Manometric studies have found that intraocular pressure (IOP) rises 116–350mmHg during scleral depression in surgical settings. No information is available regarding the effect of scleral depression on IOP in routine clinical settings. The aim of this study is to quantify the change in IOP that occurs when scleral depression is performed on normal eyes in a routine clinical setting.
MethodsA total of 28 eyes from 28 normal subjects were included. Tono-Pen tonometry was performed while scleral depression was performed in each of the two quadrants: superotemporal (ST) and inferonasal (IN). A post-procedure IOP measurement was obtained following each scleral depression examination. Both ST and IN quadrants were tested on all eyes, with the quadrant tested first chosen at random (15 ST, 13 IN).
ResultsThe mean IOP during scleral depression was 65.3mmHg ST and 47.8mmHg IN, with a maximum recorded IOP of 88mmHg. The mean change in IOP for the ST quadrant was 51.9±17.3mmHg and 46.4±16.0mmHg for the right and left eyes, respectively. The mean change in IOP for the IN quadrant was 45.3±22.7mmHg and 16.8±15.8mmHg for the right and left eyes, respectively.
ConclusionsScleral depression as performed in a routine office setting produces wide fluctuations in IOP and may impair ocular perfusion. Additional studies are needed to determine the long-term consequences of routine scleral depression.
Los estudios manométricos han hallado que la presión intraocular (PIO) se eleva de 116 a 350mmHg durante la depresión escleral en el ámbito quirúrgico. No se dispone de información en relación al efecto de la depresión escleral sobre la PIO en la rutina del ámbito clínico. El objetivo de estudio es la cuantificación del cambio en la PIO que se produce cuando se realiza la depresión escleral en ojos normales en un escenario clínico rutinario.
MétodosSe incluyeron un total de 28 ojos de 28 sujetos normales. Se realizó una tonometría Tono-Pen, mientras que la depresión escleral se llevaba a cabo en dos cuadrantes: superotemporal (ST) e inferonasal (IN). Se realizó una medición de la PIO tras llevar a cabo cada depresión escleral. Se realizaron las medidas en ambos cuadrantes ST e IN en todos los ojos, eligiéndose el primer cuadrante a testear al azar (15 ST, 13 IN).
ResultadosLa PIO media durante la depresión escleral fue de 65,3mmHg ST y 47,8mmHg IN, con una PIO máxima registrada de 88mmHg. El cambio mínimo de la PIO para el cuadrante ST fue de 51,9±17,3mmHg y de 46,4±16,0mmHg para los ojos derechos e izquierdos, respectivamente. El cambio medio de la PIO para el cuadrante IN fue de 45,3±22,7mmHg y 16,8±15,8mmHg para los ojos derechos e izquierdos, respectivamente.
ConclusionesLa depresión escleral, realizada en un entorno clínico rutinario, produce fluctuaciones de la PIO y puede afectar a la perfusión ocular. Son necesarios estudios adicionales que determinen las consecuencias a largo plazo de la depresión escleral rutinaria.
Scleral depression, sometimes referred to as “scleral indentation”, is a routine clinical procedure performed during binocular indirect ophthalmoscopy (BIO) to enhance visualization of the peripheral fundus.1 The procedure is used to extend visualization of the fundus further into the periphery and to accentuate the clinical appearance of certain lesions, such as retinal holes and tears, and hence increase the likelihood of their detection.
Scleral depression is performed by indenting the wall of the eye with an instrument known as a scleral depressor while the region of the fundus being indented is viewed ophthalmoscopically. Indentation of the globe during scleral depression produces an increase in intraocular pressure (IOP) because the contents of the globe are compressed into a smaller volume. Studies using manometry on enucleated eyes2 and during scleral buckling surgery3 have recorded IOP readings of 116mmHg to 350mmHg during scleral depression.
Published data do not currently exist on the amount of IOP elevation that occurs in normal eyes during scleral depression under conditions of routine ophthalmoscopic examination. Published studies that have investigated this question were conducted on diseased rather than normal eyes, and IOP measurement was performed using an invasive procedure (manometry) rather than tonometry. The purpose of this study is to quantify the elevation in intraocular pressure during scleral depression in normal adult human eyes using tonometry under conditions resembling a routine office setting.
MethodsThis study was conducted in accordance with the principles of the Declaration of Helsinki and good clinical practice. All protocols were approved by the institutional review board at the University of the Incarnate Word. Subjects provided informed consent after being appropriately informed of the nature of the study.
Inclusion criteria for participation in this study were persons of 18–70 years of age with self-report of an eye exam within the last 4 years, no history of current or prior eye disease, and VA correctable to at least 20/30 in each eye. Exclusion criteria were any active ocular disease, intraocular surgery within the past 30 days in the tested eye, current or past history of glaucoma, anterior chamber angles of grade 2 or less using the Van Herick estimation technique, baseline IOP of 25mmHg or higher, any condition that could be exacerbated by acute elevations of IOP (such as myopic macular degeneration or angioid streaks), any media opacity that impairs visibility of the ocular fundus, or any ocular condition or abnormality that would impair accurate measurement of intraocular pressure. If both eyes of a subject were eligible for inclusion in the study, the study eye was selected at random.
Subjects underwent a screening examination, including best-corrected visual acuity, tonometry and biomicroscopy. The test eye was anesthetized with proparacaine and the pupil was dilated using 1% tropicamide and 2.5% phenylephrine. After the pupil had dilated to a minimum of 8mm in diameter, the subject was placed into a supine position and a screening ophthalmoscopic examination was performed without scleral depression.
All IOP measurements were made using the same Tono-Pen® XL tonometer (Reichert Inc., Depew, NY) that was calibrated prior to each session. Examiner #1 performed a baseline tonometry reading after the patient remained in the supine position for 5min. The average of 4 good quality tonometry readings was recorded as the IOP measurement, according to manufacturer's recommendations (Tono-Pen User's Guide, Reichert, 2012). Examiner #1 then performed tonometry while Examiner #2 performed BIO with scleral depression in each of the two quadrants: superotemporal (ST) and inferonasal (IN). Whether the ST or IN quadrant was tested first was determined at random.
Because maintaining the view of the fundus through the condensing lens of the ophthalmoscope is not possible while tonometry is being performed, the following procedure was adopted. The broad end of a double-tipped Josephberg-Besser scleral depressor was introduced and visualized in the peripheral fundus. Care was taken to not exert any more force than was necessary to achieve a satisfactory indentation of the fundus for routine examination purposes. As soon as this had been accomplished, the condensing lens was removed and Examiner #1 performed tonometry with Examiner #2 maintaining the position and amount of force exerted on the scleral depressor. Our method of measuring IOP while performing scleral depression is illustrated in Fig. 1. Following tonometry, Examiner #2 reintroduced the condensing lens and verified that the scleral depressor was still visible in the same location as before tonometry. The scleral depressor was then withdrawn.
Method of recording IOP while performing scleral depression. Once Examiner #2 has obtained a satisfactory view of the scleral depressor through the binocular indirect condensing lens, the condensing lens is removed and Examiner #1 performs tonometry. After an IOP reading has been obtained the condensing lens is reintroduced so that Examiner #2 may confirm that the scleral depressor has remained in the original position.
The duration of each scleral depression procedure was recorded with a stopwatch. Examiner #2 rated the degree of eyelid tension present as “loose”, “normal” or “tight” based upon his subjective impression of the amount of force required to achieve a satisfactory indentation of the fundus. A post-procedure IOP measurement was obtained following each scleral depression examination. Both ST and IN quadrants were tested on all eyes, with the quadrant tested first chosen at random (15 ST, 13 IN).
Power analysis was conducted prior to initiation of the study. The primary research hypothesis was that IOP will increase significantly from baseline during scleral depression. For a one-tailed, dependent-samples t-test, with alpha=.05, power=.80 and standardized effect size d=.5, a minimum sample size of 27 eyes was needed.
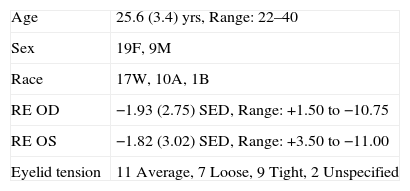
ResultsA total of 28 eyes (15 right and 13 left) from 28 normal healthy adult subjects were included in the study. Subject age ranged from 22 years to 40 years of age (mean: 25.6±3.4 years). There were 19 female and 9 male subjects. Self-reported race was predominantly white. Subject demographics are summarized in Table 1.
Demographic characteristics of subjects.
| Age | 25.6 (3.4) yrs, Range: 22–40 |
| Sex | 19F, 9M |
| Race | 17W, 10A, 1B |
| RE OD | −1.93 (2.75) SED, Range: +1.50 to −10.75 |
| RE OS | −1.82 (3.02) SED, Range: +3.50 to −11.00 |
| Eyelid tension | 11 Average, 7 Loose, 9 Tight, 2 Unspecified |
Data presented as mean (standard deviation). Yrs: Years; F: Female; M: Male; W: White; A: Asian; B: Black; OD: Right eye; OS: Left eye; RE: refractive error; SED: Spherical equivalent diopters.
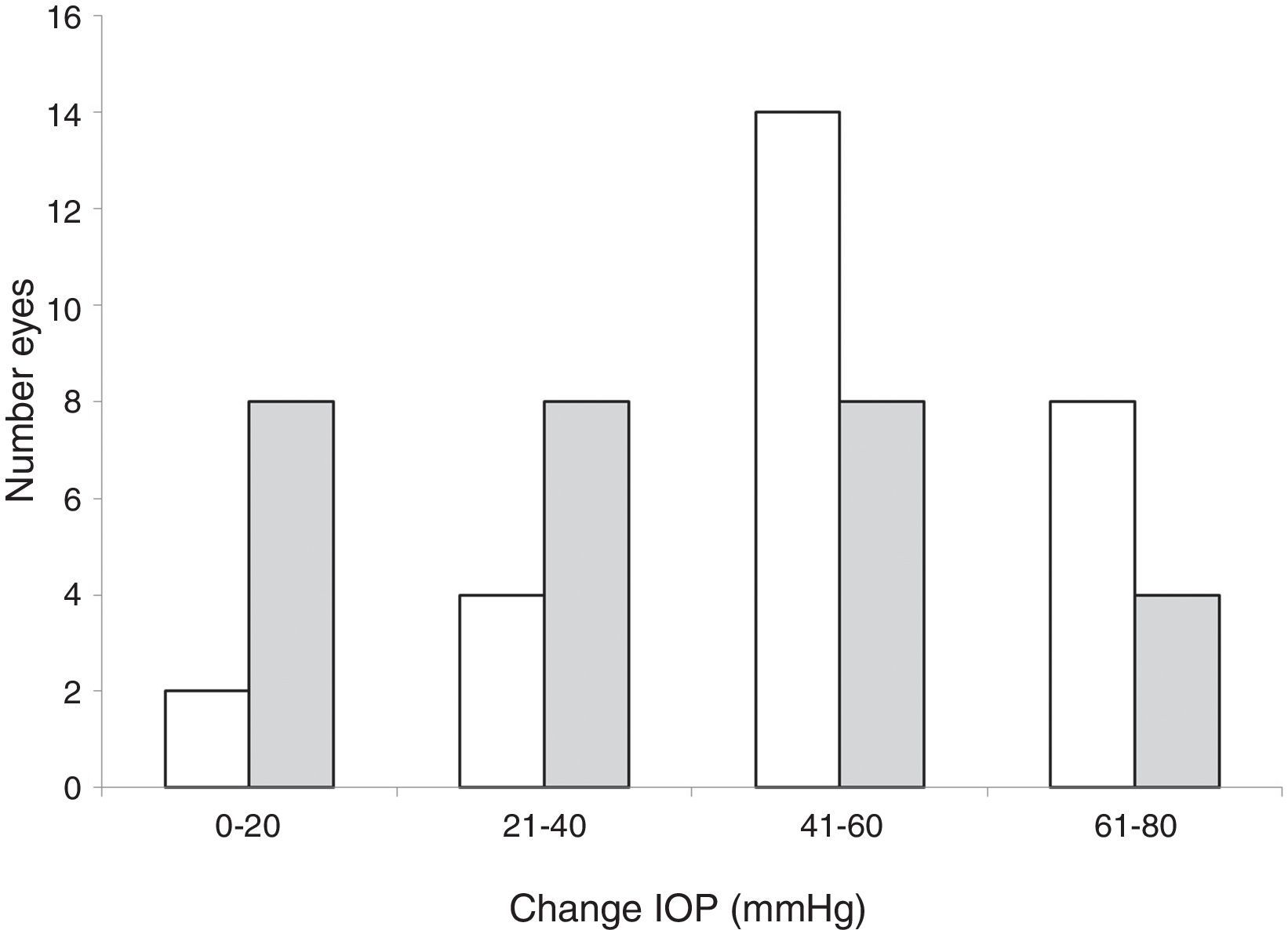
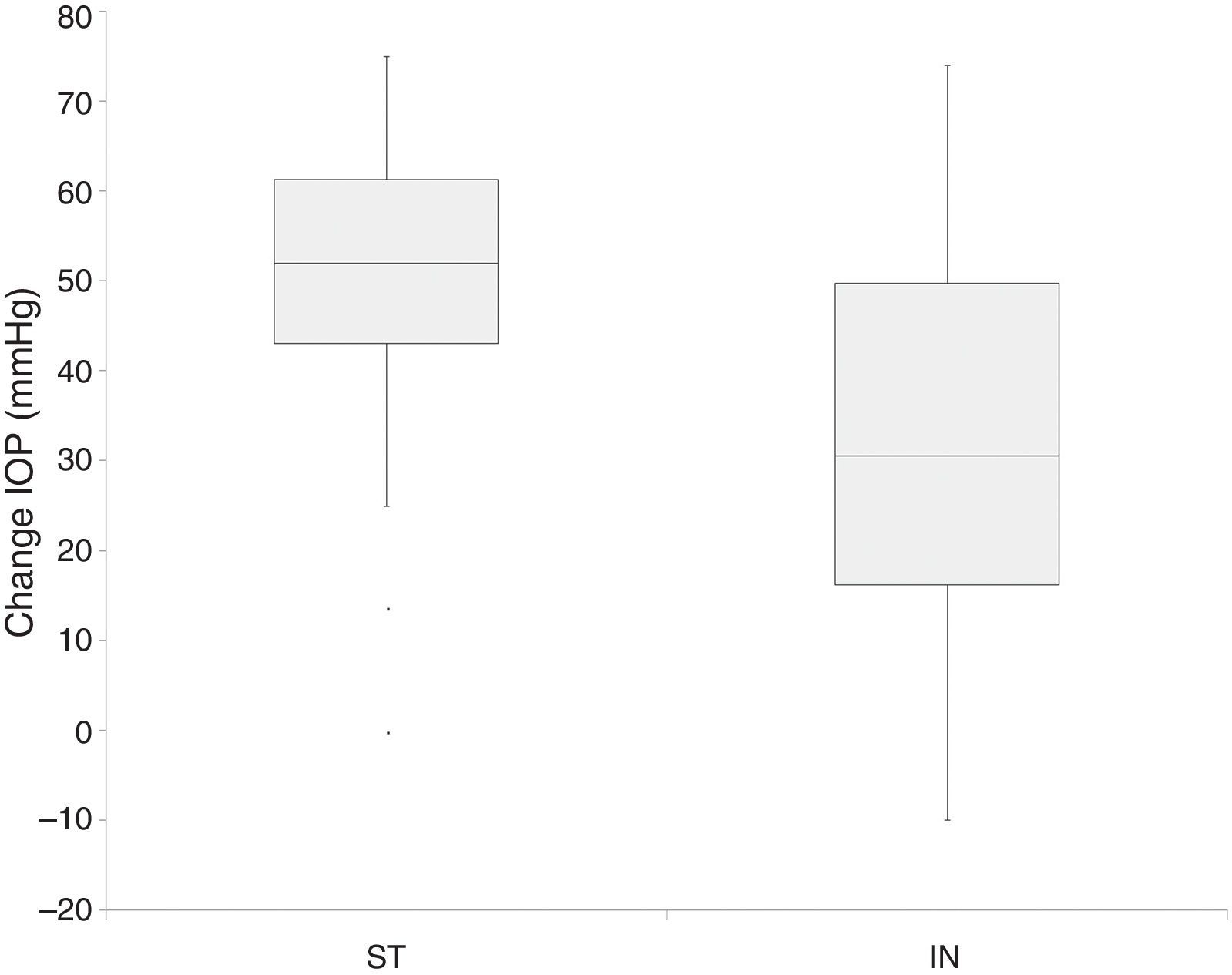
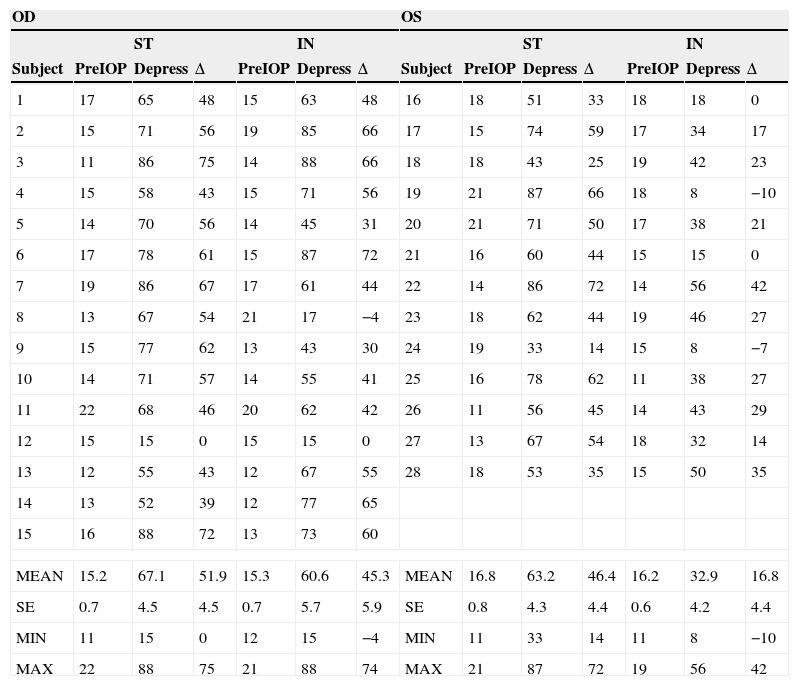
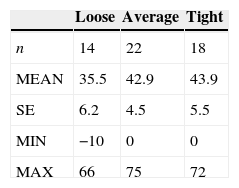
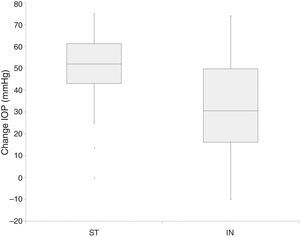
The IOP changes that occurred during scleral depression are presented in Table 2 and are presented graphically in Figs. 2 and 3. When scleral depression was performed in the ST quadrant, the mean rise in IOP was 49.4±17.0mmHg, and 8 subjects experienced a rise in IOP of greater than 60mmHg. When scleral depression was performed in the IN quadrant, the mean rise in IOP was 32.0±24.4mmHg, and 4 subjects experienced a rise in IOP of greater than 60mmHg. The change in IOP that occurred while performing scleral depression in the ST quadrant was, on average, significantly greater than when performing scleral depression in the IN quadrant (p<0.001).
Effect of scleral depression on IOP.
| OD | OS | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ST | IN | ST | IN | ||||||||||
| Subject | PreIOP | Depress | Δ | PreIOP | Depress | Δ | Subject | PreIOP | Depress | Δ | PreIOP | Depress | Δ |
| 1 | 17 | 65 | 48 | 15 | 63 | 48 | 16 | 18 | 51 | 33 | 18 | 18 | 0 |
| 2 | 15 | 71 | 56 | 19 | 85 | 66 | 17 | 15 | 74 | 59 | 17 | 34 | 17 |
| 3 | 11 | 86 | 75 | 14 | 88 | 66 | 18 | 18 | 43 | 25 | 19 | 42 | 23 |
| 4 | 15 | 58 | 43 | 15 | 71 | 56 | 19 | 21 | 87 | 66 | 18 | 8 | −10 |
| 5 | 14 | 70 | 56 | 14 | 45 | 31 | 20 | 21 | 71 | 50 | 17 | 38 | 21 |
| 6 | 17 | 78 | 61 | 15 | 87 | 72 | 21 | 16 | 60 | 44 | 15 | 15 | 0 |
| 7 | 19 | 86 | 67 | 17 | 61 | 44 | 22 | 14 | 86 | 72 | 14 | 56 | 42 |
| 8 | 13 | 67 | 54 | 21 | 17 | −4 | 23 | 18 | 62 | 44 | 19 | 46 | 27 |
| 9 | 15 | 77 | 62 | 13 | 43 | 30 | 24 | 19 | 33 | 14 | 15 | 8 | −7 |
| 10 | 14 | 71 | 57 | 14 | 55 | 41 | 25 | 16 | 78 | 62 | 11 | 38 | 27 |
| 11 | 22 | 68 | 46 | 20 | 62 | 42 | 26 | 11 | 56 | 45 | 14 | 43 | 29 |
| 12 | 15 | 15 | 0 | 15 | 15 | 0 | 27 | 13 | 67 | 54 | 18 | 32 | 14 |
| 13 | 12 | 55 | 43 | 12 | 67 | 55 | 28 | 18 | 53 | 35 | 15 | 50 | 35 |
| 14 | 13 | 52 | 39 | 12 | 77 | 65 | |||||||
| 15 | 16 | 88 | 72 | 13 | 73 | 60 | |||||||
| MEAN | 15.2 | 67.1 | 51.9 | 15.3 | 60.6 | 45.3 | MEAN | 16.8 | 63.2 | 46.4 | 16.2 | 32.9 | 16.8 |
| SE | 0.7 | 4.5 | 4.5 | 0.7 | 5.7 | 5.9 | SE | 0.8 | 4.3 | 4.4 | 0.6 | 4.2 | 4.4 |
| MIN | 11 | 15 | 0 | 12 | 15 | −4 | MIN | 11 | 33 | 14 | 11 | 8 | −10 |
| MAX | 22 | 88 | 75 | 21 | 88 | 74 | MAX | 21 | 87 | 72 | 19 | 56 | 42 |
Data presented as IOP in mmHg. OD: Right eye; OS: Left eye; ST: Scleral depression in the superotemporal quadrant; IN: Scleral depression in the inferonasal quadrant; PreIOP: IOP recorded immediately prior to scleral depression; Depress: IOP recorded during scleral depression; Δ: Change in IOP induced by scleral depression; SE: Standard error; MIN: Minimum; MAX: Maximum.
Histogram of change in IOP recorded during scleral depression. White bars represent readings obtained during scleral depression of the superotemporal (ST) quadrant, and shaded bars represent readings obtained during scleral depression of the inferonasal (IN) quadrant. Negative recorded changes (reductions in IOP) are counted as zero increase in IOP in this graph.
Box plots of change in IOP recorded during scleral depression in the superiotemporal (ST) and inferonasal (IN) quadrants. The bottom and top of the box represent the first and third quartiles, and the band inside the box is the second quartile (the median). The vertical lines protruding from the box extend to the minimum and the maximum values of the data set, as long as these values do not differ from the median by more than one and half times the interquartile range (ST=18.75mmHg; IN=38.5mmHg). Values exceeding this limit are recorded as individual data points.
There was no significant difference in the mean IOP change of the superior and inferior quadrants of the right eye (p=0.26), but the mean change that occurred during scleral depression inferiorly in the left eye was significantly less than occurring during scleral depression of the superior quadrant of this eye (p<0.001). Furthermore, when comparing corresponding quadrants of the right and left eyes, there was no significant difference between superior quadrants (OD: 51.9±17.3; OS: 46.4±16.0; p=0.41), but inferior quadrants were significantly different (OD:45.3±22.7; OS: 16.8±15.8; p=0.001).
There was much greater variability in the IOP change that was recorded while performing scleral depression in an IN quadrant than a ST quadrant. The standard deviation was 40% larger and the interquartile range was more than twice as large (interquartile range ST: 18.75; IN: 38.50). It is noteworthy that 3 instances of IOP reduction occurred when scleral depression was performed in an IN quadrant (−4, −7, and −10mmHg) and none when scleral depression was performed in a ST quadrant. Similarly, there were 3 instances of no IOP change when scleral depression was done in an IN quadrant and only one instance of no IOP change when scleral depression was performed in a ST quadrant. Four of the 7 anomalous readings occurred in the IN quadrant of the OS. Exclusion of these anomalous readings, that are likely a consequence of measurement error, from the analysis does not change the results in a meaningful way. The change in IOP during scleral depression in the ST quadrant increases from 49.4±17.0mmHg to 51.2±14.3mmHg, and for the IN quadrant the IOP change increases from 32.0±24.4mmHg to 41.8±17.7mmHg. The general pattern of greater IOP change occurring during scleral depression in the ST quadrant persists after exclusion of the 7 anomalous readings from the results.
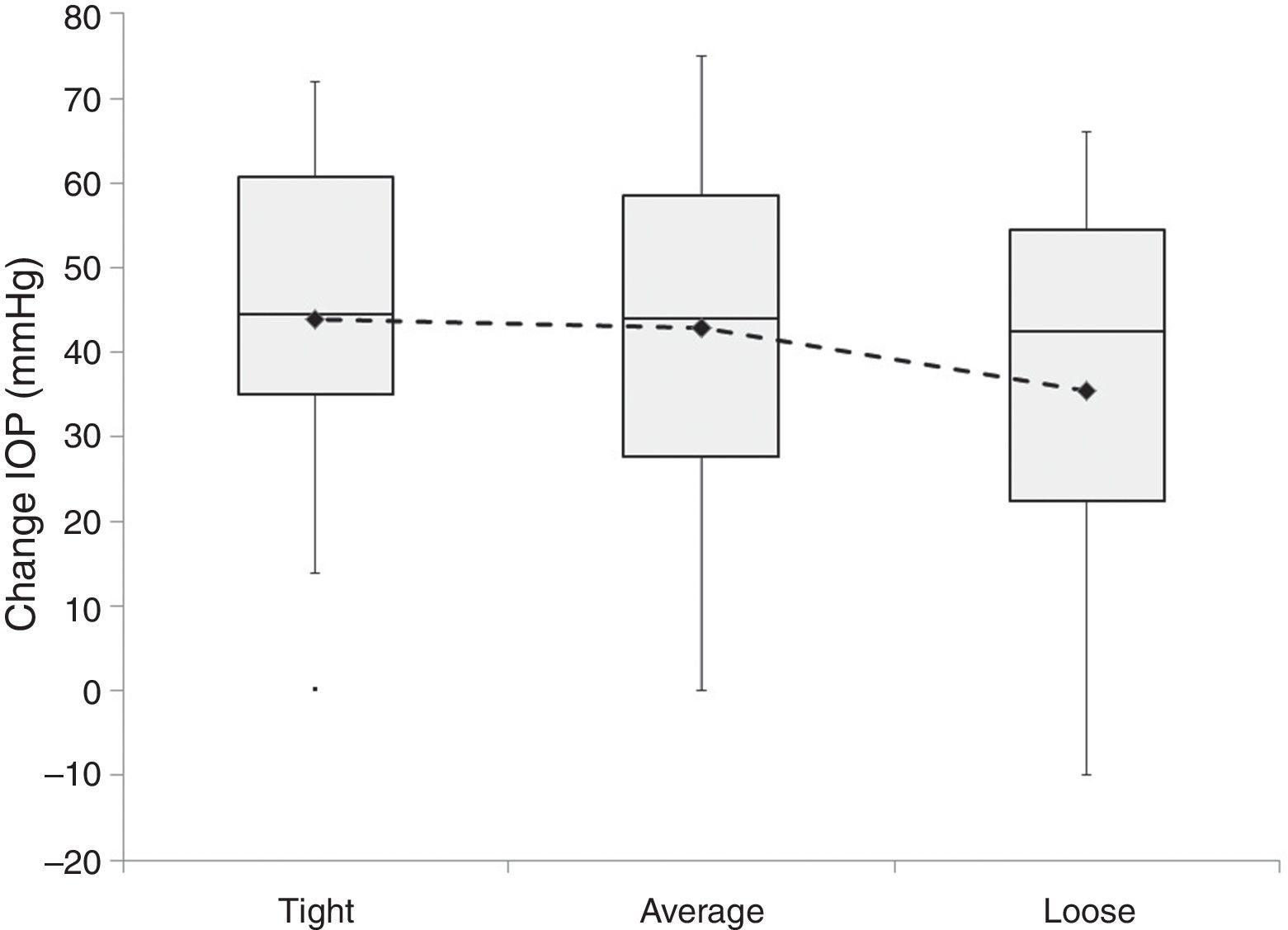
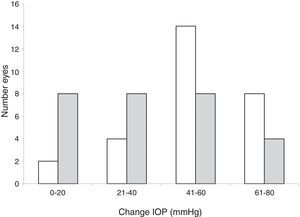
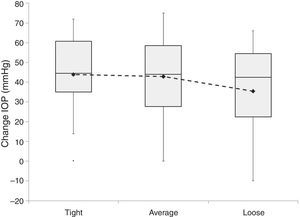
Lid tension during scleral depression was subjectively rated to be average in a total of 11 subjects, tight in 9 subjects, and loose in 7 subjects (Table 3, Fig. 4). There was a non-significant trend toward subjects judged to have loose eyelids to have a lower mean rise in IOP during scleral depression than subjects deemed to have average eyelid tension (p=0.35). Similarly, there was a non-significant trend toward those subjects with tight eyelids to have a greater mean rise in IOP than subjects with average eyelid tension (p=0.88).
Box plots of change in IOP recorded during scleral depression by lid tension. The bottom and top of the box represent the first and third quartiles, and the band inside the box is the second quartile (the median). The vertical lines protruding from the box extend to the minimum and the maximum values of the data set, as long as these values do not differ from the median by more than one and half times the interquartile range. Values exceeding this limit are recorded as individual data points. The means of each category are plotted with a diamond marker and are joined by the dashed line.
The mean change in IOP from baseline following scleral depression in a ST quadrant was −0.1±3.1mmHg and −0.6±3.6mmHg following scleral depression in an IN quadrant (p=0.64). The mean duration of scleral depression was 12.9±6.4s and 16.4±6.1s in the ST and IN quadrants, respectively (p=0.068).
DiscussionThis study finds that scleral depression causes a clinically significant elevation in IOP. The mean change during scleral depression was 40.7mmHg, and there were 12 recorded instances of a change >60mmHg.
The mean change in IOP was significantly greater when scleral depression was performed in the ST quadrant than in the IN quadrant. There are several possible explanations for this finding. One is that the resistance to indentation posed by the eyelids and sclera may differ in various quadrants. Greater eyelid and scleral resistance would be expected to produce a smaller indentation of the globe and hence smaller change in IOP for a given indenting force. Using the Shiotz tonometer, Patel et al.4 found that significant regional variations in resistance to indentation do exist between anterior scleral quadrants, with the greatest resistance in the IN quadrant and lowest resistance in the ST quadrant. These results are consistent with our findings of greater IOP change during indentation of the ST quadrant and less IOP change during indentation of the IN quadrant. While we are not aware of any studies investigating indentation resistance of the upper and lower lids, the significant anatomic differences between them would suggest that differences may exist. A second possible explanation is that the examiner consistently applied greater force while performing scleral indentation in the ST than the IN quadrant. While a deliberate effort was made to achieve equal indentation, as assessed ophthalmoscopically, in each location, we cannot rule out that a systematic error may have been introduced due to differences in grip strength, hand dominance, and other related factors. Yet another factor that may account for the observed difference in IOP change between ST and IN quadrants is that the tonometry measurements we obtained during scleral depression in the ST quadrant are perhaps more reliable that measurements obtained during scleral depression of the IN quadrant. Anomalous measurements, including no change or reductions in IOP during scleral depression, disproportionately occurred during scleral depression of the IN quadrant. This may be related to difficulties in obtaining a tonometry reading at the ideal position perpendicular to the center of the cornea during downward gaze, in which the cornea is often partially concealed behind the lower eyelid (Tono-Pen User's Guide, Reichert, 2012). It is therefore possible that the actual change in IOP that occurs during scleral depression is closer to what we found for the ST quadrant (49mmHg) than what was found for the IN quadrant (32mmHg).
The change in IOP during scleral depression recorded in our study is less than what has been previously reported during enucleation and scleral buckling surgery. Fraunfelder and co-workers2 used manometry to monitor the change in IOP that occurs during various stages of an enucleation surgical procedure in four human eyes, including scleral depression for purposes of retinal examination. He found that the peak IOP during scleral depression ranged from 160mmHg to 350mmHg. He concluded that scleral depression should not be routinely performed on eyes with intraocular malignancy because these very high intraocular pressures may increase the risk of tumor seeding and metastasis.
Gardner and colleagues3 used manometry to monitor IOP during scleral buckling surgery performed on 20 human eyes for rhegmatogenous retinal detachment. They found that on average the greatest increase in IOP that occurred during surgery was caused by scleral depression/cryopexy. A mean increase in IOP of 102.65±60.75mmHg occurred during scleral depression/cryopexy. They concluded that the IOP fluctuations that occur during scleral buckling surgery were large enough to possibly impair ocular perfusion, and this may be particularly detrimental in eyes with preexisting glaucoma or arterial insufficiency.
The smaller mean rise in IOP during scleral depression found in this study compared to prior studies may be a consequence of differences in study population, scleral depression technique, and IOP measurement methodology. Prior studies examined the effect of scleral depression on diseased eyes, whereas the current study examined the effect of scleral depression on normal eyes of healthy young adults. Both prior studies examined the effect of scleral depression as it is performed in the operating theater on anesthetized patients, whereas the current study may more closely reflect scleral depression as it is routinely performed in an office setting. Prior studies utilized manometry to directly measure IOP, whereas the current study measured IOP indirectly using Tono-Pen tonometry. Boothe and colleagues5 have examined the correlation between manometrically set IOP and Tono-Pen tonometry in enucleated eyes. They found the Tono-Pen tonometer tends to underestimate IOP at pressures greater than 20mmHg and the larger the degree of underestimation grew the further the IOP was increased above 20mmHg. At 70mmHg, the highest IOP that was examined, the Tono-Pen tonometer underestimated IOP by an average of about 7mmHg. Other studies have found that the Tono-Pen tonometer underestimates Goldmann tonometry at higher intraocular pressures. 6–9 Because the mean IOP recorded during scleral depression in our study was 56.5±22.2mmHg and the maximum was 88mmHg, it is likely that the Tono-Pen tonometer underestimated the changes in IOP that occurred during scleral depression.
There are no reports of serious adverse effects following scleral depression performed on normal healthy eyes. Nonetheless, it would seem prudent to exercise caution when performing scleral depression to minimize the magnitude and duration of IOP elevation because even brief periods of IOP elevation may produce clinically significant adverse effects. Gardner and co-workers3 found that central retinal artery closure occurred in the majority of their patients during scleral depression and cryopexy. The mean central retinal artery closing pressure (CRACP) in that study was 79mmHg (range: 48–110mmHg). In our study, the mean IOP during scleral depression was 65.3±16.7mmHg and 47.8±23.6mmHg in the ST and IN quadrants, respectively. These pressures are approaching the CRACP levels reported by Gardner et al.3 Gardner and co-workers also found that those patients whose CRACP exceeded during scleral depression were significantly older than patients who did not experience CRA closure during scleral depression. In addition, 69% of the patients who experienced IOP elevations during scleral depression in excess of their CRACP had a medical history of diabetes, hypertension, and/or atherosclerosis. While the patients in our study were, on average, younger than those in the study by Gardner et al., and all were in good medical health, our data reveal that scleral depression as performed in a routine office setting can achieve levels capable of inducing central retinal artery closure in some patients.
Caution is warranted when performing scleral depression in the immediate postoperative period following intraocular surgery1 because acute elevation in IOP has the potential to cause wound leak. A similar concern exists for patients with suspected penetrating injury because external pressure on the globe may worsen or aggravate the injury.1
A hemorrhagic retinopathy has been reported in infants with active retinopathy of prematurity (ROP) following examination with scleral depression.10,11 The retinopathy takes the form of numerous intraretinal dot and blot hemorrhages and a few flame hemorrhages scattered throughout the posterior fundus and vascularized periphery. The retinal hemorrhages may appear within hours of examination with scleral depression. It has been suggested that ocular manipulation, abrupt intraocular pressure change, and fragile immature retinal vasculature with poor autoregulation may contribute to the pathogenesis of this retinopathy. It is recommended that scleral depression be used judiciously in infants with active ROP.10
Serious adverse effects of transient IOP elevation have been reported. IOP spikes of 100mmHg or more can occur during LASIK surgery12 and may result in optic neuropathy and visual field defects.13 It has been suggested that cases of anterior ischemic optic neuropathy that develop immediately after an uncomplicated cataract extraction are a consequence of transient IOP elevation.14 Vision loss has also been reported as a consequence of IOP spikes that occur following argon laser trabeculoplasty.15
Electrophysiologic studies of experimentally induced acute IOP elevation in humans and animal models find that inner retinal dysfunction occurs soon after the onset of an IOP spike and may persist long after the IOP has returned to normal. Feghali and colleagues, using a rabbit model, found that pattern electroretinogram (PERG) amplitude was reduced within 1minute of suction cup-induced elevation of IOP to a level of 35–50mmHg.16 PERG amplitude immediately returned to baseline on discontinuation of suction. They suggest that the rapidity of onset and reversibility of this change suggest a vascularly mediated effect. Others have confirmed that in human subjects ocular perfusion pressure (OPP) rather than IOP per se plays the dominant role in reducing the PERG during acute elevation of IOP17,18 Kong et al., working in a mouse model, found that the positive wave of the scotopic threshold response (pSTR) electroretinogram was the most sensitive component of the flash ERG to acute IOP elevation.19 An IOP spike of 50mmHg lasting 30min resulted in a 50% reduction in pSTR amplitude that had not yet returned to baseline levels after 1 week. The investigators concluded that persistent impairment of inner retinal function can occur after a single IOP spike. Colotto and associates studied the effect of a 6minute elevation of IOP to 30mmHg (induced by scleral suction) on the PERG of normal controls and patients with ocular hypertension (OHT).20 They found that during IOP elevation PERG amplitudes of patients with OHT were significantly more reduced with respect to baseline values compared to those of controls. PERG amplitudes returned to baseline during the 6minute recovery period in each of the controls, but was much delayed in all of the OHT patients. The researchers concluded that the inner retina of patients with OHT may have a heightened sensitivity to the effects of acutely raised IOP. In summary, research on the electrophysiologic effects of experimentally induced IOP spikes suggest that transient IOP elevation of an order of magnitude and duration achievable during routine scleral depression may have adverse effects on inner retinal function, especially in patients with OHT and others that may have heightened sensitivity to transient decreases in OPP.
It is interesting to note that examiner evaluation of lid tension does show some correlation to the degree of IOP rise during scleral depression, although this effect failed to achieve statistical significance. This finding suggests that the examiner has the ability to assess how much effort is required to achieve a satisfactory scleral indentation and that this subjective perception by the examiner does correlate, albeit somewhat imprecisely, with the magnitude of the IOP elevation. It may be possible with feedback and training to further develop and refine this ability.
A strength of our study is that it offers a closer approximation of how scleral depression is routinely performed in an office setting than prior studies. Previous studies that have investigated IOP fluctuations during scleral depression specifically examined the effects of intraoperative manipulations on IOP. In the current study, we were more interested in simulating what may occur during a routine ophthalmoscopic examination. It is probable that the examination techniques used in these two settings are sufficiently different to have differing effects on IOP. Differences may also exist due to the possible influence of anesthesia in a surgical setting versus patient anxiety and discomfort during the procedure in an office setting. We believe that our findings more closely reflect the effects of scleral depression as it is performed during routine ophthalmoscopic examination in an office setting.
One weakness of the current study is that a single examiner performed all scleral depression procedures. Our findings may therefore reflect the style and technique used by this examiner, and hence may not be generalizable. Examiner variables such as hand dominance and grip strength could possibly influence the degree of IOP rise that occurs during scleral depression. Likewise, scleral depressors of various designs may have differing effects on IOP in the hands of a given examiner. For example, because the Josephberg-Besser scleral depressor indents more surface area than a depressor with a T-bar tip,21 it is possible that a depressor of this design would tend to produce a greater rise in IOP. Another weakness of this study are the limitations of the Tono-Pen tonometer, which impaired our ability to record IOP in down-gaze and which may underestimate true IOP in the range that is typically encountered during scleral depression.
In summary, we find that scleral depression performed on normal eyes of healthy young adults usually causes a 45–50mmHg elevation in IOP. A change of this magnitude may be clinically significant in patients who are sensitive to transient changes in ocular perfusion pressure, such as patients with glaucoma and arterial insufficiency. Additional studies are needed to determine the long-term consequences of these pressure elevations.
Financial disclosureNone.
Conflicts of interestThe authors have no conflicts of interest to declare.
This study was carried out with the approval from the University of the Incarnate Word Institutional Review Board, and informed consent was obtained from all subjects who participated in this study.