Goldmann applanation tonometer (GAT) is the gold standard for Intraocular Pressure (IOP) measurement but has disadvantage of being contact device and problems with portability. The aim of the study was to compare the Keeler's Pulsair noncontact tonometer (NCT) with GAT in Indian Population.
Materials and methodsEighty-one subjects were screened from a Glaucoma clinic of a tertiary care centre in North India. The IOP was measured by Pulsair NCT and GAT after explaining the procedure. Central corneal thickness (CCT) was measured to avoid its bias on IOP readings. The data were analyzed using SPSS software.
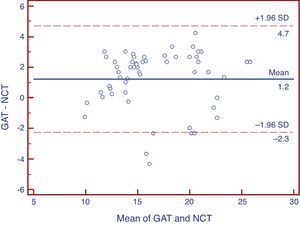
ResultsThe mean age of subjects was 49.9±8.8 (mean±SD) years. The mean IOP as taken by Pulsair NCT was 15.79±4.07mmHg and that for GAT was 17.02±4.23mmHg (p=0.062). The mean CCT was 0.536±0.019mm. A positive Pearson's correlation coefficient of 0.909 (p=0.0001) was found between the two instruments. Bland and Altmann analysis showed a fair agreement between the two tonometers at lower IOP range.
ConclusionPulsair NCT can be used as a screening tool for community practices but is not reliable in the subjects with higher IOP range.
El Tonómetro de aplanación de Goldmann (TAG) es el método de referencia para la medición de la presión intraocular (PIO), aunque tiene la desventaja de que es un dispositivo de contacto, y presenta problemas de portabilidad. El objetivo de este estudio fue la comparación del tonómetro de no contacto Pulsair de Keeler (NCT) con el TAG en la población de India.
Material y métodosSe exploró a ochenta y un pacientes en una clínica de glaucoma, perteneciente a un centro de atención terciaria al norte de India. Se midió la PIO utilizando el NCT y el TAG, tras la explicación del procedimiento. Se midió el espesor central corneal (ECC) para evitar su influencia en las lecturas de la PIO. Se analizaron los datos utilizando el software SPSS.
ResultadosLa edad media de los pacientes fue de 49,9±8,8 (mediana±DE) años. La PIO media medida con Pulsair NCT fue de 15,79±4,07mm Hg, y la medida con GAT fue de 17,02±4,23mm Hg (p=0,062). El ECC medio fue de 0,536±0,019mm. Se halló un coeficiente de correlación de Pearson de 0,909 (p=0,0001) entre los dos dispositivos. El análisis de Bland y Altmann arrojó una concordancia clara entre los dos tonómetros en el rango de PIO mas baja.
ConclusiónEl Pulsair NCT puede utilizarse como herramienta de revisión en prácticas comunitarias, aunque no es fiable en pacientes PIO más elevadas.
Glaucoma is an optic neuropathy of multivariate aetiology wherein intraocular pressure (IOP) is the most important and only modifiable risk factor.1 The accurate IOP measurement has a very important role in diagnosis as well as management of glaucoma. However, Goldmann Applanation Tonometry (GAT) is still the gold standard for the measurement of IOP.2,3
Pulsair noncontact tonometer (NCT) is an air puff tonometer (Keeler Ltd., Windsor, Berks, UK) having basic working principle same as that of GAT.4,5
The Pulsair NCT has been compared with GAT by number of authors6–9 but none of them have compared these tonometers in Indian population. It is relevant to compare the two tonometers in Indian population because racial variations in IOP and CCT have been found in several studies.10–12 Liwan eye study highlighted that IOP is lower in Chinese population than in Caucasians.10 Similarly another study showed that African Americans have thinner CCT than Caucasians and Asians.11 Moreover, it is also well known that IOP readings are affected by CCT, corneal curvature and the technique used for its measurement.11,13 It has also been observed that NCT readings are affected more by thicker cornea than applanation readings.14 Due to these confounders it is important to test the two tonometers in Indian population.
In this study, we compared the IOP measurements by Pulsair NCT and GAT in normal and glaucomatous subjects of Indian subcontinent so that its applicability in this subset of population can be assessed.
Materials and methodsThis was a non-interventional, cross sectional study conducted at a tertiary care centre of Northern India. Eighty-one consecutive subjects attending the Glaucoma clinic were included in the study. IOP was measured by Keelers Pulsair NCT and a slit lamp mounted GAT in all the subjects. Thirty-seven out of 81 subjects were diagnosed as glaucoma and remaining 44 subjects had normal eye examination. The diagnosis of glaucoma was based on IOP, visual fields and disc evaluation. The normal subjects were taken as controls.
Inclusion criteria- (1)
Best corrected visual acuity (BCVA) at least 6/6
- (2)
Refractive error within ±2D spherical and within ±2D of astigmatism.15
- (3)
The subjects with normal fundus on +90D examination were included as controls.
- (4)
The subjects with glaucomatous visual field defects on Humphrey's visual fields and glaucomatous optic neuropathy who were diagnosed as Glaucoma.
- (1)
Refractive error >±2D.
- (2)
Any active eye disease – uveitis, corneal disease, infection, discharge, etc.
- (3)
Any condition that did not allow taking measurements.
Both the procedures were explained to the subjects and an informed consent was taken according to the Declaration of Helsinki.
All the measurements were taken from 9 AM to 10 AM to avoid the effect of diurnal fluctuations on IOP.
MethodsMeasurement by Pulsair NCT: this was done first in each patient followed by applanation tonometry. It was done before applanation tonometry because touching the cornea by applanation prism might have effect on NCT readings.16–22 The subjects were made to sit on a chair and IOP was measured by the hand held Pulsair NCT.
The measurements by the Pulsair NCT were taken four times, out of which first reading was excluded (as specified by the manufacturer). The average of three measurements was taken for analysis because it has been found that Pulsair NCT records first reading high followed by lower consecutive readings.5 The reading of only one eye was included in the study and the eye was decided by randomization from computer generated numbers to avoid dependency bias.
Measurement by GAT: the applanation tonometry was done by a slit lamp mounted applanation tonometer on Haag-Streit R-900 device (Haag-Streit, Koeniz, Switzerland). The subjects were seated comfortably on the slit lamp after explaining the procedure. Proparacaine (0.5%) eye drops were instilled as an anaesthetic agent followed by application of sterilized strip of Flourescein (1%) in the inferior fornix of the eye.2,3,23–25 The applanation prism tip was cleaned to avoid transmission of infection.26,27 The time difference of at least 15min was kept between the two measurements. The readings were taken by properly calibrated GAT. The standard clinical methods, recommendations and guidelines of the manufacturers were followed for appropriate readings.28–30 Three different readings for the designated eye were taken by a single experienced observer and the average was calculated which was used for statistical analysis.
Central Corneal Thickness (CCT) was measured by ultrasonic pachymeter (PacScan 300AP, Sonomed, NY, USA). It was done to adjust the IOP reading in patients with thick or thin cornea which has an effect on IOP measurements.6,10,11,13,31–33
The data were entered in Microsoft excel spread sheet. Statistical analysis was done with SPSS 16 software (Chicago, IL, USA). The mean IOP measured by each instruments were compared. Pearson's correlation coefficient was used to explore correlation between the two methods of IOP measurements. An agreement between the instruments was calculated by Bland and Altmann plots by Medcalc software (Mariakerke, Belgium). A p-value of <0.05 was taken as significant.
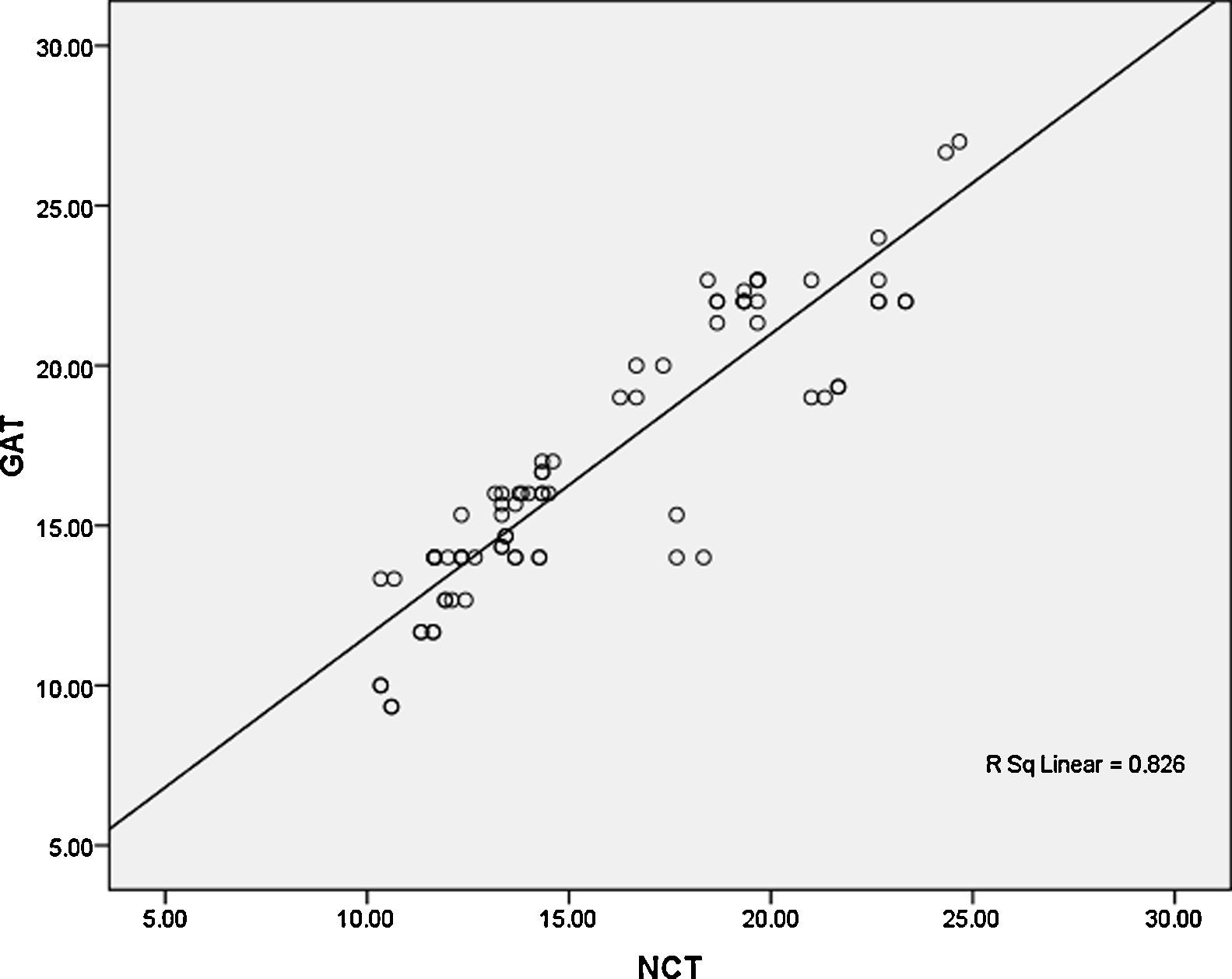
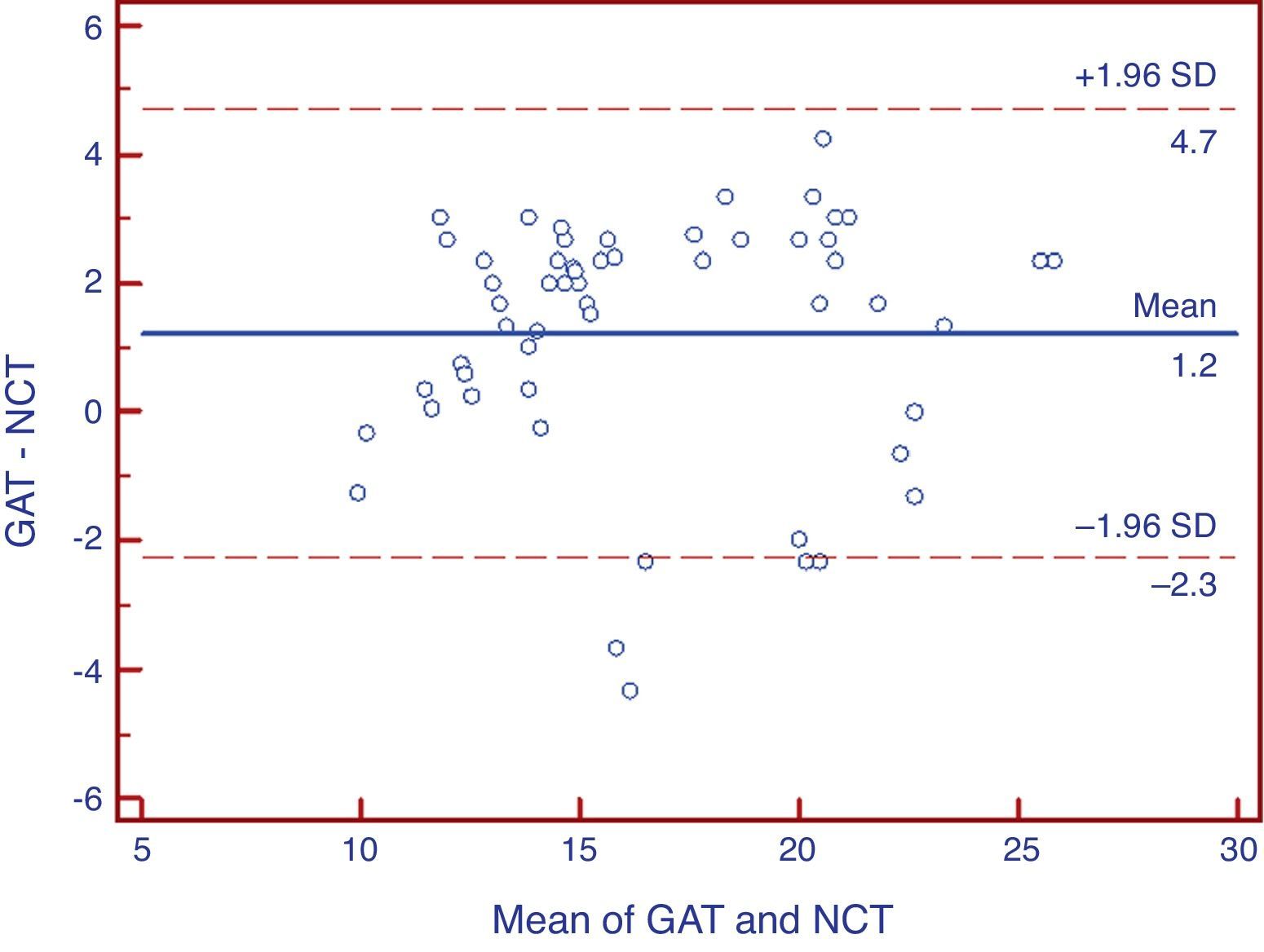
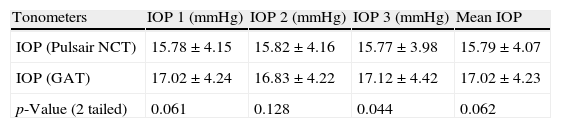
ResultsThe mean age of subjects was 49.9±8.84 (mean±standard deviation) years and the range was 40–78 years. The mean IOP, as taken by NCT, was 15.79±4.07mmHg (Table 1) and the range was 11.34–19.67mmHg. The mean IOP measurement by GAT was 17.02±4.23mmHg (Table 1) with a range of 13.33–21.27mmHg. The difference between the mean of the NCT and GAT reading was not found to be statistically significant (p=0.062). The mean CCT was 0.536±0.019mm with the range of 0.517–0.549mm. The bias calculated from the 95% CI was found to be 1.224. Twenty-nine (35.8%) out of eighty-one subjects had GAT IOP more than 18mmHg. The mean of difference between NCT and GAT in the subjects below 18mmHg was 0.99±1.66mmHg and in subjects with IOP >18mmHg was 1.71±1.88mmHg. Pearson's correlation coefficient was determined between the two tonometers and was found to have a positive correlation of 0.909 (p=0.0001). Seventy out of eighty-one eyes (86.4%) had IOP difference within±3mmHg. Figs. 1 and 2 show fair agreement between the two instruments at lower IOP range but poorer agreement at high IOP ranges.
IOP (three readings+mean) in the study participants.
| Tonometers | IOP 1 (mmHg) | IOP 2 (mmHg) | IOP 3 (mmHg) | Mean IOP |
| IOP (Pulsair NCT) | 15.78±4.15 | 15.82±4.16 | 15.77±3.98 | 15.79±4.07 |
| IOP (GAT) | 17.02±4.24 | 16.83±4.22 | 17.12±4.42 | 17.02±4.23 |
| p-Value (2 tailed) | 0.061 | 0.128 | 0.044 | 0.062 |
IOP, intraocular pressure; NCT, noncontact tonometer; GAT, Goldmann applanation tonometer.
GAT is the gold standard tonometer for IOP measurements but associated problems are attachment with slit lamp, need for a skilled examiner, and portability of the instrument.34,35 Moreover, GAT requires touching the cornea and staining with fluorescein. This touching of cornea raises the issue of sterilization and predisposes the eye to risk of infection,25–27 especially in early post operative period.22 There are other sources of error like thickness of mires, amount of fluorescein dye, inability to be used in young children and physically disabled persons who cannot be positioned properly on slit lamp.25,28–30 Although, Perkins tonometer is a hand held applanation tonometer, it has potential benefits of portability and non-requirement of slit lamp but it has same disadvantages of risk of transmission of infection, risk of corneal abrasion and need for a skilled examiner.34–38 Pulsair NCT is a portable fourth generation tonometer with a calibration range of 7–50mmHg and auto switching capability of 7–30/30–50mmHg.5,9,16–21 In this tonometer an air puff is directed towards cornea which gradually flattens the corneal surface. The moment of applanation is determined by an optical sensor which detects obliquely reflected light rays from the cornea when its surface is flat.2,16–18 A microcomputer present in the tonometer calculates the IOP from the known force and area and displays it in digital form. Pulsair NCT does not require touching the cornea and can be used safely in early post operative cases as the risk of infection is minimal.22 As it is a hand held instrument, therefore, it is very useful in children23 and in the persons who cannot sit properly on slit lamp.14,16 Moreover, any resident or healthcare personal can be trained to measure IOP with this device.4,5,13,16–18 A previous study conducted in Africa has also compared GAT with Keeler's NCT to determine if the instrument was accurate in Africans population. The study found the two tonometers were accurate in their population.6 The present study was conducted to compare the Keeler's Pulsair NCT with GAT in a subset of patients residing in North India so that the data can be interpolated for the normal individuals.
Our study included subjects between 40 years and 78 years of age. The BCVA in all patients was 20/20. The mean IOP was less with NCT than with GAT and it was found to be non statistically significant. The study done by Babalola et al. from Africa showed no significant difference between the two instruments.6 This could be due to racial differences as their subjects were Africans as in our study that was done on subjects with Indian origin. On contrary, the findings of Oguchi et al. suggested that the NCT consistently read higher reading.20 Another study also found similar findings.7 A study done by Yucell et al. showed that the Pulsair NCT records IOP lesser than GAT as seen in our study.8 In our study we have excluded the first reading from NCT which is generally high. Vernon et al. also confirmed in their study that first high IOP reading is not due to biological variation but due to factors involved in the measurements.5 So, we got the lower average IOP, as seen in other studies.32 Even the manufacturers have accepted this error and have recommended to exclude the first reading. Moreover, it is a known fact that if the readings of NCT are taken after GAT then it may demonstrate lower IOP readings, because applanation produces a delayed IOP reduction.14,23 So, in our study the Pulsair NCT was done before GAT to avoid this error of measurement.
Our data also highlighted that there were 86.4% of eyes having IOP variations within ±3mmHg. Study done by Moseley et al. showed that 71% of the patients had IOP variation within ±3m Hg.9 Babalola et al. found that 79% of patients were within ±3mmHg.6 The mean of the paired difference in IOP was lesser in IOP less than 18 than above that. These differences in IOP were more common at the higher IOP ranges than the IOP in lower teens. This indicated that in most of the patients the Keeler's Pulsair NCT measured IOP correctly if it was within normal range but one has to become cognisant if measured IOP is 18mmHg or above with Pulsair NCT. This observation has been seen in other studies also.6–8,13,20 This finding highlights one of the shortcomings in the use of Keeler's NCT. The study done by Moseley et al. also showed that at low IOP ranges the NCT tends to underestimate the readings whereas at high IOP ranges it tends to overestimate the IOP.9 Agreement between the instruments was fair in IOP ranges of low teens. But it was not reliable in the eyes with high IOP. Study done by Lawson Kopp et al. also showed that Pulsair NCT readings were lower for the values below 15mmHg whereas they were higher for the values above 15mmHg.21
Various studies report association between central corneal thickness and IOP measurements.10–13 It is also a known fact that IOP requires CCT correlation,6,10–13,31–33 and moreover NCT readings are more affected by variation in corneal thickness.38 Therefore, CCT was done in all the patients and these readings were adjusted to get a true IOP.1
The shortcomings of the present study were the immediate IOP testing by the GAT after Pulsair NCT. It might cause probe bias in the patients which is not known. There may be an error due to use of Proparacaine eye drops which might change corneal hydration. High refractive error especially astigmatism was taken into consideration but other parameters that can influence the results like corneal curvature, biomechanics and axial length were not considered.11,13,15,28,39,40 These might also have some bearing on the IOP measurements.
In conclusion, we can say that Keeler's Pulsair NCT is a fair tool for screening purposes in community practices as can be easily used by residents and health care personals. The reliability of the instrument decreases if IOP is in the range of higher teens.
Financial disclosureNone.
Conflicts of interestThe authors have no conflicts of interest to declare.