Although previous studies suggest that orthokeratology contact lens wear slows eye growth in children with progressing myopia, some limitations in the methodology employed have become evident. Furthermore, the safety of this modality of visual correction has not been assessed. The study “Myopia Control with Orthokeratology Contact Lenses in Spain” (MCOS) is being conducted to compare axial length growth between white European myopic children wearing orthokeratology contact lenses (OK) and wearing distance single-vision spectacles (SV). Additionally, the incidence of adverse events and discontinuations is also recorded. We outline the methodology and baseline data adopted.
MethodsSubjects aged 6 to 12, with myopia ranging from 0.75 to 4.00 D and astigmatism ≤1.00 D were prospectively allocated OK or SV correction. Measurements of axial length, anterior chamber depth, corneal topography, cycloplegic autorefraction, visual acuity and corneal staining are performed at 6-month intervals. The incidence of adverse events and discontinuations are also recorded.
ResultsThirty one children were fitted with OK and 31 with SV correction. Eight subjects did not meet the refraction-related inclusion criteria for enrollment. No significant differences were found in baseline mean age and refractive and biometric data betwseen the two groups (P>0.05). No adverse events were found in any of the two groups at baseline.
ConclusionTo the authors’ knowledge, MCOS is the first prospective clinical trial to assess the safety and efficacy of orthokeratology contact lens wear to slow myopia progression vs. single-vision spectacle wear. The MCOS offers a number of notable features: prospective design; well-matched samples and high-resolution ocular biometry measures, which should collectively elucidate whether orthokeratology contact lens wear is a feasible and safe method for myopia-progression control.
A pesar de que estudios previos sugieren que el uso de lentes de contacto para ortoqueratología ralentizan el crecimiento ocular en niños con miopía progresiva, ha quedado de manifiesto algunas limitaciones en la metodología empleada en dichos estudios. Además, hasta la fecha no se ha evaluado la seguridad de esta modalidad de corrección visual. El estudio “Control de la miopía con lentes de contacto para ortoqueratología en España” (MCOS, según sus siglas en inglés) se está llevando a cabo para evaluar el aumento de la longitud axial ocular en niños miopes europeos de raza blanca, usuarios de lentes de contacto de ortoqueratología frente a usuarios de gafas monofocales. Además, también se está evaluando la incidencia de reacciones adversas y abandonos. En este artículo explicamos la metodología empleada, así como los datos iniciales del estudio.
MétodosSe asignó de manera prospectiva corrección OK o SV a sujetos de entre 6 y 12 años de edad, con una miopía comprendida entre 0,75 y 4,00 D y con astigmatismo ≤1,00 D. Se llevan a cabo, inicialmente y cada 6 meses, medidas de la longitud axial, profundidad de la cámara anterior, topografía corneal, de autorrefracción cicloplégica, agudeza visual y tinción corneal. Además, se está evaluando la incidencia de reacciones adversas y abandonos.
ResultadosA 31 niños se les adaptó corrección OK y a 30 corrección SV. Ocho sujetos no cumplían el criterio de inclusión relativo a la refracción. No se encontraron diferencias significativas entre los dos grupos en lo que respecta a edad media y a valores de refractivos y biométricos (P>0.05). No se encontraron reacciones adversas en ninguno de los 2 grupos en la visita inicial.
ConclusionesSegún el conocimiento de los autores, el MCOS es el primer ensayo clínico prospectivo en el que se evalúa la seguridad y eficacia del uso de lentes de contacto ortoqueratológicas para ralentizar el avance de la miopía, comparando los resultados con los obtenidos en un grupo de control compuesto por usuarios de gafas monofocales para miopía. El estudio MCOS tiene una serie de características destacables: diseño prospectivo; muestras bien emparejadas, medidas de biometría ocular de alta resolución; todo ello debería permitir dilucidar si el uso de lentes de contacto ortoqueratológicas es un método factible y eficaz para frenar la progresión de la miopía en niños.
The prevalence of myopia in young adolescents has increased substantially over recent decades and is now approaching 10-25% and 60-80% in industrialized societies of Western and Eastern Asia, respectively;1 worldwide, the condition is considered to be the leading cause of visual impairment.2 In clinical terms, it is widely acknowledged that the myopic eye is a vulnerable eye, especially for myopia levels greater than 6.00 D, and one that is especially susceptible to a range of ocular pathologies.3-7 Several treatment therapies, including rigid contact lenses, bifocal and multifocal spectacle lenses as well as pharmaceutical agents, have been used in the past with relatively modest success to eliminate or, at least, reduce myopia progression.8,9 More recently, modern orthokeratology has claimed to be effective in slowing the progression of myopia in children. This technique is an effective treatment for the temporary reduction of up to -6.00D of myopia with the overnight use of reverse-geometry gas-permeable contact lenses.10 Usually, studies evaluating the effect of orthokeratology lens wear on myopia progression measure changes in the eye's axial length, the principal structural correlate of refractive error,11 due to the concomitant temporary reduction in myopia that occurs as a consequence of the corneal flattening induced by orthokeratology contact lens wear.12
Although a retrospective study13 and a case report14 on the subject were previously published, only two prospective studies have assessed the effect of orthokeratology contact lens wear on myopia progression in children.15,16
Over a two-year period, Cho et al.15 monitored the increase in axial length in 35 Hong-Kong Chinese children aged 7 to 12 who were fitted with orthokeratology lenses, and compared the rate of change of axial length with that observed in a historical control group made up of 35 children wearing single-vision spectacles. Both groups were matched for age, gender and baseline spherical equivalent refractive error. At the end of the 24 months, the increase in axial length was 0.29±0.27 mm and 0.54±0.27 mm for the orthokeratology lenses and single-vision spectacle groups, respectively. However, the study failed to recruit a prospective control group. Furthermore, the baseline level and progression of myopia observed among Chinese children are reported to be significantly greater than among white European children.8 In addition, differences in contact-lens-induced responses in the corneas of Asian and non-Asian subjects have also been previously observed.17
More recently, a study undertaken in the USA by Walline and co-workers16 compared the growth of the eye observed among myopic children wearing orthokeratology contact lenses with that observed in a historical control group of children wearing soft contact lenses. The groups consisted of children aged 8 to 11 with myopia ranging from 0.75 to 4.00 D and having less than 1.00 D of astigmatism. Over the two-year period, the axial length for the soft-contact-lens group increased, on average, 0.32 mm more than for the orthokeratology-lens group. However, the Walline et al.16 study was unable to recruit a prospective control group. Since Cho et al.15 and Walline et al.16 employed historical prospective control groups, subjects were not randomized into one modality of visual correction vs. another. Additionally, these two previous studies measured axial-length growth using A-scan ultrasonography.15,16 An alternative measuring method (the Zeiss IOLMaster) uses partial coherence interferometry to carry out non-contact measures of axial length with a dioptric resolution of 0.03 D (an order of magnitude better than the 10 Hz ultrasound technique).18
As with any treatment regimen, both efficacy and safety need to be assessed. Although case reports and case series of observations on undefined populations of participants wearing overnight orthokeratology contact lenses have been presented, there are no formal prospective reports on the incidence of adverse events associated with overnight orthokeratology contact lenses specifically used to treat myopia.19
This report introduces the study designated as MCOS (Myopia Control with Orthokeratology contact lenses in Spain) and outlines its design, methodology and baseline findings. The primary outcome measure of MCOS is to compare differences in axial length growth between white European myopic children wearing orthokeratology contact lenses (OK) and distance single-vision spectacles (SV) over a 2 year period. The secondary outcome is to record differences in the incidence of adverse events and discontinuations between the two study groups. To the authors’ knowledge, the MCOS study is the first prospective clinical trial to assess the safety and efficacy of overnight orthokeratology contact lens wear.
MethodsSample sizeThe study's sample size was calculated using a statistical power analysis software (JMPIN 4.0.2, SAS Institute Inc., NC, USA) based on data from previous clinical trials.15,16 Assuming that the standard deviation of the change in axial length over a two-year period is 0.27 mm and taking a statistical power of 0.90, a sample size of 25 subjects per group is needed to be able to detect a difference of variation in axial length equal to 0.25 mm (equivalent to approximately 0.75 D)20 at P=0.05. Previous studies have reported drop-out rates of approximately 17% among OK15 and SV21 subjects enrolled in clinical trials. Therefore, to account for attrition, the number of subjects to be recruited in this study was taken to be at least 29 per group.
Method of RecruitmentSubjects were sought through advertisements in local newspapers, among individuals attending the clinic where the study was to be undertaken, by word-of-mouth and by randomly mailing the area of Madrid.
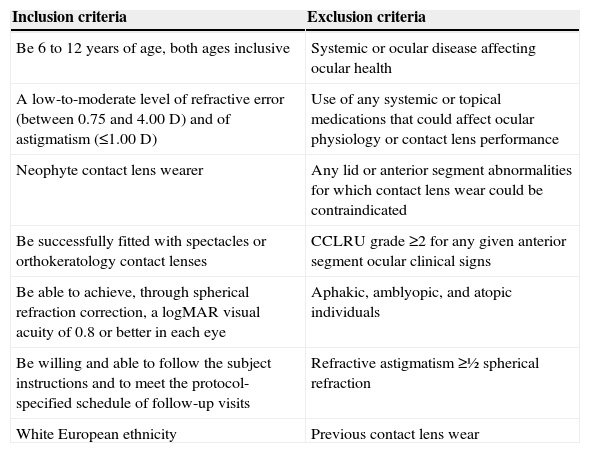
Recruitment Session and Follow-up VisitsThe objectives of the recruitment session were to determine whether or not the children met the inclusion and exclusion criteria for the study (Table 1) and to inform the child's parent(s) or guardian(s) verbally and in writing about the nature of the study. During this session, parent(s) or guardian(s) were given a balanced account of the advantages and disadvantages of the two vision correction modalities offered in the study (i.e. SV or OK). Particular care was taken not to suggest that one modality might perform better than the other or provide a better control over myopia progression. Parent(s) or guardian(s) were also informed that for the whole duration of the study (2 years) children would obtain visual correction (i.e. glasses or contact lenses) made to their prescription, contact lens care solutions (for the OK group only) and full ocular examinations free of charge. After parent(s) or guardian(s) chose one of the two modalities offered, full informed consent and child assent were obtained prior to the start of all experimental work and data collection. The informed consent also included detailed information regarding the potential adverse reactions that might occur as a result of contact lens wear (e.g. microbial keratitis). Patient participation in the study could be discontinued at the examiner's discretion should significant symptoms or slit-lamp findings occur. Subjects were instructed that they could withdraw from the study anytime. All measurements were obtained at Clinica Oftalmológica Novovision (Madrid, Spain). The study protocol was reviewed and approved by the Institutional Review Board. No Ethics Committee Aproval was required; otherwise, the study followed the tenets of the Declaration of Helsinki.
Inclusion and exclusion criteria
| Inclusion criteria | Exclusion criteria |
| Be 6 to 12 years of age, both ages inclusive | Systemic or ocular disease affecting ocular health |
| A low-to-moderate level of refractive error (between 0.75 and 4.00 D) and of astigmatism (≤1.00 D) | Use of any systemic or topical medications that could affect ocular physiology or contact lens performance |
| Neophyte contact lens wearer | Any lid or anterior segment abnormalities for which contact lens wear could be contraindicated |
| Be successfully fitted with spectacles or orthokeratology contact lenses | CCLRU grade ≥2 for any given anterior segment ocular clinical signs |
| Be able to achieve, through spherical refraction correction, a logMAR visual acuity of 0.8 or better in each eye | Aphakic, amblyopic, and atopic individuals |
| Be willing and able to follow the subject instructions and to meet the protocol-specified schedule of follow-up visits | Refractive astigmatism ≥½ spherical refraction |
| White European ethnicity | Previous contact lens wear |
D: diopters; CCLRU: Cornea and Contact Lens Research Unit.
At the recruitment session, all subjects underwent a full anterior segment examination, indirect fundus microscopy, binocular vision and refractive evaluations to elucidate whether or not they were eligible to participate in the study. Subsequently, baseline study measurements were performed in eligible subjects (see below for further details on the measurement procedures).
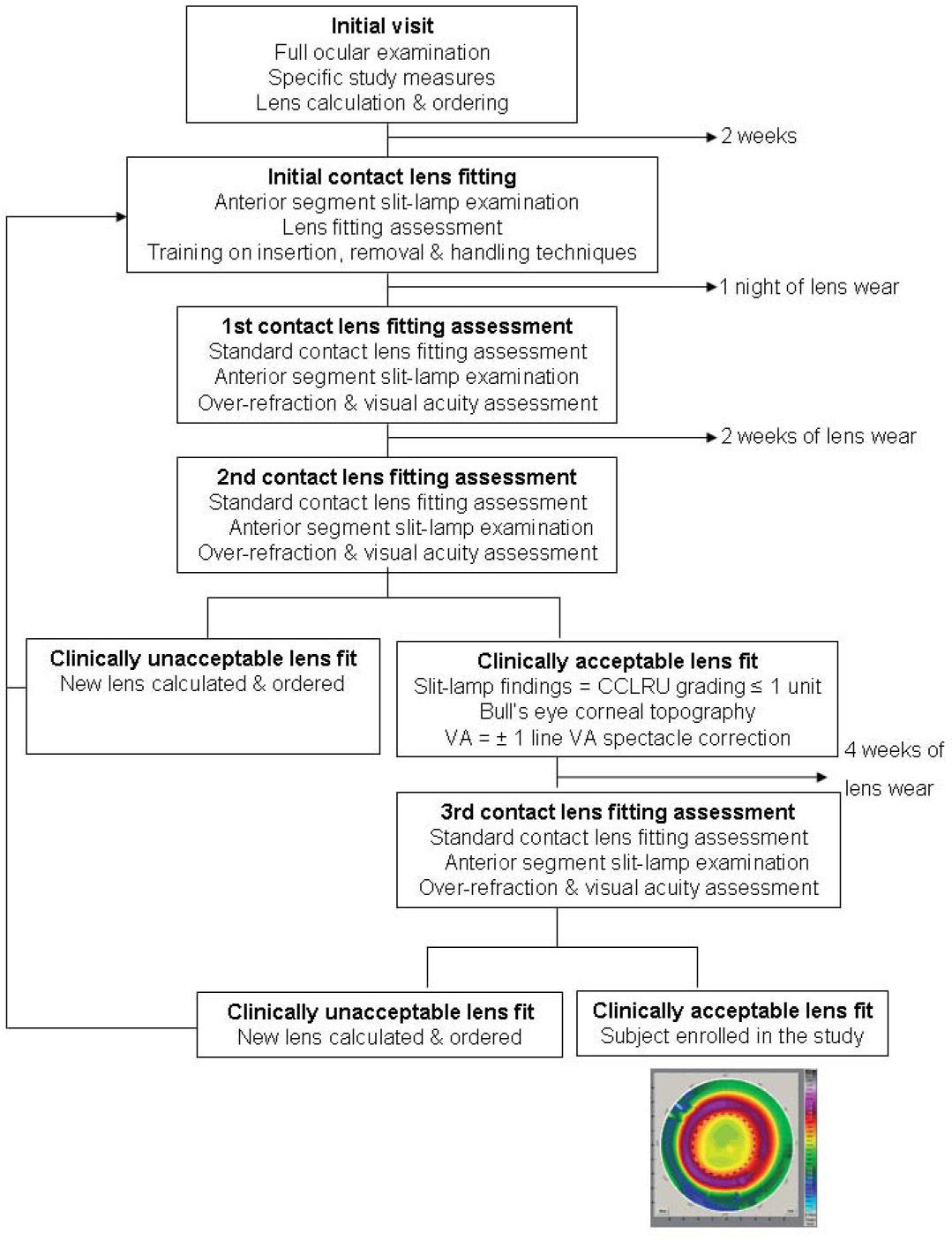
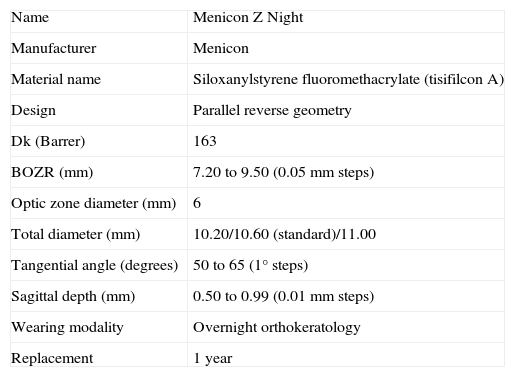
Subjects in the SV group were prescribed distance single-vision spectacles having the highest positive power consistent with optimum visual acuity and were asked to wear the spectacles at all times. Subjects in the OK group were fitted with Menicon Z Night contact lenses (Table 2) using the Menicon Professional Easy Fit Software (Figure 1) (Menicon Co., Ltd, Nagoya, Japan). Corneal topography and cycloplegic refraction data for both eyes of each subject were input into the software, which automatically calculated the specifications of the Menicon Z Night trial lens to allow orthokeratology fitting. Contact lenses were ordered and subjects from the OK group were rescheduled for an appointment approximately two weeks later. After the initial contact lens fitting, on the first day all contact lens subjects were instructed in the procedures for contact lens insertion, removal and cleaning/disinfection and these instructions were reinforced in subsequent visits. Subjects were provided with MeniCare Plus multipurpose solution for daily cleaning, rinsing and disinfecting of their contact lenses, and also Menicon Progent intensive cleaner, to be used once a week (Menicon Co., Ltd, Nagoya, Japan).
Menicon Z Night contact lens specifications
| Name | Menicon Z Night |
| Manufacturer | Menicon |
| Material name | Siloxanylstyrene fluoromethacrylate (tisifilcon A) |
| Design | Parallel reverse geometry |
| Dk (Barrer) | 163 |
| BOZR (mm) | 7.20 to 9.50 (0.05 mm steps) |
| Optic zone diameter (mm) | 6 |
| Total diameter (mm) | 10.20/10.60 (standard)/11.00 |
| Tangential angle (degrees) | 50 to 65 (1° steps) |
| Sagittal depth (mm) | 0.50 to 0.99 (0.01 mm steps) |
| Wearing modality | Overnight orthokeratology |
| Replacement | 1 year |
Dk: oxygen permeability; BOZR: back optic zone radius.
Subjects in the OK study group were informed that contact lenses had to be inserted every day, just before going to sleep, and removed the following morning. Subjects were requested to attend no later than two hours after lens removal on the morning following the first night of lens wear. A subsequent visit was scheduled for three weeks later to ascertain whether or not the contact lens fitting was clinically acceptable; otherwise, new contact lenses were calculated and ordered. An orthokeratology fit was considered to be successful if after three weeks of lens wear, the subject showed a CCLRU score regarding the anterior eye segment signs ≤1 unit,22 a “bull's eye” corneal topography pattern and monocular and binocular visual acuities within ±1 line of the best-correct decimal spectacle visual acuity. Subjective over-refraction was undertaken to ascertain whether changes in the contact lens base curve were required. If so, new lenses were ordered for the subjects while maintaining the same design specifications for the contact len's back surface. In the event of an unsuccessful fitting (i.e. flat- or steep-fitting lenses), the Menicon Professional Easy Fit Software was used to calculate alternative contact lenses that would constitute a successful lens fit; this tool is included in the Menicon software.
It was made clear to all OK subjects that they had to remove their contact lenses if they experienced any sort of problem. Subjects and their parent/guardians were instructed in the steps to take in the event of an adverse reaction, and were instructed to ensure adherence to the study protocol. Moreover, compliance was monitored closely by one of the authors (CV-C). Subjects from both study groups were advised to report/turn up at the clinic immediately should events not considered normal (e.g. red eye, pain, unusual discomfort, unusual eye secretions) occurred.
After initial enrolment, subjects are seen again at the scheduled 1-, 6-, 12-, 18- and 24–months follow-up visits. To prevent subjects from forgetting their follow-up appointments, all subjects receive a telephone reminder one day before their appointment. Follow-up visits are scheduled to fall within two hours of awakening. A decrease in one line of visual acuity accompanied by a change in subjective refraction23 at any one of the follow-up visits was considered to be clinically significant and was remedied by supplying new contact lenses or spectacles made to their new prescription.
MeasurementsCycloplegic auto-refractionThree drops of chlorhydrate cyclopentolate 1% (Alcon Cusí, Masnou, Barcelona, Spain) were instilled 10 minutes apart in each of the subjects’ eyes using a multidose bottle. Ten minutes after instillation of the third drop, three auto-refraction measurements were taken (Topcon RM 8000B, CA, USA) and their mean was calculated. Additionally, distance subjective refraction was also performed before and after cycloplegia.
Corneal TopographyCorneal topography measurements were performed with the Wavelight Allegro Topolyzer (WaveLight Laser Technologies AG, Erlangen, Germany). The first measurement taken in each eye, which provided an optimum index value according to the manufacturer's recommendations, was used for the study. Furthermore, the measurement generated a simulated central keratometry reading as well as the rate of peripheral corneal flattening/steepening with displacement from the corneal apex, the latter indicating the degree to which an aspheric surface differs from the spherical form (i.e. e-value).24
Axial Length, Anterior Chamber Depth and Posterior Segment Depth MeasurementsMeasurements of axial length and anterior chamber depth were performed with the Zeiss IOLMaster (Carl Zeiss Jena GmbH, Jena, Germany).18 Three separate measurements of axial length are recorded, whereas a single shot automatically recorded five measures of the anterior chamber depth. The posterior segment depth was calculated by subtracting the anterior chanber depth from the axial length obtained with the IOL Master. All biometric measurements were undertaken prior to cycloplegia.
Corneal StainingThe extent and depth of corneal staining were measured to the nearest 0.5 unit using the CCLRU grading scales.22 Additionally, the location (i.e. superior, inferior, nasal, temporal and central) of the staining was also recorded.
Subjective QuestionnairesThe Pediatric Refractive Error Profile survey, employed by Walline et al., will be employed to assess and compare vision-specific quality of life of those children in the OK and the SV groups, both at the 12- and the 24-month follow-up visits.25,26 The survey was modified for both the OK and the SV groups and consists of 26 questions to which was added two additional questions:
- 27.
The habitual handling of my contact lenses/glasses is normally done by my parents.
- 28.
I usually perform the handling of my contact lenses/glasses.
All the questions have a stem of five possible responses: strongly disagree, disagree, neutral, agree and strongly agree. The surveys will be answered by the children, and parents will be asked not to participate.
The same format was used for two further questions to be answered only by the parents:
- 1.
I think orthokeratology contact lenses/glasses are an excellent method of visual correction.
- 2.
Once this study is finished, I intend to continue offering this method of visual correction to my child.
The number of contact lenses required to achieve an optimum fit during the initial contact lens fitting procedure was recorded, together with the reasons for the implemented changes (i.e. flat fit). At the follow-up visits, the number of lenses required throughout the study and the reasons for each change (i.e., lost and broken lenses, or change in refraction) are also recorded.
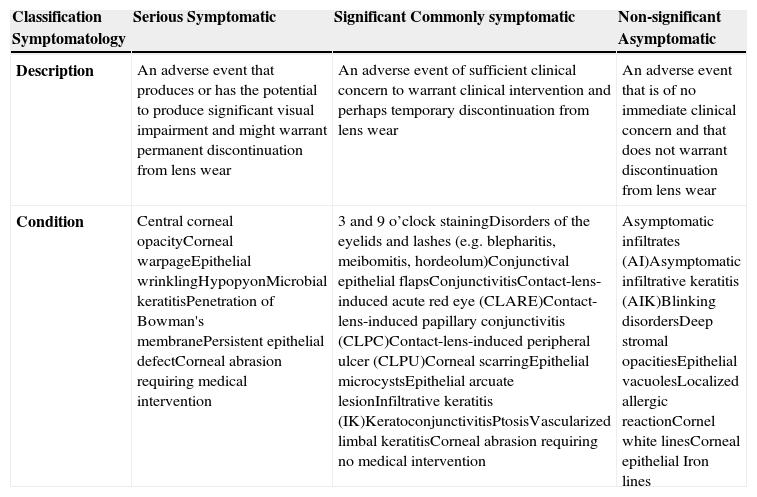
Adverse Events and DiscontinuationsThe classification of adverse events and discontinuations were adapted from Morgan et al.27 Adverse events were classified as “serious,” “significant,” or “non-significant” according to table 3.27,28 Although table 3 shows most of the ocular adverse events that could occur as a result of contact lens and spectacle wear, all adverse events, even those not shown in table 3, were recorded in this study. For obscure adverse reactions, the opinion of the ophthalmologist on duty at the clinic is sought and the condition treated in collaboration with the MCOS clinician. In all cases, an appropriate classification of the adverse reaction is obtained. Recurrences of the same adverse event(s) in the same or fellow eye at any of the subsequent follow-up visits were classified as separate events; bilateral events were counted as two separate events. The incidence rate of each adverse event was recorded as a percentage of eyes per annum.29
Classification of adverse events. The table has been adapted from Morgan et al.28
| Classification Symptomatology | Serious Symptomatic | Significant Commonly symptomatic | Non-significant Asymptomatic |
| Description | An adverse event that produces or has the potential to produce significant visual impairment and might warrant permanent discontinuation from lens wear | An adverse event of sufficient clinical concern to warrant clinical intervention and perhaps temporary discontinuation from lens wear | An adverse event that is of no immediate clinical concern and that does not warrant discontinuation from lens wear |
| Condition | Central corneal opacityCorneal warpageEpithelial wrinklingHypopyonMicrobial keratitisPenetration of Bowman's membranePersistent epithelial defectCorneal abrasion requiring medical intervention | 3 and 9 o’clock stainingDisorders of the eyelids and lashes (e.g. blepharitis, meibomitis, hordeolum)Conjunctival epithelial flapsConjunctivitisContact-lens-induced acute red eye (CLARE)Contact-lens-induced papillary conjunctivitis (CLPC)Contact-lens-induced peripheral ulcer (CLPU)Corneal scarringEpithelial microcystsEpithelial arcuate lesionInfiltrative keratitis (IK)KeratoconjunctivitisPtosisVascularized limbal keratitisCorneal abrasion requiring no medical intervention | Asymptomatic infiltrates (AI)Asymptomatic infiltrative keratitis (AIK)Blinking disordersDeep stromal opacitiesEpithelial vacuolesLocalized allergic reactionCornel white linesCorneal epithelial Iron lines |
In this study, “discontinuation” is defined as the cessation of lens wear for the remainder of the study. Discontinuation may occur as a result of: adverse events, ocular discomfort, visual problems, lack of motivation, failure to follow up instructions, unacceptable visual acuity and other logistic or personal reasons that may or may not have been directly related to lens wear. Temporary suspension of lens wear of up to 2 weeks was allowed (at the investigator's discretion) should significant symptoms or slit-lamp findings occur. Although temporarily discontinued, subjects were examined at frequent intervals until the condition completely subsided, and attempts were made to limit the duration of the suspension period to as few days as possible. Some subjects were discontinued from the study as a result of “lost to follow up”; defined as a situation whereby a subject did not turn up at the next scheduled follow-up visit (despite active efforts to encourage attendance). The incidence rate of discontinuations was recorded as a percentage of subjects per annum.29
Data Collection and MaskingInvestigator CV-C was responsible for the data collection; investigator JS-R undertook all the data analysis without knowing the identity of the study groups.
Statistical AnalysisThe goodness-of-fit Kolomogorov-Smirnov test was employed to assess whether or not baseline demographics, refractive and biometric data from both groups were significantly different from one another, hypothesized on the basis of the assumption of a normal distribution. Normally and non-normally distributed data were expressed as mean ± standard deviation (SD) and median [quartiles], respectively. The differences between the two study groups in terms of baseline demographics, refractive and biometric data were analyzed using unpaired t-tests and Mann-Whitney U tests, depending on whether the results of the Kolomogorov-Smirnov test demonstrated that the data were normally distributed or not normally distributed, respectively. Data for the right eye was only used to avoid the confounding effect of using non-independent data from both eyes.30 The level of statistical significance was taken as 5%.
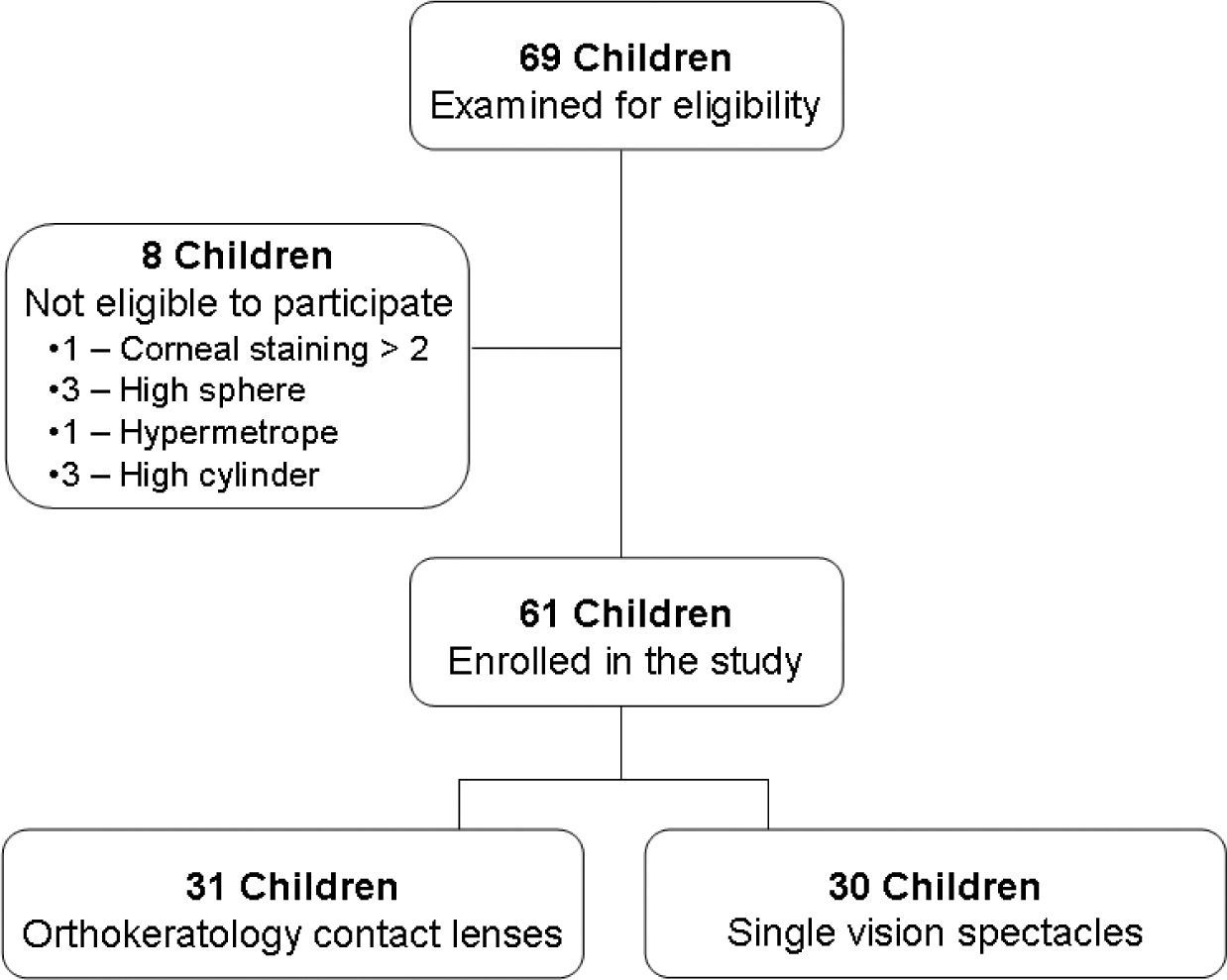
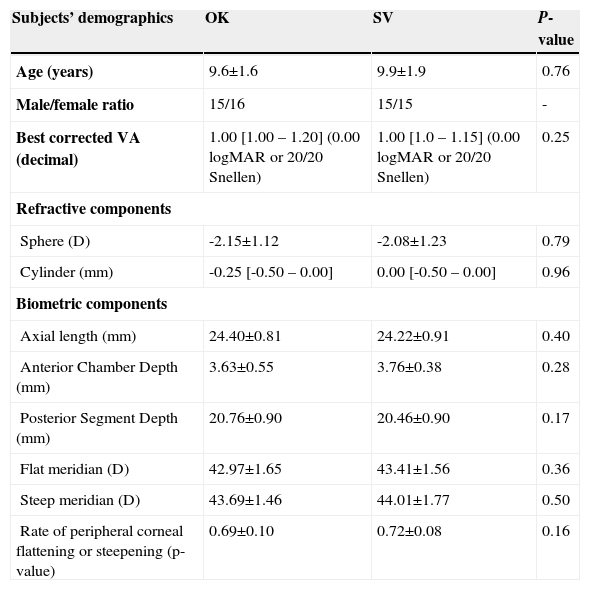
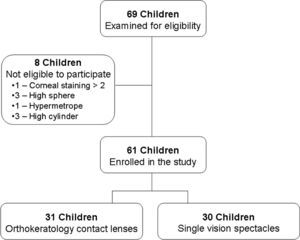
ResultsSixty-nine subjects were recruited for the study between March 2007 and March 2008. Thirty-one children were prospectively allocated to OK and 30 to the SV correction modalities (Figure 2). Eight subjects could not be enrolled in the study because they failed to meet the inclusion criterion for refraction (Figure 2). A normal frequency distribution was found for all baseline demographics, refractive and biometric data in both groups (P>0.05), except for visual acuity and the cylindrical refractive component (P<0.01). Thus, parametric and non-parametric statistics were employed accordingly to assess differences between groups at baseline. Both study groups were well matched at baseline as no significant differences were found between the two groups neither in demographics, nor in refractive nor in biometric data (Table 4).
Baseline subjects’ demographics, and refractive and biometric data. Normally and non-normally distributed data were expressed as mean ± standard deviation (SD) and median [quartiles], respectively. “P-value” refers to the statistical P-value; “p-value (units)” refers to the rate of peripheral corneal flattening or steepening
| Subjects’ demographics | OK | SV | P-value |
| Age (years) | 9.6±1.6 | 9.9±1.9 | 0.76 |
| Male/female ratio | 15/16 | 15/15 | - |
| Best corrected VA (decimal) | 1.00 [1.00 – 1.20] (0.00 logMAR or 20/20 Snellen) | 1.00 [1.0 – 1.15] (0.00 logMAR or 20/20 Snellen) | 0.25 |
| Refractive components | |||
| Sphere (D) | -2.15±1.12 | -2.08±1.23 | 0.79 |
| Cylinder (mm) | -0.25 [-0.50 – 0.00] | 0.00 [-0.50 – 0.00] | 0.96 |
| Biometric components | |||
| Axial length (mm) | 24.40±0.81 | 24.22±0.91 | 0.40 |
| Anterior Chamber Depth (mm) | 3.63±0.55 | 3.76±0.38 | 0.28 |
| Posterior Segment Depth (mm) | 20.76±0.90 | 20.46±0.90 | 0.17 |
| Flat meridian (D) | 42.97±1.65 | 43.41±1.56 | 0.36 |
| Steep meridian (D) | 43.69±1.46 | 44.01±1.77 | 0.50 |
| Rate of peripheral corneal flattening or steepening (p-value) | 0.69±0.10 | 0.72±0.08 | 0.16 |
OK: Orthokeratology; SV: single-vision spectacles; VA: visual acuity; D: diopters.
Of the 31 subjects that were assigned orthokeratology contact lens wear at baseline, an optimum lens fit was obtained in 21 subjects with the first contact lens fitted in accordance with the Menicon Professional Easy Fit software. Ten subjects required a total of 35 adjustments to attain an optimum lens fit. Of these, 5 subjects required more than 2 contact lens fit changes per eye; 5 subjects required just 1 change each; 2 subjects required 1 change per eye each; 2 subjects required 2 changes per eye each; and 3 subjects required 3 changes each. The reasons for the changes were: undercorrection (13), lens decentration (12) and central island (10). Across the whole group, an average of 1.6 lenses per eye were required to attain an optimum fit. Two subjects broke their lenses (2) and one subject lost one lens in the interim between initial contact lens fitting and final enrolment in the study (Figure 1).
None of the subjects showed corneal staining and no adverse events were found in any of the two groups at baseline.
DiscussionTo the authors’ knowledge, the MCOS study is the first prospective clinical trial to assess the efficacy and safety of OK lens wear for myopia progression vs. a group of SV spectacle lens wearers. Subjects and parents engaged enthusiastically in the study and responded well to initial introduction of the study design and protocol. The number of contact lenses required to achieve an optimum fit were either lower than31 or similar to32 those reported in previous studies.
For the present study (MCOS), the subjects’ baseline refractive and biometric data were markedly similar to those from other studies assessing the effects of orthokeratology contact lens wear on myopia progression in children.15,16 Also, similar age groups and male/female ratios were employed in MCOS compared to a previous study;15 another study employed an older group and a higher percentage of female subjects.16
Although we are fully aware of the advantages of random allocation, to our knowledge no previous study on the effects of orthokeratology contact lens wear on myopia progression has used a randomized design. Subjects were not randomized into the two modalities of visual correction in MCOS, but both study groups were well matched, as shown by the similarity between the baseline demographics, refractive and biometric data collected in the two groups. Also, all subjects from both study groups in MCOS were monitored over the same time period. Previous studies have used historical prospective control groups that had not been monitored over the same time period; the latter feature might introduce a higher bias than that due to MCOS's design (e.g. it is possible that children from the historical control groups were monitored during times of different environmental exposure, such as greater levels of close work, compared to the experimental groups). Furthermore, the advantage of MCOS's approach is that it is apposite to actual clinical practice, where practitioners provide various options of visual correction and parents opt for a particular option with the child's approval.
A limitation of this study is that, in terms of statistical power, the sample size employed is theoretically too small to detect the absolute incidence rates of adverse events and discontinuations for each of the two modalities of visual correction under investigation. However, we envisage that it might be sufficiently powered to detect differences in incidence rate between the two groups, as previous studies with samples sizes similar to those used in the present study have effectively demonstrated differences in incidence rate for different contact lens types and wearing regimes.27,29
The primary outcome measure of this study is, however, to compare in white European myopic children axial length growth following OK and SV lens wear over a 2-year period. In this respect, the comparison of axial growth between the two groups is optimized by the use of non-contact partial coherence interferometry, which has a resolution that is an order of magnitude better than that of the 10 Hz ultrasound technique.18
Since the start of the MCOS, the importance of peripheral imagery in the etiology of myopia has been acknowledged both in animal and in human studies.33-35 Consequently, as an adjunct to the present study, peripheral axial length measures in the horizontal plane (using partial coherence interferometry) will be recorded at the 24-month follow-up visit for both study groups, at successive eccentricities at successive eccentricities from from 10° to 30° temporally and nasally.36
Another constraint of the MCOS study is that the investigator collecting clinical data (CV-C) was not masked with respect to the mode of visual correction. Full masking of data collection in clinical trials such as MCOS presents difficulties, in that the identity of the subject's group can be revealed by a variety of clinical observations such as, for example, limbal or conjunctival staining or corneal topography measurements. Nevertheless, the investigator collecting data was fully aware of the need to disregard where feasible the identity of the subject's group. Furthermore, data analysis was undertaken by an investigator (JS-R) who was masked with regard to the identity of the study groups.
Although some limitations in the MCOS study have been identified, the study offers a number of notable features: a prospective design; well-matched samples and high-resolution ocular biometry measures, which collectively should elucidate whether or not OK contact lens wear is a feasible and safe method for myopia progression control.
The authors acknowledge the clinical and technical staff at Novovision for their assistance with the acquisition of the data for this study, EURO-OPTICA for their help in recruiting subjects for the study and Dr Edward Mallen of the University of Bradford, United Kingdom, for his help in developing the IOLMaster attachment needed to undertake peripheral axial-length measurements. This work was partly funded by Menicon Co., Ltd.