To compare contrast sensitivity (CS) in multi-transfused β-thalassemia patients who received deferoxamine with those who received Osveral.
MethodsIn this cross sectional study a total of 60 β-thalassemia patients (30 used deferoxamine and 30 used deferasirox) were regarded as case group and 30 age and sex matched healthy subjects were selected as control group. All subjects had a set of examinations including refraction, visual acuity, Biomicroscopy, ophthalmoscopy and CS. Contrast threshold was assessed with the use of Freiberg visual acuity and contrast test under the mesopic light condition for three frequencies; 1, 5, 15cpd. All data analysis was performed using SPSS, version 17.
ResultsIn visual acuity tests, thalassemic patients did not have any problem. Contrast threshold was higher in thalassemic patients who infuse deferoxamine (1.87±0.63, 1.46±0.81, and 2.96±1.68 in 1, 5, and 15cpd, respectively) than that of those who intake deferasirox (1.74±0.80 (P=0.743), 0.99±0.74 (P=0.047), and 2.42±1.36 (P=0.321) for 1, 5, and 15cpd, respectively), and also than healthy patients (1.33±0.58 (P=0.009), 0.95±0.68 (P=0.022), and 2.24±1.23 (P=0.135) for 1, 5, and 15cpd, respectively). Comparing those who used deferasirox with healthy subjects, contrast threshold was higher in deferasirox group at all special frequencies (P>0.05). No significant relationship was observed between CS values and duration of transfusion, serum ferritin concentration and dose of chelation therapy (P>0.05).
ConclusionsCS tests can detect visual disturbance in thalassemic patients before the impairment of visual acuity. It is suggested that CS tests be included in their regular eye examination.
Comparar la sensibilidad de contraste (SC) en pacientes multitrasfundidos con β-talasemia y tratados con deferoxamina u Osveral.
MétodosEn este estudio transversal, un total de 60 pacientes con β-talasemia (30 tratados con deferoxamina y 30 con deferasirox) fueron considerados como grupo de estudio, y 30 sujetos sanos pareados por edad y sexo fueron seleccionados como grupo control. A todos los sujetos se les realizó una serie de exámenes que incluyeron refracción, agudeza visual, biomicroscopía, oftalmoscopía y SC. El umbral de contraste se valoró mediante la prueba de agudeza visual y contraste de Freiberg, en condiciones de visión mesópica para tres frecuencias: 1, 5 y 15 cpd. Todos los análisis de los datos se realizaron utilizando SPSS, versión 17.
ResultadosEn las pruebas de agudeza visual los pacientes con talasemia no tuvieron ningún problema. El umbral de contraste fue superior en los pacientes con talasemia a quienes se infundió deferoxamina (1,87±0,63, 1,46±0,81 y 2,96±1,68 en 1, 5 y 15 cpd, respectivamente) que en los pacientes tratados con deferasirox (1,74±0,8 (P=0,743), 0,99±0,74 (P=0,047) y 2,42±1,36 (P=0,321) para 1, 5 y 15 cpd, respectivamente), y también en los pacientes sanos (1,33±0,58 (P=0,009), 0,95±0,68 (P=0,022) y 2,24±1,23 (P=0,135) para 1, 5 y 15 cpd, respectivamente). Al comparar los pacientes tratados con deferasirox y los sujetos sanos, el umbral de contraste fue superior en el grupo de deferasirox para todas las frecuencias especiales (P>0,05). No se observó una relación significativa entre los valores de SC y la duración de la trasfusión, la concentración de ferritina sérica y la dosis de la terapia de quelación (P>0,05).
ConclusionesLas pruebas de SC pueden detectar la alteración visual en los pacientes con talasemia con anterioridad al deterioro de la agudeza visual. Sugerimos la inclusión de las pruebas de SC en su examen ocular regular.
Thalassemia which is one of the most common sever genetic blood disorders can lead to different ocular involvements.1,2 Ocular findings in these patients may correlate to disease itself, iron overload due to regular blood transfusion or chelating agents used to reduce iron store in their body.3
Since 1970, iron chelation therapy has been used to reduce iron overload in thalassemic patients.4 Deferoxamine (DFO, Desferal®) is the oldest iron chelator which should be injected subcutaneously usually in the duration of 8–12h. Injection of DFO is its main problem. So in recent years some oral chelators such as deferiprone and deferasirox were introduced.5,6
Ocular complications of thalassemia and its therapeutic modalities has been reported by many sources.1,3,7,8 But there are only few studies that evaluate contrast sensitivity in these patients.9–11 Impaired contrast sensitivity in the presence of normal visual acuity can detect early changes in the visual system of these patients. To our knowledge, no study has been done to compare contrast sensitivity in thalassemia major patients who used different chelator agents.
Gartaganis et al. in 2000 investigated contrast sensitivity function in β-thalassemia major patients treated by regular blood transfusion and subcutaneous infusion of DFO. They used the Vector Vision CSV-1000 contrast sensitivity test and conclude that contrast sensitivity function in all β-thalassemia patients was significantly lower than normal subjects.10 Spyridon et al. in 2010 used B-VAT II SG mentor visual acuity tester to measure contrast sensitivity in β-thalassemia major patients and found significant difference between contrast sensitivity of thalassemic and normal subjects in special frequencies of 2, 3, and 6 cycles per degree (cpd).11
According to high prevalence of β-thalassemia in Iranian population, particularly in north of Iran12 and its ocular side effects which influence their quality of life, evaluation of contrast sensitivity of these patients using cheap, simple and reliable test to identify early changes in their ocular system is fundamental.
The primary objective of this study was to compare contrast sensitivity in multi-transfused β-thalassemia patients who received subcutaneous DFO with those who received Osveral (an Iranian made deferasirox) and normal subjects. We also investigated the correlation of contrast sensitivity with serum ferritin level, duration of blood transfusion and dosage of chelation therapy.
MethodsThis cross sectional study was carried out in the thalassemic research center of Mazandaran province, Iran. Thalassemic patients in Mazandaran are all registered in this center in order to receive treatment. Study participants were selected with simple random sampling method from the list of thalassemic patients with the use of computerized table. Informed written consent was obtained from all participants after a detailed explanation of the nature of the study according to the code of ethics in the declaration of Helsinki protocol. Selected participants were visited by hematologist and those with no diabetes or other systemic disease who received chelator agents (DFO or deferasirox) for at least 2 years were referred for ophthalmic and optometric evaluation.
An ophthalmologist examined anterior and posterior segments of the eye with the use of slit lamp (Model BQ 900: Haag Streit, Bern, Switzerland) and ophthalmoscope (Ophthalmoscope, Heine Beta 200, Germany) and those with any ophthalmic pathology, aphakia, strabismus, corneal and lens opacities, history of ocular surgery, history of ocular trauma and pathologic myopia were excluded.
Then an optometrist began optometric examinations. Uncorrected visual acuity (UCVA) was measured monocularly using the Snellen chart at 6m. Refraction was measured using the autorefractometer (Topcon RM8800) and checked with a Heine streak retinoscope (HEINE Optotechnik). Those with UCVA worse than 20/20 had subjective refraction and then best corrected visual acuity (BCVA) was recorded. Those with BCVA worse than 20/20 and those with spherical refractive error of more than 1.5 diopter (D) and astigmatism greater than 1D were excluded from the study.
Finally, 60 patients with β-thalassemia (30 used DFO and 30 used deferasirox) ranging in age between 20 to 30 years and 30 age and sex matched healthy subjects were enrolled for the study. Healthy subjects were selected randomly amongst the staff of the thalassemia research center. Contrast sensitivity test was done for all selected subjects. Contrast threshold was measured for each eye with the Freiberg visual acuity and contrast test (FrACT version 3.7.1) under mesopic light condition for three frequencies; 1, 5, 15cpd.
FrACT is a computer program that uses eight alternative force choices and the best parameter estimation by sequential testing (PEST) algorithm for threshold determination.13,14 It enables automatic and observe independent determination of contrast threshold at different special frequencies using sinusoidal gratings or special optotype size. In this study, gratings were presented in 8 different orientations. The patient tell the perceived direction of gratings and the investigator entered the response. Twenty-four trials comprised one run and two runs were taken for each condition. At the end of the test, contrast threshold was computed in percent and showed on the screen.
Contrast threshold was tested monocularly at a distance of 4m. In those with UCVA worse than 20/20, contrast sensitivity evaluation was performed using carefully cleansed trial lenses (Oculus, Wetzler, Germany).
Descriptive and inferential data analysis were carried out using SPSS.17 software (SPSS for Windows, SPSS Inc., Chicago, IL, USA). Kolmogorov–Smirnov test for normality indicated that the distribution of spherical and cylindrical refractive errors was not normal and therefore non-parametric tests were used for statistical analysis of these parameters. Median test, independent sample T Test, One-way ANOVA and Pearson correlation were used where applicable. A statistical significant difference was considered for P<0.05.
ResultsIn this study, 60 thalassemic patients were studied including thirty patients from desferal group and 30 from Osveral group. As contrast thresholds in the right and left eye were correlated (Pearson correlation; r=0.847, P=0.000), the data from the right eye were considered. The mean age of thalassemic patients in Desferal and Osveral groups were 24.33±3.44 and 23.70±3.39, respectively. The control group included 30 healthy subjects with the mean age of 24.70±3.46. The age of included subjects in case and control groups ranged from 20 to 30 years old. There was no significant difference for sex and age between groups (P=0.731, P=0.524, respectively).
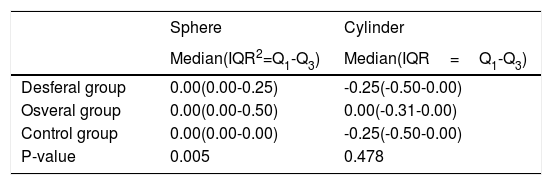
Table 1 shows median and interquartile range (IQR) of spherical and cylindrical refractive errors in the two thalassemic and control groups. Median test was used for testing whether study groups differ in their median value or not. According to the table, significant difference was found between spherical refractive errors of three groups (P=0.005), but no significant difference was found in cylindrical refractive errors (P=0.478).
Spherical and cylindrical refractive errors in two thalassemic and control groups.1
| Sphere | Cylinder | |
|---|---|---|
| Median(IQR2=Q1-Q3) | Median(IQR=Q1-Q3) | |
| Desferal group | 0.00(0.00-0.25) | -0.25(-0.50-0.00) |
| Osveral group | 0.00(0.00-0.50) | 0.00(-0.31-0.00) |
| Control group | 0.00(0.00-0.00) | -0.25(-0.50-0.00) |
| P-value | 0.005 | 0.478 |
All thalassemic patients were asymptomatic and ophthalmic examinations did not revealed any pathological and structural problem in their ocular system. The mean ±SD values for best corrected visual acuity was 1min of arc in all participants.
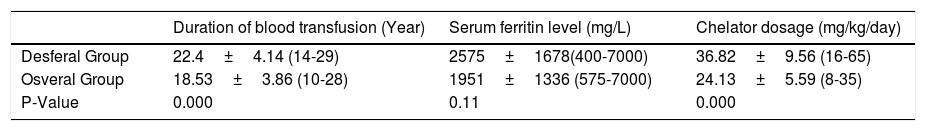
Table 2 shows the characteristics of thalassemic patients based on the type of chelator they received.
characteristics of thalassemic patients based on the type of chelator they received1
| Duration of blood transfusion (Year) | Serum ferritin level (mg/L) | Chelator dosage (mg/kg/day) | |
|---|---|---|---|
| Desferal Group | 22.4±4.14 (14-29) | 2575±1678(400-7000) | 36.82±9.56 (16-65) |
| Osveral Group | 18.53±3.86 (10-28) | 1951±1336 (575-7000) | 24.13±5.59 (8-35) |
| P-Value | 0.000 | 0.11 | 0.000 |
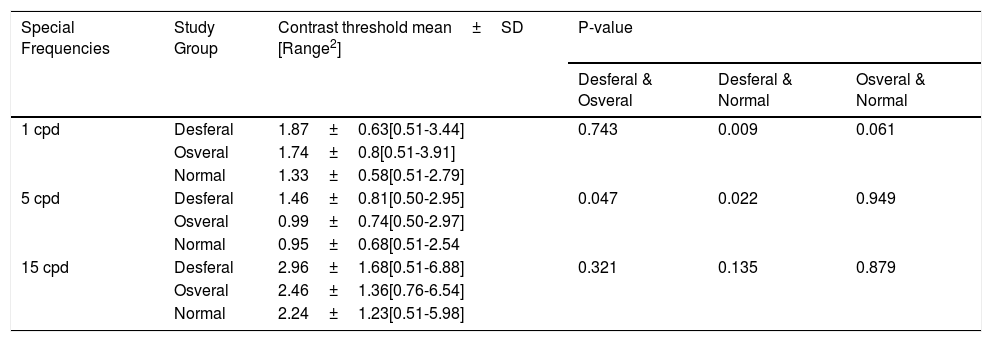
The mean±SD contrast threshold of all participants are given in Table 3. Contrast threshold was evaluated for three spatial frequencies (1, 5, and 15cpd). One-way ANOVA test showed a significant difference between contrast threshold of patients in Desferal and control groups in all evaluated special frequencies. Also, contrast threshold of Desferal group for all special frequencies was higher than that of Osveral group, although the difference was not statistically significant for 1 and 15cpd. In the comparison of contrast threshold in those who used deferasirox with healthy subjects, contrast threshold was higher in deferasirox group at all special frequencies, but the difference was not significant.
Mean contrast threshold of both thalassemic and healthy subjects.1
| Special Frequencies | Study Group | Contrast threshold mean±SD [Range2] | P-value | ||
|---|---|---|---|---|---|
| Desferal & Osveral | Desferal & Normal | Osveral & Normal | |||
| 1 cpd | Desferal | 1.87±0.63[0.51-3.44] | 0.743 | 0.009 | 0.061 |
| Osveral | 1.74±0.8[0.51-3.91] | ||||
| Normal | 1.33±0.58[0.51-2.79] | ||||
| 5 cpd | Desferal | 1.46±0.81[0.50-2.95] | 0.047 | 0.022 | 0.949 |
| Osveral | 0.99±0.74[0.50-2.97] | ||||
| Normal | 0.95±0.68[0.51-2.54 | ||||
| 15 cpd | Desferal | 2.96±1.68[0.51-6.88] | 0.321 | 0.135 | 0.879 |
| Osveral | 2.46±1.36[0.76-6.54] | ||||
| Normal | 2.24±1.23[0.51-5.98] | ||||
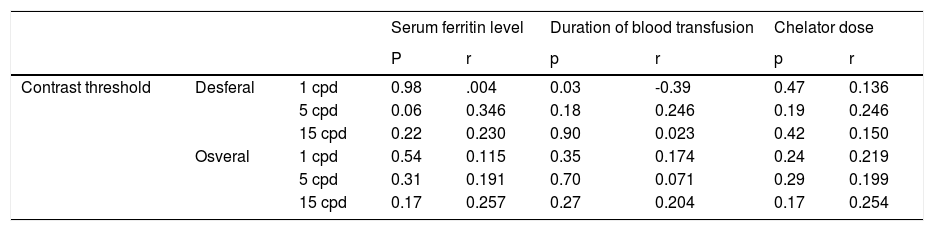
Table 4 represents the Pearson correlation of contrast threshold with serum ferritin level, dose of chelation therapy and duration of blood transfusion. According to the table, no significant correlation was found between contrast threshold and these parameters.
The Correlation of contrast threshold with serum ferritin level, dose of chelation therapy and duration of blood transfusion.1
| Serum ferritin level | Duration of blood transfusion | Chelator dose | ||||||
|---|---|---|---|---|---|---|---|---|
| P | r | p | r | p | r | |||
| Contrast threshold | Desferal | 1 cpd | 0.98 | .004 | 0.03 | -0.39 | 0.47 | 0.136 |
| 5 cpd | 0.06 | 0.346 | 0.18 | 0.246 | 0.19 | 0.246 | ||
| 15 cpd | 0.22 | 0.230 | 0.90 | 0.023 | 0.42 | 0.150 | ||
| Osveral | 1 cpd | 0.54 | 0.115 | 0.35 | 0.174 | 0.24 | 0.219 | |
| 5 cpd | 0.31 | 0.191 | 0.70 | 0.071 | 0.29 | 0.199 | ||
| 15 cpd | 0.17 | 0.257 | 0.27 | 0.204 | 0.17 | 0.254 | ||
Contrast sensitivity has been considered as an important indicator of visual function by some researchers and it is claimed that its evaluation can better discriminate ophthalmic disorders compared to Snellen visual acuity.15,16 As the results of this study showed, contrast threshold was higher in patients with major thalassemia who infuse DFO than that of those who intake deferasirox and also healthy patients at all spatial frequencies. In the comparison of contrast threshold in those who used deferasirox with healthy subjects, contrast threshold was higher in deferasirox group at all special frequencies, but the difference was not significant. While in conventional visual acuity tests measured with the Snellen chart, thalassemic patients did not have any problem. No statistically significant relationship was observed between contrast sensitivity values and duration of transfusion, mean serum ferritin concentration and dose of chelation therapy.
Previous studies have also confirmed similar findings; Gartaganis et al. have found that contrast sensitivity function in all beta-thalassemic patients with normal Snellen visual acuity was significantly lower compared to the normal control subjects for all spatial frequencies tested.10 Spyridon et al. also reported reduced contrast sensitivity values in patients with major thalassemia than the values for normal subjects for frequencies of 2, 3 and 6cpd.11
Ocular complications, such as lens opacity, macular degeneration, retinal vascular changes and RPE degeneration have been reported in patients with major thalassemia in previous studies.1,3,7,8,17 The mechanism is not exactly clear, some researchers believe that ocular abnormalities were mainly because of iron overload and not secondary to chelation therapy while others claim that chelator administration, especially DFO, has toxic effects and can affect the eye in many ways.3 Also, unstable blood hemoglobin values in spite of periodic blood transfusion can cause chronic retinal hypoxia and damage function of the retinal cells.10
In the current study, we did not include those with any pathologic eye problems or systemic diseases, such as diabetes which can adversely affect visual system. It is claimed that in diabetic patients due to disruption of the blood retinal barrier, DFO is able to cross to retina more than in normal patients and consequently can cause more toxic problems.18,19 On the other hand, we exclude thalassemic patients with high refractive errors, especially high myopia. It seems that in these patients due to changes in Bruch layer, iron deposition would be higher and subsequently more side effect is expected.20 It should be noted that, similar to previous studies, despite the lack of obvious pathological and structural changes in the ocular system of our selected thalassemic patients, their contrast sensitivity was considerably lower than in healthy subjects, especially in those who infuse DFO. However, although we do not find any obvious ocular pathology in our selected patients, previous studies indicated that they may reveal some abnormalities with the use of electro-diagnostic tests, fluorescein angiography or tests such as perimetery.1,3,21 For instance, Gartaganis et al. did not found any problem in slit lamp examination of their patients but angiod streak and RPE degeneration were revealed in 13% of their subjects with the use of fluorescein angiography. They also reported that contrast sensitivity loss in those who revealed ocular pathology with the use of fluorescein angiography was higher than that of those who do not showed any problem.10
The result of our study showed a significant difference between contrast sensitivity of thalassemic patients who used different chelator drugs. To our knowledge, this is the first study that compare contrast sensitivity in thalassemic patients using different chelator agents. In a previous study, we evaluate ocular abnormalities in thalassemic patients who used different chelator drugs. In that study, in order to evaluate the effect of different type of chelators, thalassemia patients were divided into three groups based on the type of chelators they received: Group A received blood transfusion and subcutaneous DFO, Group B blood transfusion combined with subcutaneous DFO and oral deferiprone, and Group C blood transfusion along with Osveral. Although no significant difference was found between the prevalence of different type of ocular abnormalities among three thalassemic groups in that study, among evaluated ocular abnormalities, RPE degeneration was slightly higher in those who used desferal in comparison to those who used Osveral.1 In our present study, contrast sensitivity in desferal group was considerably lower than that of Osveral group. More reduction of contrast sensitivity in those who used desferal confirm that they may reveal some abnormalities in more detailed examinations.
There are several studies that investigate the relationship between the dose of chelator agents, mean serum ferritin level and the number of blood transfusions with ocular problems.1,8,10,22 In this study, we did not observe any relationship between duration of blood transfusion, chelator dose and serum ferritin level with contrast sensitivity, which was similar to Gartaganis findings. They conclude that the main reason for contrast sensitivity loss could be chronic retinal hypoxia and other factors such as duration of transfusions, the duration of chelator therapy and the serum ferritin concentrations are of lesser importance.10 In our previous study on another group of thalassemic patients, we found a significant positive correlation between the prevalence of ocular abnormalities and number of blood transfusions but not with mean serum ferritin level and dose of chelator agents.1 However, considering different age range of the participants in different studies, it is difficult to make an accurate comparison.
However, despite widespread claims of the effectiveness of DFO dosage on visual function,22 we do not find any correlation between doses of chelator agents and contrast sensitivity reduction. This could be due to low dose of chelator that our patients received. Cohen et al. indicated that DFO doses lower than 50mg/kg/day cannot cause structural eye problems and only may lead to hearing loss.23 Ninety eight percent of our subjects received lower than 50mg/kg/day of chelators.
Our study has some limitations; in this study those who were taking Osveral were on DFO previously, so loss of contrast sensitivity can be related to their previous treatment. Also, due to the limited number of cases and the short time that they intake Osveral, we could not fully evaluate effect of Osveral on contrast sensitivity function of these patients. Also, we do not evaluate and exclude patients with dry eye. As there is evidence about the degree of association between thalassemia and dry eye,1 which could have some effects on contrast sensitivity results, it was better to exclude those with dry eye.
As we know, in many ophthalmic disorders contrast sensitivity tests can detect visual disturbances before the impairment of visual acuity. According to this issue, it is suggested that contrast sensitivity tests be included in regular eye examination of thalassemic patients and in the event of diagnosis any reduction in contrast sensitivity, it is better to refer patients to hematologist to evaluate the possibility of changing their treatment regimen and prevent further complications.
Conflicts of interestThe authors report no conflicts of interest. The authors alone are responsible for the content and writing of the paper. Also, this research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
The authors wish to thank the staff and patients of the thalassemia research center and Bou-Ali Sina Hospital of Mazandaran University of medical sciences for their cooperation.