs of ocular allergy such as red eye and papillae, 6.3% had Vogt's striae, 4% had corneal scar and 2% had Munson's sign. Following the Amsler–Krumeich grading system,14 37.6% were categorized as stage I, 30.1% stage II, 4.4% stage III and 27.8% stage IV keratoconus at the time of diagnosis.
Majority (52%) of the keratoconus patients were prescribed with contact lens. Around 24% had crosslinking treatment and another 2.5% had corneal graft. A small percentage (2.5%) of patients was prescribed with glasses as they were diagnosed at early stage of the disease and were not keen to start on contact lenses. Another 5% of the patients were in the waiting list for crosslinking treatment at the time of data collection.
DiscussionThe prevalence and incidence of keratoconus have been variably reported with most estimates being 50–230 per 100,000 in general population (approximately 1 per 2000 to 1 per 500).3 The prevalence found in this study is higher, of approximately 1 per 100. This estimated prevalence may not be the indicator for the frequency of keratoconus in Malaysia as some of the patients in this study were referred to the specialist clinic for follow-up examination. However, this is the first reported prevalence of keratoconus in Malaysia and the prevalence obtained is part of a demographic profile of keratoconus patients attending a corneal specialist clinic in this country.
The results of the present study also demonstrate apparent difference in the percentage of cases observed among different ethnic groups in this country. Malaysia is a multiracial country consisting of three main ethnic groups. Data from Malaysia census population and housing report 2010 showed that around 49.74% of the population were Malays, 22.80% Chinese and 1.30% Indians.15 Majority of the keratoconus patients were of Indian and Malay origins. Similar trend was also observed in a tertiary eye care centre in this country.16 Despite the claim by Rabinowitz,2 who states that all ethnic groups are equally affected, the variation in the percentage suggests that genetic factor may influence the development of the disease. Earlier reports indicate a 4–7.6-fold increase in keratoconus incidence among Asian population compared to Caucasians. Georgiou et al.6 whose study population mostly comprised people from the Indian continent found lower incidence of atopy among Asians compared to Caucasians. Furthermore, there were reports stating that the Asian keratoconus patients were generally younger when the condition first presented and required corneal grafting at earlier age.5 According to Pierson et al.,5 majority of Asian keratoconus patients reaches the advanced stage by the second decade of their life. However, larger multicentre studies are needed to further confirm these findings.
The results of the present study support the earlier reports and emphasize the need for early screening, detection and treatment in the younger population within this region. Early detection and appropriate management may improve the quality of life of keratoconus patients. Nevertheless, older patients were expected to have more severe disease due to progression of the disease. However, the analysis of this study showed no statistically significant correlation between age and mean K and between age and manifest refraction. These results however suggest that age is not a factor in determining the level of severity of the disease.
Awareness of gender-based differences is important in prevention, diagnosis and management of conditions that may be more prevalent to one gender. In this study, higher percentage of men (71%) than women (29%) was found to have keratoconus. However, no significant difference was detected between genders with respect to the mean K and refraction. In a study performed in United Kingdom, around 60% of the 130 keratoconus patients attending a corneal specialist clinic were men.13 In New Zealand, men were found to have an earlier onset of keratoconus and experience a more rapid disease course.12 However, results of the present study showed no significant difference in the mean age at the time of presentation between men and women. Fink et al.11 reported that there was no difference in the disease severity as measured by first definite apical clearance lens, keratometry or scarring, although women were more unlikely to have Vogt's striae. Such difference was not noted in this study due to small number of patients having Vogt's striae at the time of presentation. Clinical signs such as corneal scar and Vogt's striae were not common in this study even though majority of the patients were at moderate and advanced stage of the disease.
It was also noted that high percentage of the keratoconus patients in this study had asthma. The association between keratoconus and atopic disease has been reported in earlier studies.17,18 Rahi et al.18 showed significantly higher levels of serum IgE in keratoconus compared to control groups which suggest that atopic traits are more common in patients with keratoconus than general ophthalmic patients.
This study highlights the demographic profile of keratoconus patients from a single cornea specialist centre in Kuala Lumpur. There is an apparent difference in the prevalence of keratoconus between ethnic groups that suggest the possibility of genetic factor playing a role in the aetiology of the disease. The condition was found to manifest at younger age (early 20s) and more common in men than women. These factors should be considered during vision screening so that early intervention can be provided.
Conflict of interestsThe authors have no conflict of interests to declare.
We acknowledged the staff of Pusat Pakar Mata Centre for Sight Petaling Jaya for their kind support throughout this study.