We analyze the role of bilateral symmetry in enhancing binocular visual ability in human eyes, and further explore how efficiently bilateral symmetry is preserved in different ocular surgical procedures. The inclusion criterion for this review was strict relevance to the clinical questions under research. Enantiomorphism has been reported in lower order aberrations, higher order aberrations and cone directionality. When contrast differs in the two eyes, binocular acuity is better than monocular acuity of the eye that receives higher contrast. Anisometropia has an uncommon occurrence in large populations. Anisometropia seen in infancy and childhood is transitory and of little consequence for the visual acuity. Binocular summation of contrast signals declines with age, independent of inter-ocular differences. The symmetric associations between the right and left eye could be explained by the symmetry in pupil offset and visual axis which is always nasal in both eyes. Binocular summation mitigates poor visual performance under low luminance conditions and strong inter-ocular disparity detrimentally affects binocular summation. Considerable symmetry of response exists in fellow eyes of patients undergoing myopic PRK and LASIK, however the method to determine whether or not symmetry is maintained consist of comparing individual terms in a variety of ad hoc ways both before and after the refractive surgery, ignoring the fact that retinal image quality for any individual is based on the sum of all terms. The analysis of bilateral symmetry should be related to the patients’ binocular vision status. The role of aberrations in monocular and binocular vision needs further investigation.
Analizamos el papel de la simetría bilateral para mejorar la capacidad visual binocular en ojos humanos, y exploramos adicionalmente el modo en que la simetría bilateral se conserva en diferentes procedimientos quirúrgicos oculares. Los criterios de inclusión para esta revisión fueron la relevancia estricta ante las cuestiones clínicas en estudio. El enantiomorfismo se ha reportado en aberraciones de bajo orden, aberraciones de alto orden, y direccionalidad de los conos. Cuando el contraste difiere en ambos ojos, la agudeza binocular es mejor que la agudeza monocular del ojo con mejor contraste. La anisometropía es una situación infrecuente en las grandes poblaciones. La anisometropía observada en la infancia y la juventud es transitoria, y de consecuencia menor para la agudeza visual. La sumación binocular de las señales de contraste declina con la edad, independientemente de las diferencias inter-oculares. Las asociaciones simétricas entre el ojo derecho y el izquierdo podrían explicarse mediante la simetría del offset pupilar y el eje visual, que es siempre nasal en ambos ojos. La sumación binocular mitiga el empeoramiento de la función visual en situaciones de baja luminosidad, y la fuerte disparidad inter-ocular afecta de manera perjudicial a la sumación binocular. Existe una simetría considerable de la respuesta en los ojos de los pacientes que se someten a PRK y LASIK para la corrección de la miopía, pero sin embargo el método para determinar si la simetría se mantiene o no consiste en comparar los términos aberrométricos individuales en una serie de modos ad hoc, con anterioridad y posterioridad a la cirugía refractiva, ignorando el hecho de que la calidad de la imagen de la retina para cualquier individuo se basa en la suma de todos los términos. El análisis de la simetría bilateral podría relacionarse con la situación de la visión binocular de los pacientes. El papel de las aberraciones en la visión monocular y binocular precisa una mayor investigación.
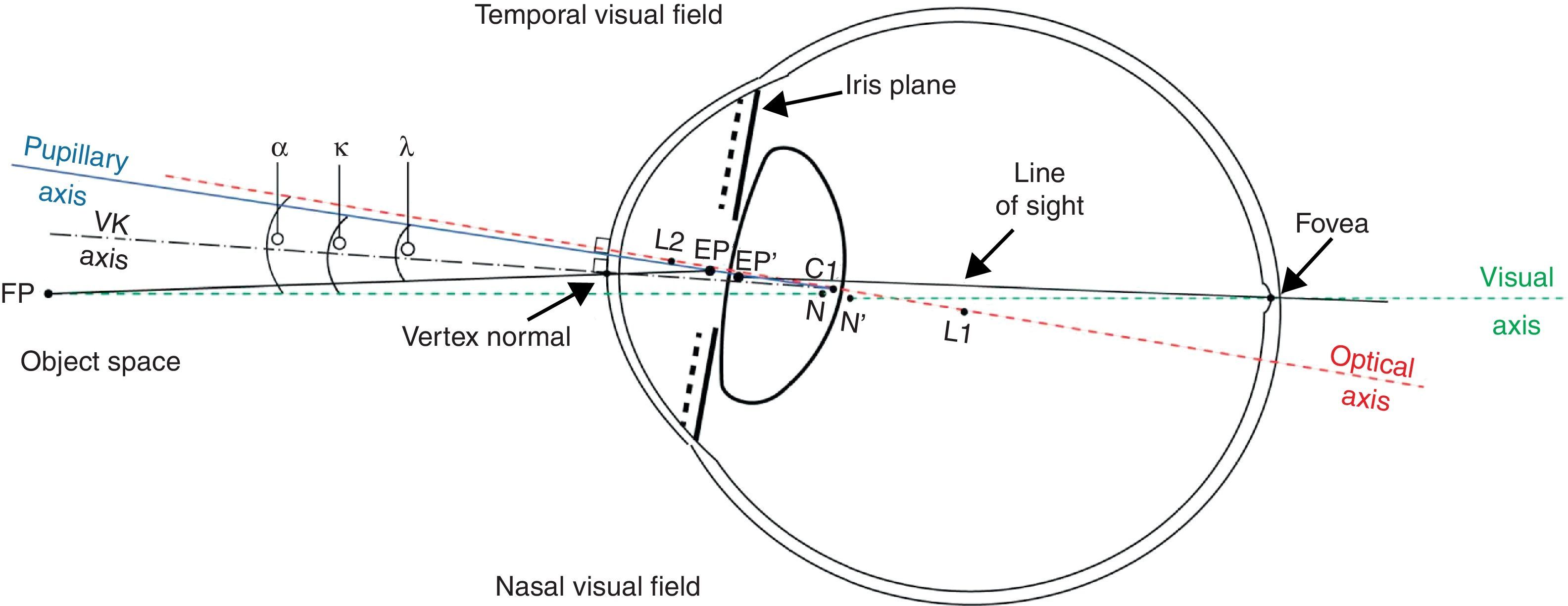
The role of bilateral symmetry and summation (or fusion) in forming the visual ability in humans has been pursued since centuries. The binocular visual system in humans possesses a cardinal feature to unify two separate monocular views to render a cyclopean view of the surroundings. In both eyes, the visual axis is symmetric to the nose–chin axis toward the nasal visual field, representing bilateral symmetry (enantiomorphism) (Fig. 1). The binocular visual system also makes stereopsis possible.1 The parallax provided by the different positions of the two eyes in the head, gives humans a precise sense of depth perception.2 Binocular viewing of a scene creates two slightly different images of the scene. These differences, referred to as binocular disparity, provide information that the brain can use to calculate depth in the visual scene, providing a major means of depth perception. It has been suggested that the impression of “real” separation in depth is linked to the precision with which depth is derived, and that a conscious awareness of this precision (perceived as an impression of realness) may help guide the planning of motor action.3 Stereopsis appears to be processed in the visual cortex of mammals in binocular cells having receptive fields in different horizontal positions in the two eyes. Such a cell is active only when its preferred stimulus is in the correct position in the left eye and in the correct position in the right eye, making it a disparity detector.
Schematic sketch of the reference angles and axes in the human eye. The axes are indicated by the following lines; solid black (line of sight), solid blue (pupillary axis), dashed green (visual axis), dashed red (optical axis), and dashed black (videokeratoscope axis). The centers of curvature of each refracting surface are represented as L2, C2, C1, and L1. In both the eyes, the visual axis is symmetric to the nose–chin axis toward the nasal visual field, representing the bilateral symmetry (enantiomorphism). Binocular fusion unifies two separate monocular views to render a cyclopean view of the surroundings. (Image courtesy of: Nowakowski, Sheehan, Neal, Goncharov: Investigation of the isoplanatic patch and wavefront aberration along the pupillary axis compared to the line of sight in the eye. Biomed Opt Express 2012, 3:240–258.)
Several visual tasks and experiments have explored and compared the monocular and binocular visual performance in humans. Blake and Fox4 presented a very important review of the experiments and techniques developed in the 20th century in pursuit of the question, whether binocular summation enhances the visual performance in humans They concluded that binocular vision enhances visual performance compared to monocular vision. Neural binocular summation occurs when the binocular response is greater than the probability summation.5
Other important features of binocular vision include utrocular discrimination (the ability to tell which of two eyes has been stimulated by light),6 eye dominance (the habit of using one eye when aiming something, even if both eyes are open),7 allelotropia (the averaging of the visual direction of objects viewed by each eye when both eyes are open),8 binocular fusion or singleness of vision (seeing one object with both eyes despite each eye having its own image of the object),4 and binocular rivalry (seeing one eye's image alternating randomly with the other when each eye views images that are so different they cannot be fused).9
In this topical review, our motive is twofold, first to analyze the role of bilateral symmetry in enhancing the binocular visual ability in human eyes, and second to explore how efficiently bilateral symmetry is preserved in different ocular surgical procedures performed in the current times.
Bilateral symmetry in human visual systemThe bilateral symmetry (enantiomorphism) in human eyes with respect to the nose–chin axis enables a much wider horizontal field of view than vertical field of view (Fig. 2). Humans have a maximum horizontal field of view of ∼190° with two eyes, ∼120° of which makes up the binocular field of view flanked by two uniocular fields of ∼40° each. Further to this, both eyes show many interrelated symmetries and can influence each other in several ways. Light falling in one eye affects the diameter of the pupils in both eyes. If one eye is open and the other closed, the closed eye follows the accommodation of the opened eye. The state of light adaptation of one eye can have a small effect on the state of light adaptation of the other. Li et al.10 evaluated the symmetry between the right and left eye of 397 subjects in 14 biometric parameters. They found a potentially clinically important inter-ocular symmetry in spherical equivalent, best corrected visual acuity (BCVA), average corneal curvature, Jackson crossed cylinder power of corneal astigmatism (CJ0 and CJ45), intraocular pressure, central corneal thickness, axial length (AL), anterior chamber depth, lens thickness and vitreous chamber depth; with significant interocular differences observed only in Jackson crossed cylinder power of refractive error astigmatism with axes at 90° and 180° (RJ0, p=0.00), and at 45° and 135° (RJ45, p=0.02) and corneal asphericity coefficient (p=0.00). However, for keratoconic patients a greater inter-ocular asymmetry in pachymetry and posterior corneal elevation variables has been reported.11,12 Based on inter-ocular symmetry, many diagnostic methods have been presented to discriminate between normal and keratoconic cornea.13–18 Galletti et al.19 evaluated inter-ocular corneal asymmetry in Pentacam (Oculus Optikgeräte GmbH, Wetzlar, Germany) indexes as a diagnostic method between normal patients and patients with keratoconus. They found that unlike keratoconic corneas, healthy corneas are markedly symmetric irrespective of anisometropia (a condition in which the two eyes have unequal refractive power), however corneal asymmetry analysis does not provide sufficient sensitivity to be used alone for detecting keratoconus.
The aberrations in the human visual system have been studied in reference to ocular symmetry in the past. Howland and Howland,20 employed the cross-cylinder aberroscope method they invented, and found that the optical aberrations of the eye differ greatly from subject to subject and are seldom symmetrical. McKendrick et al.21 investigated the relationship between the astigmatic axes of right and left eye pairs, with particular attention given to determining the degree to which either direct or mirror symmetry of the astigmatic axes exists. They found that in a study population of 192 individuals, there was no evidence for a predominance of either mirror or direct symmetry of the astigmatic axes. The patterns of astigmatic axis distribution of right and left eyes were remarkably similar but, within this context, there was no definite evidence for a definable association between the axis of the left and right pairs of individuals.
In recent studies, however, different findings have been reported. Touzeau et al.22 prospectively recorded both subjective refraction and auto-refractometry data of 500 patients. They quantified enantiomorphism between fellow eye axes by the absolute value of the difference between 180° and the sum of both axes. Axes were more enantiomorphic when the cylinder was high and the subject young. Oblique axes were less enantiomorphic (35.5° vs. 20.6°, p<0.001) and were associated with lower cylinder (0.56D vs. 0.98D, p<0.001). Correlation between fellow eyes was significant for cylinder (r(s)=0.66, p<0.001) and for spherical equivalent (r(s)=0.96, p<0.001).
Binocular vision and higher order optical aberrations of the eyeLiang and Williams23 constructed a wavefront sensor to measure the optical aberrations beyond the classical aberrations of the eye. They found that irregular aberrations (more popularly called as higher order aberrations (HOA)), do not have a large effect on retinal image quality in normal eyes when the pupil is small (3mm). However, they play a substantial role when the pupil is large. Although the pattern of aberrations varies from subject to subject, aberrations, including irregular ones, are correlated in left and right eyes of the same subject, indicating that they are not random defects. Porter et al.24 confirmed this observation in a large population. Thibos et al.25 used a Shack–Hartmann aberrometer to measure the monochromatic aberration structure along the primary line of sight of 200 cyclopleged, normal, healthy eyes from 100 individuals. Their results verified the correlation of aberrations from the left and right eyes indicating the presence of significant bilateral symmetry. Wang et al.26 investigated the distribution of anterior corneal HOA's (3rd to 6th orders) in a population of 134 subjects, and found that a moderate to high degree of mirror symmetry existed between right and left eyes.
Prakasht et al.27 evaluated the HOA's and resultant bilateral wavefront patterns in a cross sectional observational trial of seven consecutive pediatric patients (mean age of 9±3 years) with idiopathic amblyopia. They found no significant difference in the average of Zernike coefficients between normal and amblyopic eye. However, interrelation between Zernike coefficients was different between amblyopic and fellow eyes associated with a loss of symmetry in wavefront patterns of the two eyes. Maximum difference in the R-squared values between amblyopic and normal (fellow) eyes was seen with coma-like and trefoil-like aberrations (third order and fifth order terms). Fam et al.28 determined the effect of individual Zernike wavefront aberrations on binocular summation and binocular visual acuity and found that binocular vision has a positive effect in reducing the visual impact of aberrations as Zernike modes that suffer from the most loss of visual acuity also experience the greatest amounts of binocular summation.
In addition to the aberrations in the ocular optics, cone directionality (Stiles–Crawford effect) also controls the retinal image quality sampled by the photoreceptor array. Marcos et al.29 investigated in 12 subjects the symmetry between the right and left eyes for wavefront aberration (measured using a spatially resolved refractometer) and cone directionality (measured using an imaging reflectometric technique). Although they found that the pattern of aberrations is in general non-symmetric, suggesting that the development of aberrations follows independent paths in many right and left eye pairs, but cone directionality is in most cases mirror-symmetric (with one case of direct symmetry), suggesting some systematic process underlying cone orientation.
Binocular vision and contrast perceptionBinocular vision is traditionally treated as a combination of two processes: the fusion of similar images (binocular summation), and the inter-ocular suppression of dissimilar images (e.g. binocular rivalry). At low spatial frequencies, where the monocular sensitivity difference is minimal, binocular summation is obtained. As the sensitivity difference increases at higher spatial frequencies, the binocular contrast sensitivity decreases steadily demonstrating binocular inhibition.30 Recent work has demonstrated that inter-ocular suppression is phase-insensitive, whereas binocular summation occurs only when stimuli are in phase. In a key study by Ding and Sperling,31,32 observers indicated the perceived location of the dark bar of a sine-wave grating, which was presented as two monocular component gratings of different spatial phases. The full pattern of their results was explained by a binocular gain control model featuring suppression between the eyes, followed by binocular summation. Jiawei Zhou et al.33 presented a modification to the interocular gain-control theory32 that unifies first- and second-order binocular summation with a single principle called the contrast-weighted summation concluding that the second-order combination is controlled by first-order contrast. Daniel Baker et al.34 also challenged the model by Ding et al.32 in which contrast perception is shown to be phase-invariant. They measured perceived contrast using a matching paradigm for a wide range of inter-ocular phase offsets (0–180°) and matching contrasts (2–32%). Their results were predicted by a binocular contrast gain control model involving monocular gain controls with inter-ocular suppression from positive and negative phase channels, followed by summation across eyes and then across space. When applied to conditions with vertical disparity this model had only a single (zero) disparity channel and embodied both fusion and suppression processes within a single framework. Another interesting viewpoint was given by Thor Eysteinsson et al.35,36 who successfully demonstrated tonic inter-ocular suppression (TIS) by the means of visual evoked potential (VEP) procedures. Conversely, they concluded from these results that the increase in VEP amplitude resulting from binocular vision may be attributed to the removal of TIS rather than physiological binocular summation. Therefore, the perceived binocular visual direction of a fused disparity stimulus with an inter-ocular contrast difference is biased toward the direction signaled by the eye presented with the higher contrast image. Similar findings were reported by Weiler et al.37
When contrast differs in the two eyes, binocular acuity has been shown to be better than the monocular acuity of the eye that receives higher contrast.38,39 This binocular advantage becomes smaller but remains significant as contrast disparity became larger.39 Cuesta et al.40 evaluated the impact that interocular differences in corneal asphericity (Q) exert on binocular summation measured as the contrast-sensitivity function (CSF). A total of 92 emmetropic subjects took part in the experiment, classified according to the inter-ocular differences in corneal asphericity (ΔQ) measured with an EyeSys-2000 corneal topographer. Fifty-four subjects had ΔQ<0.1; 21 subjects had 0.1≤ΔQ≤0.2; and 17 had ΔQ>0.2. The CSF was measured monocularly (for each eye) and binocularly at different spatial frequencies. Although the binocular CSF for the three groups studied was greater than the monocular in all the spatial frequencies studied, there were significant differences in binocular summation. They concluded that differences in corneal asphericity may affect the binocular visual function by diminishing the binocular contrast-sensitivity function. This could significantly affect the results of a refractive procedure, where although the subject becomes emmetropic, if inter-ocular differences are induced in corneal asphericity; it could still reduce the binocular visual performance. Aniseikonia can also have similar implications on cataract and refractive procedures, with studies41,42 revealing a significant decline in binocular contrast sensitivity and binocular summation for 5% aniseikonia, this decline being more pronounced for intermediate and high spatial frequencies.
Development of binocular vision with ageAnisometropia is generally characterized by a threshold inter-ocular power difference of two diopters. This condition has been observed very rarely in studies with large study populations, however it may be indicative of a possible significant deterioration of post-refractive surgery mesopic binocular CSF.43 Almeder et al.44 conducted a longitudinal study for 10 years, to examine the focusing and motor behavior of a volunteer population of 686 subjects aged 3 months to 9 years. The aim of the study was to characterize normal refractive development in infants and children and to relate refractive anomalies to subsequent visual problems. They concluded that much of the anisometropia seen in infancy and childhood is transitory and probably of little consequence for the eventual visual acuity. With an error probability of 5% or less, they found a persistent anisometropia in 1% or less in their study population.
Studies45 also indicate that in children, binocular and dichoptic contrast sensitivity (binocular and dichoptic summation) is better than monocular. The magnitude of binocular/dichoptic summation is significantly greater in children than in normally sighted adults for contrast sensitivity, but not for alignment sensitivity. In normal eyes, the mean binocular summation ratio for the fovea and the peripheral field have been found to be not significantly different, however in amblyopic eyes, subjects show no or minimal binocular summation in the foveal region but reach normal ratios in the periphery.5 Binocular summation of contrast signals has been proved to decline with age, independent of inter-ocular differences.46–50 However, contrary results have also been reported51 with absence of age effects on binocular summation, when compared for resolution acuity, contrast sensitivity (CS), and spatial interval (SI) hyperacuity.
Binocular vision anomaliesBinocular vision anomalies include: diplopia (two images of a single object are seen), visual confusion (the perception of two different images superimposed onto the same space), suppression (where the brain ignores all or part of one eye's visual field), heterotropia or strabismus (inability to direct both eyes simultaneously toward the same fixation point), horror fusionis (an active avoidance of fusion by eye misalignment), and anomalous retinal correspondence (where the brain associates the fovea of one eye with an extra-foveal area of the other eye).
Several models have explored the mechanism of binocular interactions,52,53 interocular contrast and masking.54 In more recent times, psychophysical evidence has emerged for two routes to suppression in primary visual cortex before binocular summation of signals in human eyes.55 Schor et al.56 compared the binocular depth of focus of monovision wearers to the sum of the two monocularly determined depths of focus. Their results demonstrate the effectiveness of interocular suppression of anisometropic blur in monovision correction and the influence of ocular dominance upon this suppression process. Accommodative response to sinusoidal variations in blur is controlled primarily by the dominant sighting eye.
Pineles et al.57 studied binocular summation in strabismic populations without amblyopia. The authors hypothesized that strabismus may lead to decreased binocular summation for tasks related to discrimination within increased background complexity. Their goal was to test the extent of binocular summation in patients with strabismus during discrimination of a luminance target disk embedded in visual noise. Their findings supported the hypothesis that strabismus can lead to decreased binocular summation and even binocular inhibition. Despite literature showing enhanced binocular summation in visually demanding situations such as high levels of visual noise or low contrast, binocular summation was not significantly affected by visual noise in their study population. Raveendran et al.58 suggested that fixation stability in the amblyopic eye appears to improve with bifoveal fixation and reduced interocular suppression. However, once initiated, bifoveal fixation is transient with the strabismic eye drifting away from foveal alignment, thereby increasing the angle of strabismus.
Strabismic amblyopia is typically associated with several visual deficits, including loss of contrast sensitivity in the amblyopic eye and abnormal binocular vision. Conventionally binocular summation ratios provide an operational index of clinical binocular function, but does not assess whether neuronal mechanisms for binocular summation of contrast remain intact. Baker et al.59 investigated this question by comparing the conventional method to horizontal sine-wave gratings used as stimuli (3 or 9 cycles per degree; 200ms) where the contrast in the amblyopic eye was adjusted (normalized) to equate monocular sensitivities. They found that when normal observers performed the experiments with a neutral-density (ND) filter in front of one eye, their performance was similar to that of the amblyopes in both methods of assessment indicating that that strabismic amblyopes have mechanisms for binocular summation of contrast and that the amblyopic deficits of binocularity can be simulated with an ND filter.
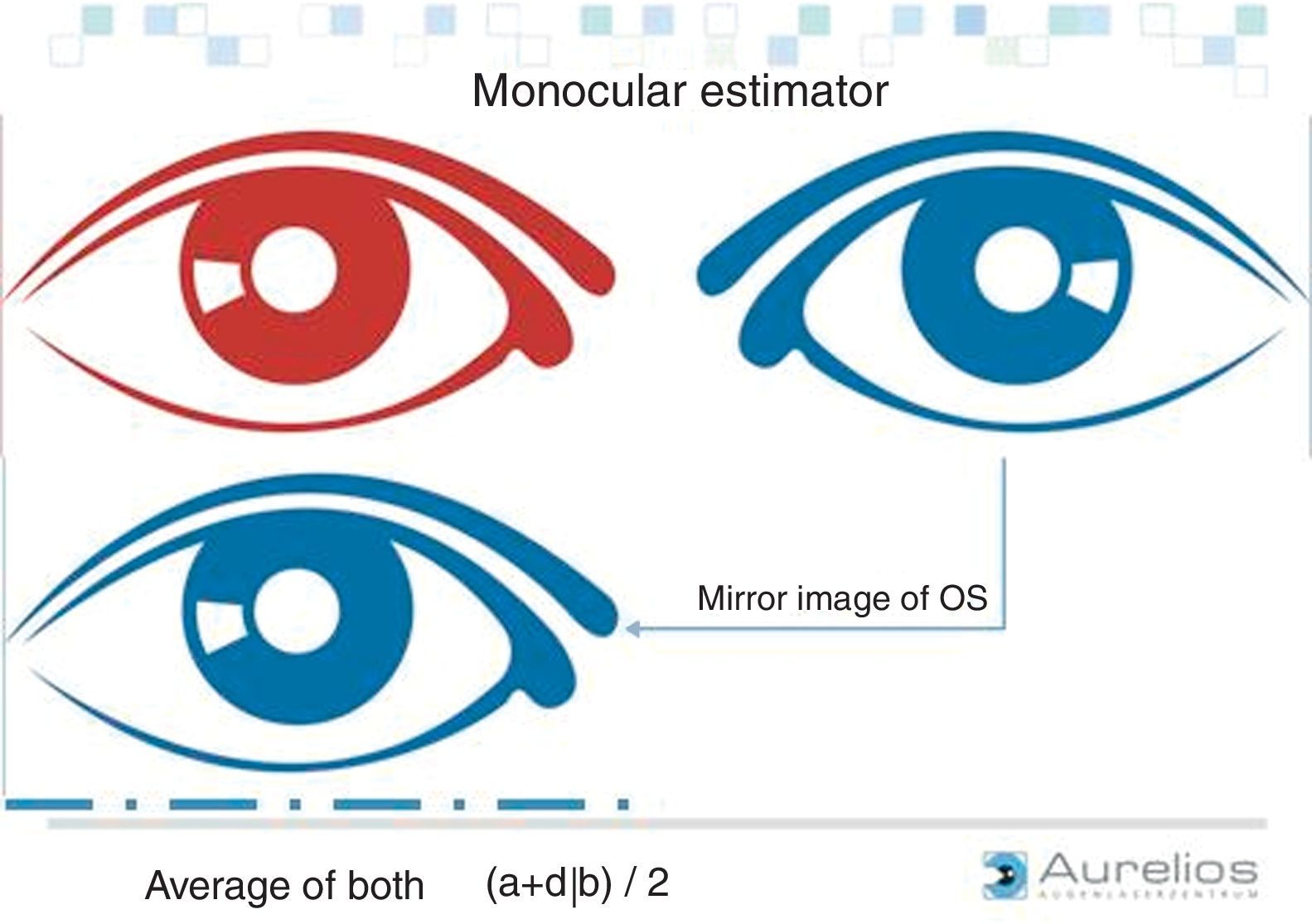
Importance of preserving bilateral symmetry in ocular surgeryConsidering the findings presented in the above mentioned studies and particularly an uncommon occurrence of anisometropia44 (which considers the most dominant aberrations of the eye), one could strongly consider a high symmetry between radial aberrations in the left and right eye. Furthermore, considering the pattern and orientation of higher order aberrations in relevance to bilateral symmetry, one can infer that ocular and corneal aberrations tend to be similar for not only radial but also vertical aberrations (with binocular summation being highest along the vertical meridian60). The horizontally oriented aberrations however shall be symmetric due to the relationship between the two eyes in the horizontal direction. Therefore, it is expected that the 0 Zernike modes61 show even symmetry; negative odd modes show even symmetry; negative even modes show odd symmetry; positive odd modes show odd symmetry and positive even modes show even symmetry. Many of these symmetric associations between the right and left eye could be explained by the symmetry in the pupil offset and the visual axis which is always nasal in both eyes.
Katsumi et al.62,63 found that when identical patterns were delivered to each eye and the patterns were fused, the binocular visually evoked response (VER) demonstrated larger amplitude than the monocular VER, resulting in a binocular summation that is prominent in the low-contrast stimulus pattern. With stimulus patterns of higher contrast, the amplitudes of the binocular and the monocular VER did not differ greatly, and the value of binocular summation was significantly decreased. Experimental results even show that binocular aberration correction benefits for visual acuity and contrast sensitivity increase with decreasing luminance.64 Also, the advantage of binocular over monocular viewing increases when visual acuity becomes worse. The findings suggest that binocular summation mitigates poor visual performance under low luminance conditions. Furthermore, a pseudo-canceling of the horizontally oriented aberrations of each eye enhances the binocular vision. Strong inter-ocular disparity detrimentally affects the binocular summation,40,65–67 severely affecting vision, leading to conditions like amblyopia (for e.g. strabismic, anisometropic and form vision deprivation amblyopia)44,68–70 and nystagmus (when the visual axes of the two eyes are far apart).71,72 All these relationships clearly point to the critical importance of maintaining (and at best improving) the existing bilateral symmetry of eyes, after an ocular surgical procedure.
Bilateral symmetry and ocular surgeryLaser based refractive correctionVery few studies in the literature have addressed the issue of analyzing the symmetry of aberrations between eyes after corneal laser refractive surgery. Refractive surgical procedures are mostly performed monocularly with different ablation profiles and popular techniques.73–76 It is significant to evaluate how a monocularly performed refractive procedure influences the inter-ocular symmetry.
Castro et al.77 determined the influence of inter-ocular differences in retinal image quality on binocular visual performance. They found that higher the inter-ocular differences in the Strehl ratio, the lower the binocular summation. Jiménez et al.78 found that binocular summation and maximum disparity significantly decrease with increasing inter-ocular differences in higher-order aberrations (total, coma, and spherical aberration) in both eyes of 35 emmetropic observers, scanned with a Wasca aberrometer (Carl Zeiss Meditec, Inc.). Jiménez et al.65 also analyzed the binocular visual function after laser-assisted in situ Keratomileusis (LASIK). They evaluated visual performance, monocular and binocular contrast sensitivity function and disturbance index for quantifying halos in 68 patients (136 eyes). Binocular summation and disturbance index diminished significantly (p<.0001) after LASIK with increasing inter-ocular differences in corneal and eye aberrations. They found that inter-ocular differences above 0.4μm of the root-mean-square (RMS) for a 5-mm analysis diameter, lead to a decrease of more than 20% in binocular summation. They concluded that the binocular function deteriorates more than monocular function after LASIK. This deterioration increases as the inter-ocular differences in aberrations and corneal shape increase. Similar findings were reported by Villa et al.79 They tested the visual performance after LASIK for a corneal asphericity (Q)-optimized ablation and Munnerlyn formula based ablation algorithm. They showed deterioration in aberrometry, CSF, binocular summation, and discrimination index for the two tested algorithms, although significantly lower deterioration was observed for the Q-optimized algorithm. Other studies80–84 also showed that conventional LASIK significantly increases ocular higher-order aberrations, which compromise the postoperative CSF specially for high spatial frequencies under mesopic conditions.
Contrary to these findings, Boxer Wachler85 reported statistically significantly better binocular visual acuity and contrast sensitivity than the visual acuity in the better eye (p=0047 to<0001) in both groups of 20 postoperative LASIK and 20 non-LASIK ametropic patients. However, they reported statistically significantly smaller pupil diameter in both groups under binocular condition compared to the monocular condition (p<0001). Keir et al.86 reported that despite an increase in HOA's, wavefront-guided LASIK yields excellent visual acuity and contrast sensitivity.
Another important aspect in maintaining the bilateral symmetry is the morphology of the LASIK flaps, where LASIK flaps created with a femtosecond laser have shown to preserve the symmetry and regularity in flap morphology with a more regular planar shape in comparison to a meniscus shape in the flaps created with a mechanical microkeratome.87,88 Arbelaez et al.89 compared the preoperative and postoperative bilateral symmetry between OD and OS eyes that have undergone femto-LASIK using Aberration-neutral ablation profiles. They presented measurements of the corneal wavefront aberration in 50 eyes (right and left eyes of 25 subjects) and analyzed the correlation of individual aberrations across the population, as well as the correlation of aberrations between the right and left eyes of the same subjects. Preoperatively 11 out of 33 Zernike terms showed significant OS-vs.-OD bilateral symmetry, whereas at 6 months postoperatively 12 Zernike terms showed significant OS-vs.-OD symmetry. Preoperatively, only 6 (C[4,−4], C[4,−2], C[5,+3], C[6,+6], C[7,−7], C[7,+3]) Zernike terms were significantly different when comparing OS vs. OD for the same subject, whereas at 6 months postoperatively 8 terms (C[4,−2], C[4,+4], C[5,+1], C[6,−6], C[6,−4], C[6,+2], C[7,−5], C[7,+3]) were significantly different. For all of them, the differences were well below the clinical relevance. Preoperatively, 23 of 25 patients showed significant OS-vs.-OD bilateral symmetry whereas at 6 months postoperatively 22 of 25 patients showed significant OS-vs.-OD bilateral symmetry. They concluded that the treatment maintained the global OD-vs.-OS bilateral symmetry, as well as the bilateral symmetry between corresponding Zernike terms contributing to the bilateral summation. Recognizing the high levels of defocus and astigmatism in their study population, the achieved results showed significant success in retaining bilateral symmetry using aberration neutral profiles.
Correction of spherical (SA) and longitudinal chromatic aberrations (LCA) has shown to have significant implications on monocular visual acuity.90 Schwarz et al.90 investigated the visual effect of SA correction in polychromatic and monochromatic light on binocular visual performance, using a liquid crystal based binocular adaptive optics visual analyzer capable of operating in polychromatic light. They found that the binocular visual acuity improves when SA is corrected and LCA effects are reduced separately and in combination, resulting in the highest value for SA correction in monochromatic light. Similar findings were reported by Zheleznyak et al.91 in reference to modified monovision with SA.
A shift from binocular summation to binocular inhibition is observed when there is a significant decrease in contrast sensitivity or reduced retinal illuminance in one eye compared to the other as in cases of unilateral cataract and amblyopia. Subramaniam92 studied how binocular function in post-LASIK subjects with unsatisfactory outcomes is influenced by differences between the two eyes in visual acuity and contrast sensitivity. He found that binocular inhibition in post-LASIK subjects increases as the visual sensitivity difference between the two eyes increases.
Many studies have explored outcomes in wavefront-guided and topography guided photorefractive keratectomy (PRK) in comparative studies,93,94 in terms of HOA's,95 post-surgical corneal shape,96 and improved uncorrected and spectacle-corrected visual acuity.97,98 Some studies have also addressed the subject of bilateral symmetry after PRK treatments. Rao et al.99 described the symmetry of response in fellow eyes of 133 patients undergoing bilateral myopic PRK. They reported that among 84 patients with similar preoperative myopia in both eyes, 54 (64.3%) patients had a postoperative spherical equivalent difference less than or equal to 1D in fellow eyes. Risk factors for asymmetric response among fellow eyes included increasing preoperative myopia (p<0.001) and dissimilar treatment technique in the two eyes (p=0.03). This study demonstrated that considerable symmetry of response exists in fellow eyes of patients undergoing myopic PRK. These findings were similar to other studies100,101 performed with smaller cohorts.
Presbyopia is commonly treated with traditional surgical approached like monovision, and more recently by corneal small aperture inlays,102 in both cases at the cost of binocular summation. Schwarz et al.103 compared the performance of corneal inlays with monovision. They measured binocular visual acuity as a function of object vergence in three subjects by using a binocular adaptive optics vision analyzer. Visual acuity was measured at two luminance levels (photopic and mesopic) under several optical conditions like natural vision (4mm pupils, best corrected distance vision), pure-defocus monovision (+1.25D add in the nondominant eye), small aperture monovision (1.6mm pupil in the nondominant eye), and combined small aperture and defocus monovision (1.6mm pupil and a +0.75D add in the nondominant eye). Visual simulations of a small aperture corneal inlay suggested that the corneal inlays extend depth of focus as effectively as traditional monovision in photopic light, but at the cost of binocular summation.
Ocular surgery beyond refractive correctionVisual deprivation disrupting binocular development, such as that occurring with congenital cataract, is reported to cause asymmetric monocular optokinetic nystagmus (MOKN), as well as poor sensory and motorfusional outcome. Hwang et al.104 tested MOKN with video and electro-oculographic recordings and stereoacuity in 5 patients with good visual acuity and satisfactory ocular alignment after surgery for congenital cataract. Their tests suggested that MOKN symmetry develops along with good stereopsis, but the quality of stereopsis necessary for development of MOKN symmetry remained unclear. Leffler et al.105 predicted the postoperative refractive astigmatism in the second eye undergoing cataract surgery using standard biometry and information obtained from the first eye. They found that the refractive with-the-rule astigmatism observed postoperatively in the first eye is a strong independent predictor of postoperative with-the-rule astigmatism in the second eye. Keratometric oblique astigmatism in the first eye is a weak but statistically significant independent predictor of postoperative oblique astigmatism in the second eye. Both findings were consistent with the mirror symmetry of the corneas about the midsagittal plane.
It has been previously shown106 that assessing the indication for and outcomes of cataract surgery, analysis of visual function should include measures of both eyes, rather than measures of the operative eye only, as differences between the eyes may play an important role in binocular measures such as stereopsis. Substantial benefit of binocular vision has been recently reported in individuals with bilateral multifocal IOL implantation in terms of increased visual acuity. Tsaousis et al.107 investigated the effect of binocularity on long-term visual acuity in twenty patients (9 men and 11 women) with an average age of 70±7 years (range: 56–78 years), who underwent bilateral implantation of a diffractive multifocal IOL. Uncorrected distance visual acuity (UDVA) improved from 0.07±0.10 and 0.21±0.12logMAR (better and worse respectively) to 0.00±0.09logMAR binocularly. Uncorrected near visual acuity (UIVA) improved from 0.18±0.14 and 0.32±0.15logMAR (better and worse respectively) to 0.08±0.15logMAR binocularly. Uncorrected near visual acuity (UNVA) improved from 0.20±0.09 and 0.32±0.12logMAR (better and worse respectively) to 0.11±0.10logMAR (20/26 Snellen) binocularly. Binocular summation was found to be statistically significant at all distances. Pseudophakic monovision using monofocal intraocular lenses has even been projected as an effective approach for managing loss of accommodation after cataract surgery in patients older than 60 years; Ito et al.108 examined 82 patients (age 49–87 years) with pseudophakic monovision using monofocal intraocular lenses. They reported binocular summation observed at 1.5–6.0 cycles per degree, near stereopsis up to 100″, and 81% overall satisfaction rate. However symptomatic patients have shown to benefit from second eye cataract extraction with lens implantation.109,110
The role of binocular function can be very important in conditions related to body's natural aging process. Luminita Tarita-Nistor et al.111 examined two aspects of binocular function in patients with age-related macular degeneration (AMD): summation/inhibition of visual acuity and rivalry. The performance of 17 patients with AMD was compared with that of 17 elderly controls and 21 young people. Binocular ratios, defined as the better-eye acuity divided by the binocular acuity, were calculated. They also measured eye dominance during rivalry (proportion of time the participants reported perceiving the input to each eye) and rivalry rates (number of alternations per minute). Their results showed that while overall binocular ratios were similar for the three groups, the frequency distributions of people who experienced inhibition, equality or summation were different for the young and AMD groups. In the rivalry test, patients experienced more piecemeal perception than the elderly and young controls, but time dominance from the better-seeing eye was comparable for the three groups. Rivalry rates decreased with age and further with pathology. Moreover, rivalry time dominance of the worse-seeing eye was negatively correlated with inter-ocular acuity differences for the AMD group.
DiscussionIf the optical system of the eye is rotationally symmetric about an optical axis which does not coincide with the visual axis, measurements of refraction and aberration made along the horizontal and vertical meridians of the visual field will show asymmetry about the visual axis.112 Charman et al.113 modeled this departure from symmetry for second-order aberrations, refractive components and third-order coma. The experimental data supports the concept that departures from symmetry about the visual axis in the measurements of crossed-cylinder astigmatism J(45) and J(180) are largely explicable in terms of a decentred optical axis. The association between peripheral astigmatic asymmetry and angle alpha was studied by Dunne et al.114; their results indicate that either peripheral astigmatic asymmetry is due to additional factors such as lack of symmetry in the peripheral curvature of individual optical surfaces, or that there is further misalignment of optical surfaces away from an optical axis. Specific to laser based refractive procedures, the importance of choosing the correct ablation centration has been pointed out time and again,112 with the correction of decentration also showing reduction in corneal HOAs, including the coma-like aberrations and spherical aberration.115 The main post-op HOAs effects (coma and spherical aberration) in refractive procedures are caused by decentration and “edge” effects: i.e., the strong local curvature changes between the optical zone (OZ) and the transition zone (TZ) and from the TZ to the non-treated cornea. As a result, it is necessary to emphasize the use of large OZs, covering the scotopic pupil size plus tolerance for possible decentration, as well as well-defined TZ.
Classical data on the detection of simple patterns shows that two eyes are more sensitive than one eye.116 The degree of binocular summation is important for inferences about the underlying combination mechanism. In a signal detection theory framework, sensitivity is limited by internal noise. If the noise is added centrally after binocular combination, binocular sensitivity is expected to be twice as good as monocular. If the noise is added peripherally at each eye prior to combination, binocular sensitivity will be sqrt[2] times higher than monocular.116 This strongly indicates the importance of maintaining and at best improving the bilateral symmetry and binocular fusion in an ideal ocular surgical procedure. Not manipulating the visual print of the patient while performing best spectacle correction, is gaining popularity in the form of aberration neutral profiles117 in refractive surgery. If the aimed aberration-neutral concept would be rigorously achieved in a refractive procedure, the bilateral symmetry between eyes would be automatically obtained, considering the high symmetry between lower order radial and vertical aberrations in the left and right eye.
Limited number of studies have evaluated the after effect of refractive surgery on bilateral symmetry. Furthermore, for the studies focusing on this topic,29,89 the method to determine whether or not symmetry is maintained consist of comparing individual terms in a variety of ad hoc ways both before and after the refractive surgery, ignoring the fact that retinal image quality for any given individual is based on the sum of all terms. The analysis of bilateral symmetry should be related to the patients’ binocular vision status.118 The role of aberrations has not been evaluated precisely in relation to the visual ability. A patient with a high level of aberrations can have an excellent visual acuity and vice versa, additionally a patient may not have good stereopsis but may show good aberration symmetry. Furthermore, these relationships have been majorly studied monocularly; evaluating them for binocular vision poses new challenges. The role of inter-ocular differences have been studied partially40 and have shown a significant influence on binocular performance, suggesting that even subtle differences must be considered significant for visual performance. Analysis of bilateral symmetry as a function of the analysis diameter is also not extensively explored. All these possibilities suggest that the future holds great potential for investigating the role of bilateral symmetry in the human vision and its influence in developing improved ocular surgical procedures. Particularly for preserving the bilateral symmetry in the eyes after laser based refractive procedures, biomechanical response of the cornea,119,120 ablation centration,112 epithelial thickness profile,121,122 and the role of HOA of the cornea117 should be extensively investigated.
Conflict of interestsNo author has a proprietary or financial interest in the materials presented herein. Dr. Samuel Arba Mosquera and Mr. Shwetabh Verma are employees of SCHWIND eye-tech-solutions.